The authors’ experience in the medium term.
Introduction
According to the current scientific literature, a prosthetically-guided approach should be the first choice for implant placement, even in case of horizontal/vertical alveolar bone resorption. In the last decade, different reconstructive techniques were described with the aim of restoring bone volume.
Among the available techniques, the authors widely experienced and achieved very satisfactory clinical outcomes with the “Edentulous Ridge Expansion” (E.R.E.), introduced by Dr. Bruschi and Scipioni in 1994.
This technique relies upon the healing potential of the spongy bone, associated with the elevation of a partial thickness flap to preserve the periosteum. The intra-bony gap is initially filled by a blood clot that turns into osteoid tissue in about 40 days. After about 90-120 days, the extracellular matrix progressively mineralizes and the osteoblasts mature into osteocytes.
In this technique, the preservation of an optimal trophism of the bone is paramount, leaving a thickness of at least 1-1.5 mm to the buccal bone; an extensive periosteal blood supply is required as well. This approach limits the risk of fenestrations, dehiscences or necrosis of the buccal bone during implant insertion and healing.
The E.R.E. technique is suitable in case of knife-edge alveolar ridges with at least a height of 10 mm and a width of 4 mm. Its main drawback is the risk of fracture during the displacement of the buccal bone plate; therefore, its predictability is not absolute. Such risk can be limited using a partial thickness flap, in order to ensure a better cortical blood supply in case of fracture.
If, on the one hand, a partial thickness flap is advisable, on the other hand, periosteal preservation does not allow to associate bone regeneration techniques that may be required during surgery, especially when a prosthetically-guided implant positioning is aimed. For this purpose, in recent years, the authors have developed a modified split-crest technique associated to a contextual guided bone regeneration (GBR), in order to compensate any dehiscence and/or fenestration, minimize the marginal bone loss and fill the gap between bone and implant. This approach is particularly important in the esthetic zone, where the stability of the buccal bone is critical for the success.
In a systematic review of the literature (Donos et al., 2008), the survival rate of implants placed in sites augmented with the split-crest technique ranged from 86.2 % to 100% after 12 months to 5 years in different studies. The success rate of the split osteotomy, measured as the achievement of adequate ridge dimensions for placement of implants, varied from 87.5% to 97.8% from 18 to 20.4 months post-loading, respectively.
The present article aimed at analyzing the clinical factors influencing the reliability of the split-crest technique as well as discussing its limits and rationale by the presentation of two clinical cases.
The technique: rationale and anatomic considerations
Comparing an atrophic ridge with its normal anatomy in sagittal view (Fig. 1), it can be noted that the bone volume is evidently resorbed, particularly on the buccal side. Differences in bone resorption rates between the buccal and lingual aspects are due to the greater amount of bundle-bone present on the buccal side of the alveolar ridge. The bundle-bone is strictly related to the presence of teeth, so a greater resorption rate occurs on the buccal aspect after tooth loss (Araujo & Lindhe 2005).
Frequently, in edentulous ridges an hourglass shaped alveolar process is found, due to the presence of an undercut at the base of the ridge. This anatomical peculiarity should not be underestimated in case of implants in the esthetic zone, as the drills can create fenestrations in the apical part of the implant site. Small fenestrations are not a big issue for osseointegration but can affect the achievement of optimal soft tissues esthetics, resulting in a grayish tissue transparency, particularly unpleasant in the anterior maxilla.
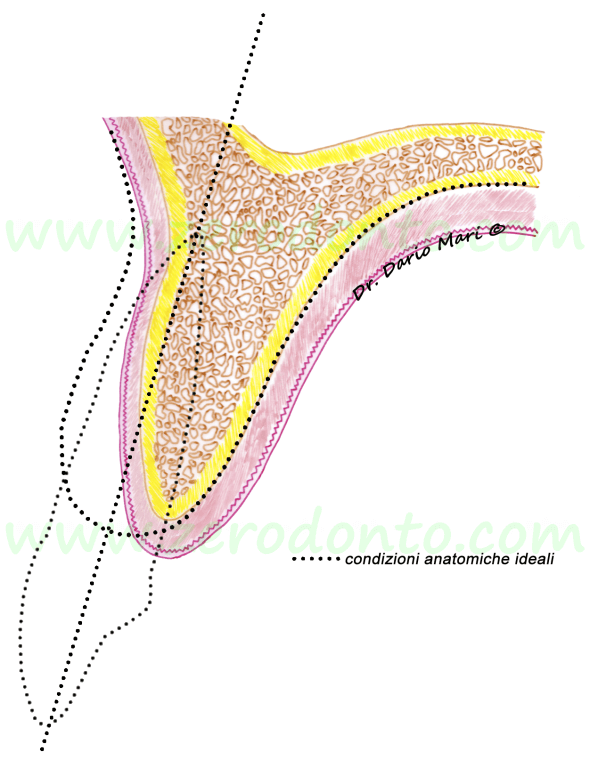
Fig.1
In order to place an implant according to the axis of the adjacent teeth (dotted line), an alveolar ridge expansion is required. If the implant (in red) would be placed just into the available bone volume in a surgically-guided position, it would be placed too palatally compared to the adjacent teeth. Consequently, it would result in an incongruous emergence profile (“ridge-lap”), more difficult to be cleaned correctly.
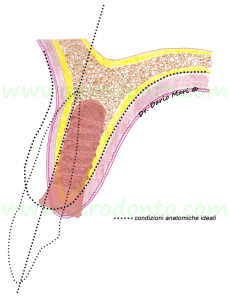
Fig.2
The same concept is evident in the occlusal view as well (fig. 3): if regerative procedures would not be performed, the implant would be positioned too palatally with respect to the ideal dental arch outlined by the other teeth. Moreover, this would result in a crown surplomb, unsuitable for the hygienic maintenance as well as for the functional and esthetic outcomes.
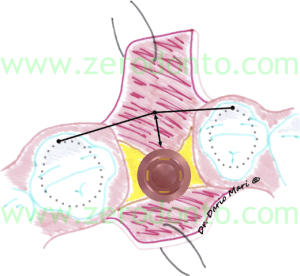
Fig.3
Even in unfavourable anatomic conditions, a clinician should try to place prosthetically-guided implants. In the anatomic conditions showed in the picture (fig.4), a correct implant placement (in green) would require bone regeneration procedures.

Fig.4
Regenerative and reconstructive techniques can restore proper bone volume, thus placing implants along the ideal arch outline.
In particular, according to the concepts expressed by Buser et al. (1998) and validated by the 3rd ITI (International Team for Implantology) Consensus Conference in 2004, it is worth remembering that the buccal aspect of the implant neck should be placed at 1-2 mm from the tangent passing through the buccal surfaces of the adjacent teeth (Fig. 5). Clinically, this can be easily checked with a periodontal probe leaning on the adjacent teeth.
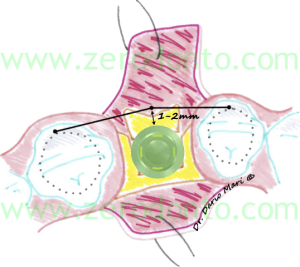
Fig.5
The importance of a proper implant insertion axis must be kept in mind during all the surgical phases, from the flap design to the bone osteotomy with chisels or sonic handpieces (fig. 6). It is paramount that the bone horizontal osteotomy (in green) should be made considering the correct implant axis, as the inclination of the palatal bone plate will not vary during the subsequent surgical steps and will guide the orientation of the drills.
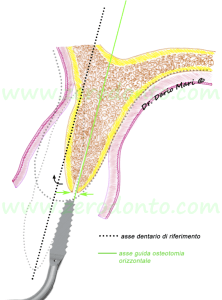
Fig.6
In order to ensure a proper bone trophism, the buccal bone should have a thickness of at least 1.5-2 mm. Therefore, the horizontal osteotomy of the ridge has to be made where it is estimated that the palatal surface of the implant will be (fig. 7). From a clinical point of view, with respect to the minimum thickness of the buccal cortical bone, this position can be identified approximately as follows:
-
identification of the tangent contacting the cervical profile of the adjacent teeth;
-
measurement of 2 mm in the palatal direction (safety zone);
-
measurement of the implant diameter with a periodontal probe.
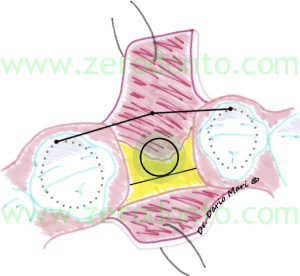
Fig.7
In figure 8, it can be noted that, once the buccal bone is gently displaced, the buccal margin (red arrow) is located at a more apical level compared to the palatal margin (green arrow) , because of a geometric rotation. This could lead to a limited exposure of the buccal part of the fixture.
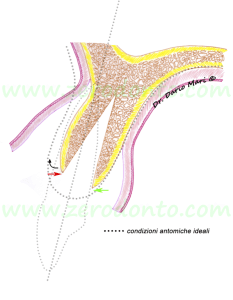
Fig.8
Furthermore, according to the bone configuration obtained after the displacement of the buccal plate, it would lead to an incorrect implant placement (red line), resulting in an angular discrepancy compared to the axes of the adjacent teeth (in green), which are parallel to osteotomy vector (fig. 9).
Most authors agree in considering that the major limitation of the split-crest technique regards the absolute impossibility to modify the buccal-palatal angulation of implant insertion, as the fixture has to be placed along the bisector between the buccal and palatal cortices. Therefore, when the alveolar ridge is not sufficiently thick and strongly angulated buccally, the split-crest technique may jeopardize the correct implant positioning with respect to angulation. In such conditions, a GBR technique is more predictable to restore bone volume and place implants according to a prosthetically-guided axis.
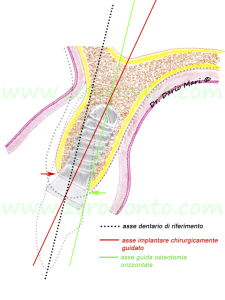
Fig.9
Currently, dental implant manufacturers produce angulated abutments to make a prosthetic correction of any disadvantageous implant placement; however, from a biomechanical point of view, this option does not represent the first choice.
During the preparation of the implant site, the use of the last drill usually increases the risk of fenestrations (Fig. 10); this could happen during drilling or screwing the fixture as well (fig. 11); such an occurrence may even affect the stability of the buccal bone. This can be due to the fact that the split-crest expands the mid-coronal portion of the ridge while its most apical part maintains the original width (usually 4-4.5 mm in atrophic ridges). This is particularly important considering that the last drills of the surgical sequence have an average diameter ranging between 2.8 and 3.5 mm. Therefore, the use of dedicated sonic or ultrasonic tips for implant site preparation could be beneficial.
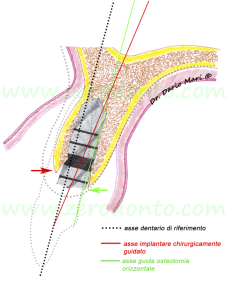
Fig.10
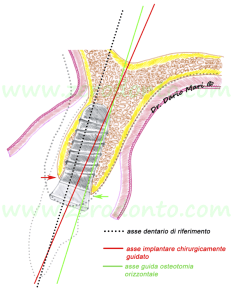
Fig.11
During implant screwing, it must be kept in mind that the implant neck may dislocate the insertion axis slightly buccally; this can be due to two main reasons:
-
being movable, the buccal bone offers no resistance to screwing;
-
when the implant neck impacts against it, the palatal bone is not susceptible to any movement, since it is joined to the ridge.
In order to avoid such drawbacks, at the end of the surgical sequence it is advisable to use the countersink drill exclusively on the palatal plate, thus avoiding any stress to the thin buccal bone. Some authors reported advantages using the tapered effect (TE) implants in case of split-crest surgery. Indeed, when screwing the fixture, the mid-coronal conical portion of such implants offers a gentle displacing movement of the buccal plate, completing the expansion and reducing the risk of bone fractures significantly.
For the above reported reasons, the authors are used to associate a contextual GBR to the split-crest technique, in order to compensate any dehiscences and/or fenestrations, minimize the marginal bone loss and fill the gap between bone and implant.
If the anatomical conditions would not ensure adequate bone thickness for a correct implant placement, a two-stage surgery is advisable, using the split-crest as support for a GBR procedure with membranes and bone grafts.
Many studies have been performed using barrier membranes and/or different bone graft materials in case of ridge splitting (Simion et al. 1992; Malchiodi et al. 1998; Vercellotti 2000; Koo et al. 2008; Ferrigno & Laureti 2005). In an interesting experimental study in dogs (Han JY et al. 2011) Bio-Oss, Bio-Oss collagen (Geistlich ®), autogenous bone chips and not grafted sites used after ridge splitting were compared, in combination with and without resorbable membranes (Geistlich Bio-Gide ®); the results showed that sites treated with Bio-Oss and Bio-Oss collagen obtained higher values of Bone to Implant Contact (BIC) and lower values of Marginal Bone Loss (MBL) compared to control sites at 2 and 3 months. Furthermore, the use of barrier membranes ensured better results in all groups.
In the present approach, the authors are used to use Bio-Oss and BioGide (fig. 12).
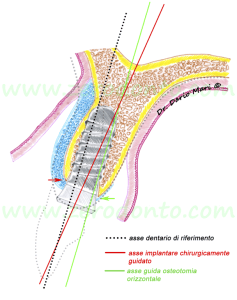
Fig.12
Two clinical cases are presented, in order to clarify the concepts illustrated in the figures.
Clinical case 1
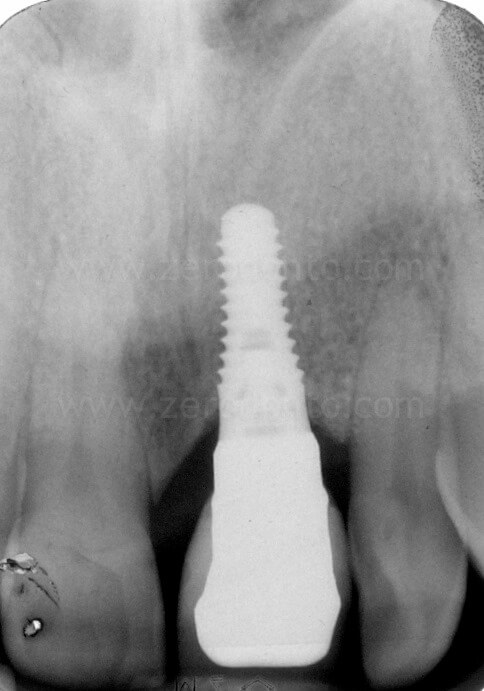
A 46 year-old male patient presented with missing 21 and a clinical history of severe adult chronic periodontitis.

The patient had previously been provided with a removable partial denture, unsatisfactory for both function and esthetics.

A severe horizontal and vertical bone atrophy was clinically and radiographically evidenced.




The patient asked for a fixed rehabilitation keeping an interincisal diastema, a feature that had always characterized his smile.
Despite the severe bone atrophy, the site could be treated with bone regenerative techniques and contextual implant placement.
After carefully evaluating the edentulous space, an implant placement was planned considering the mesio-distal diameter of 11 and the diastema.


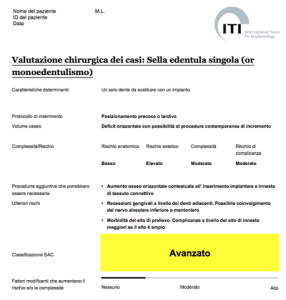
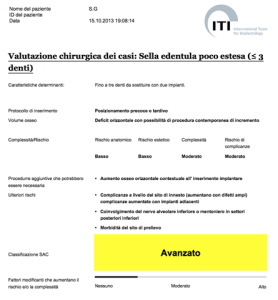
According to the ITI SAC (Straightforward, Advanced, Complex) classification, the case was considered of advanced complexity.
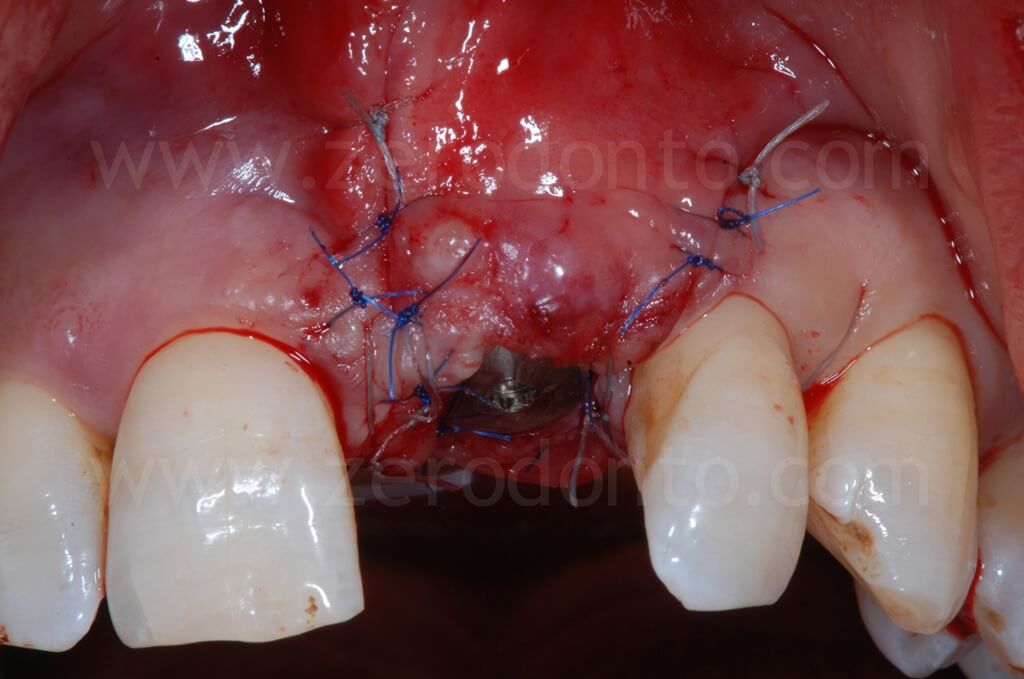
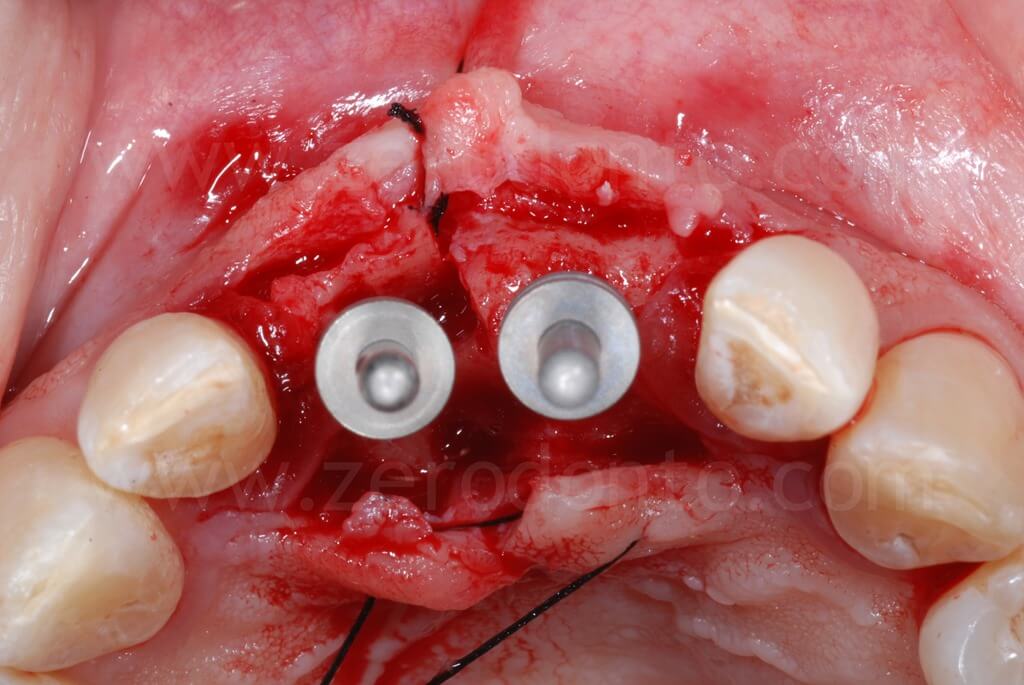
Surgical procedures
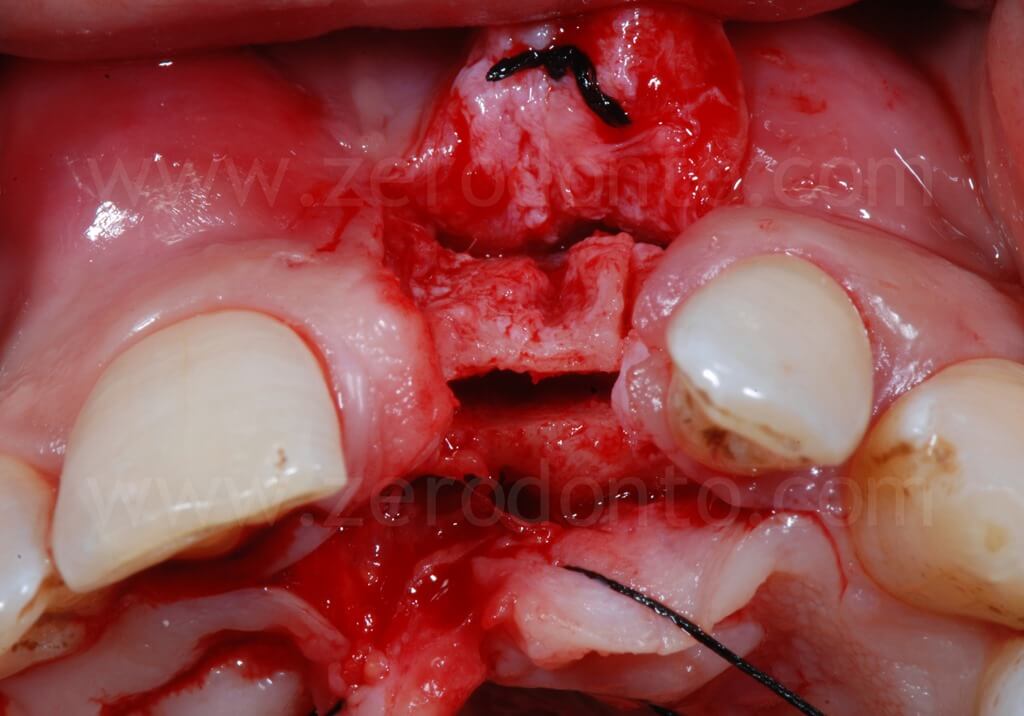
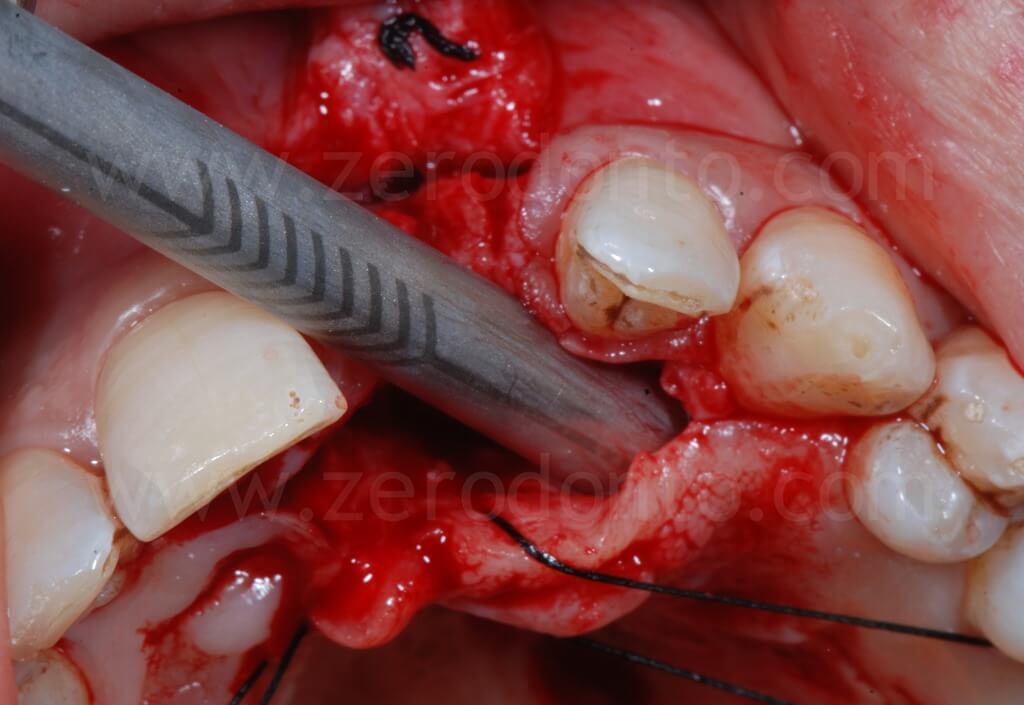
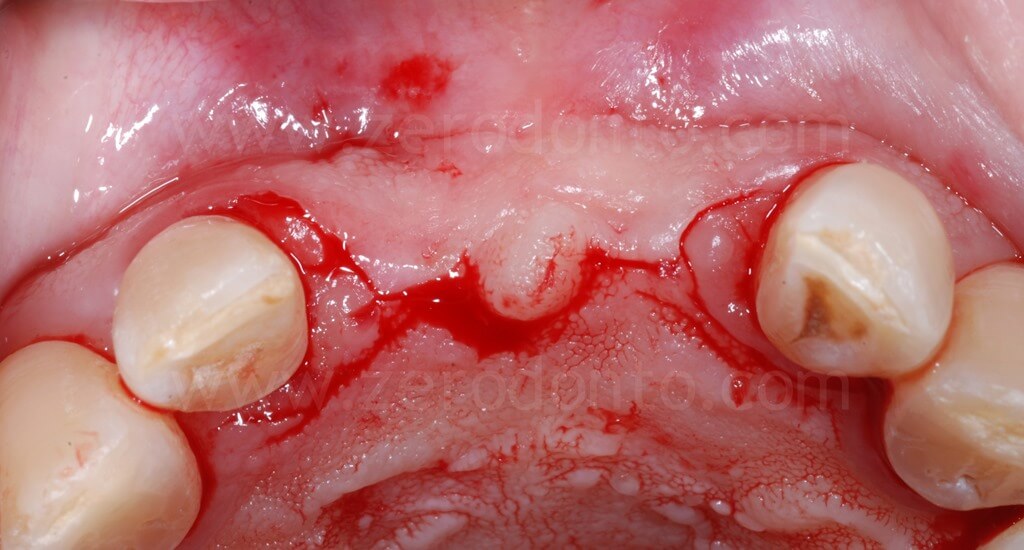
A paramarginal incision with two buccal releasing cuts was made, preserving the interdental papillae to reduce the risk of further gingival recession on the adjacent teeth; palatally, the incision was designed at the base of the papillae. In order to optimize the view and control of the surgical field, buccal and palatal divaricating sutures were made.

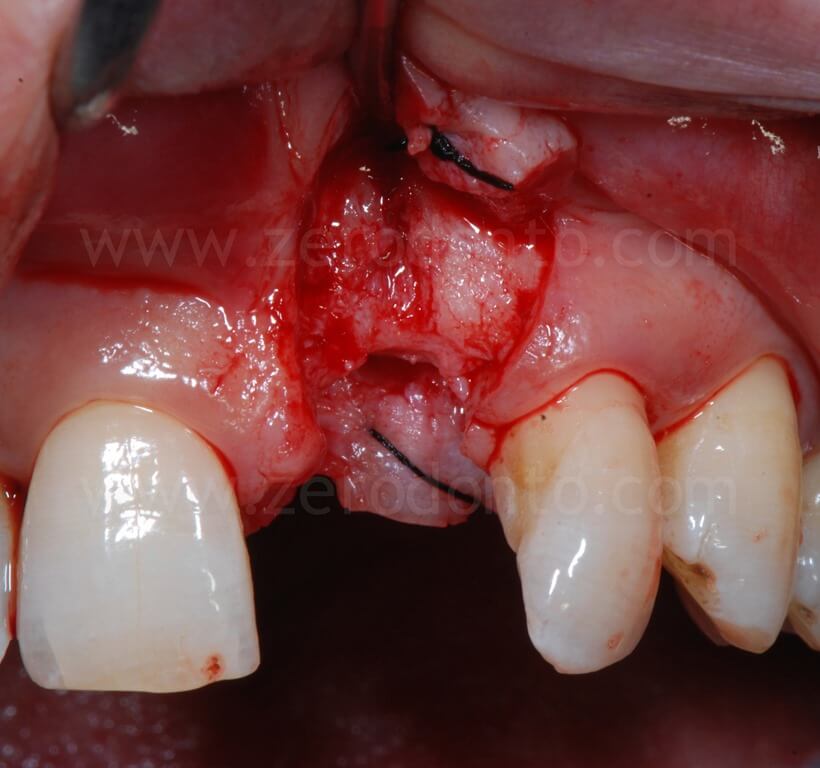
After the flap was elevated, the severe bone atrophy was confirmed; particularly, the loss of 21 had resulted in a severe resorption on the buccal aspect. In this situation, the implant platform without bone regenerations would have resulted to be too palatal and consequently unsuitable for a correct prosthesis, with the exception of a ridge-lap restoration. Nonetheless, as previously reported, a crown surplomb would not allow for a correct hygiene maintenance as well as for optimal functional and esthetic outcomes.
Accordingly, a controlled split-crest surgery associated with GBR was performed.
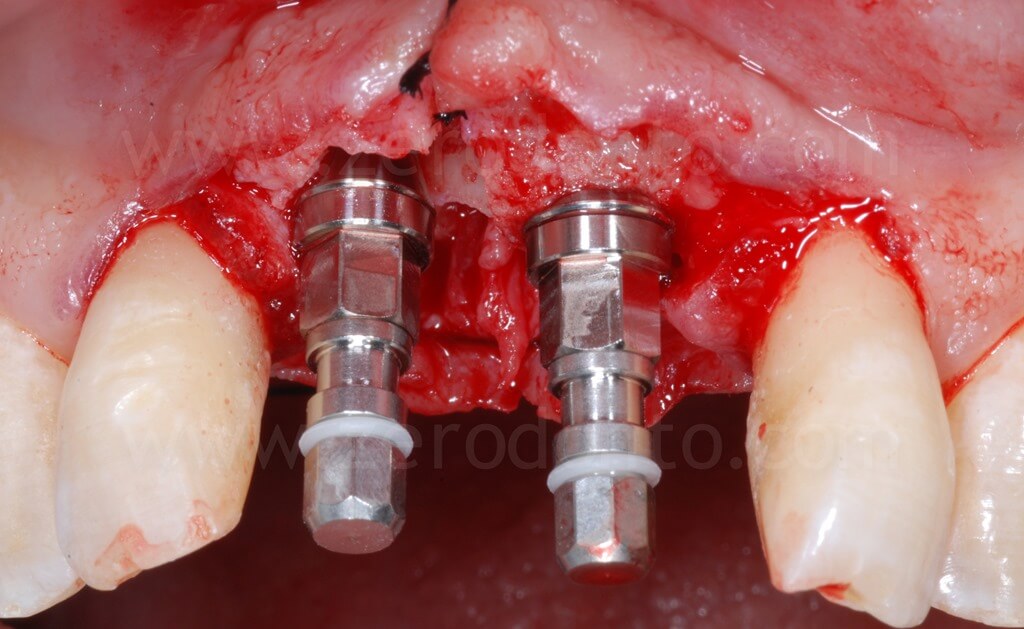
With a split-crest dedicated sonic tip mounted on a sonic handpiece, horizontal and vertical buccal osteotomies were performed. As previously described, the horizontal osteotomy has to be made where the position of the palatal surface of the implant will be; therefore, the tangent contacting the buccal cervical areas of the adjacent teeth and the fixture diameter have to be considered.

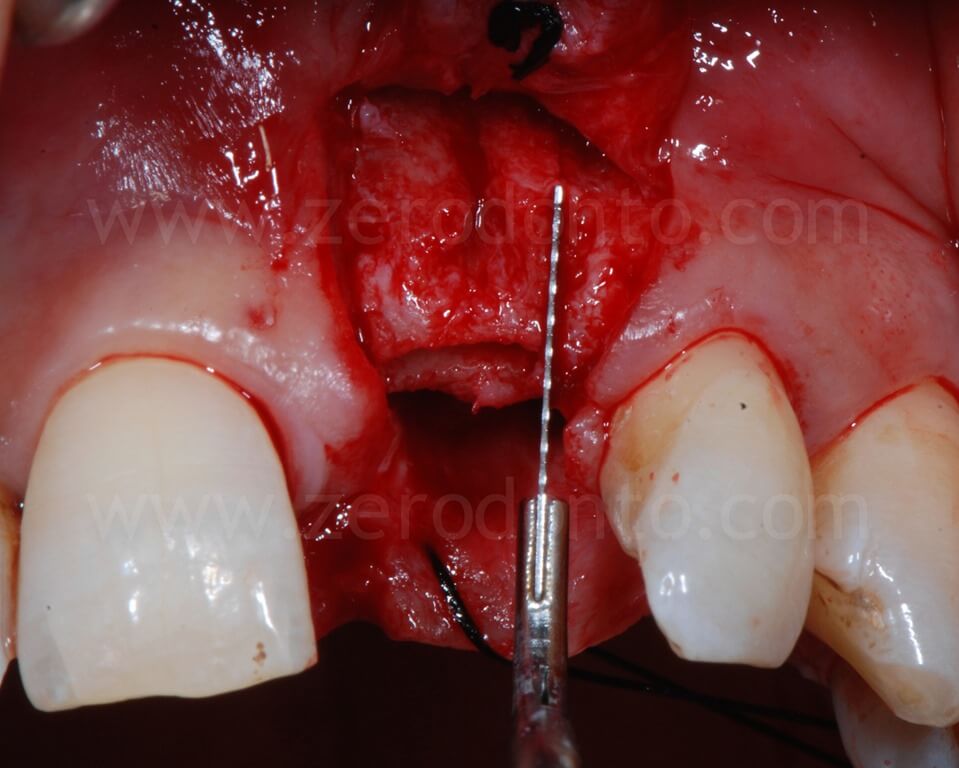
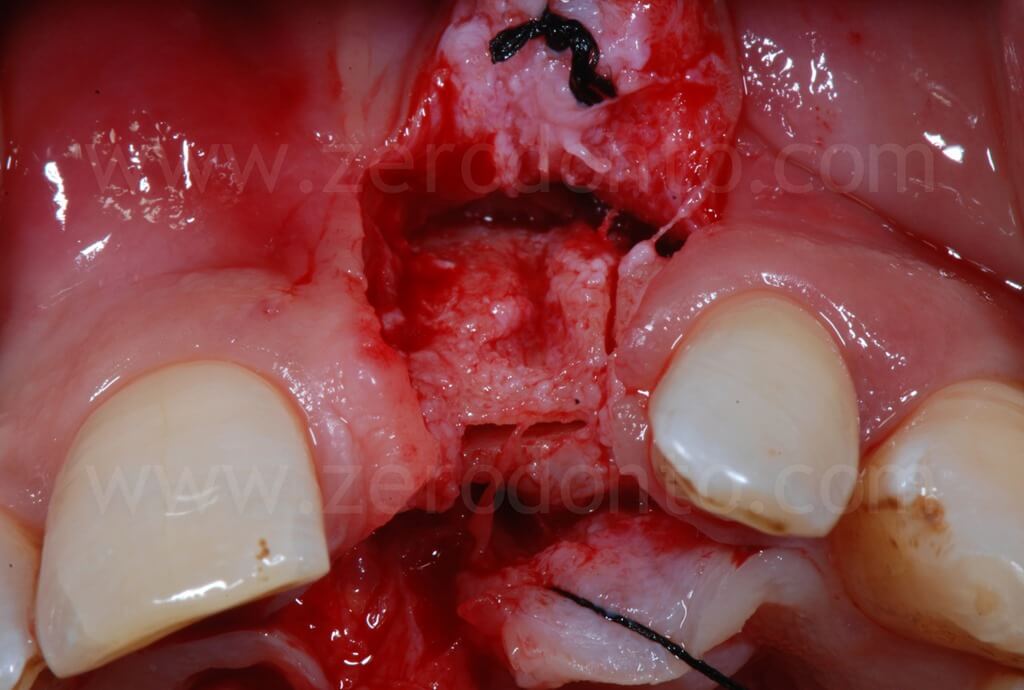

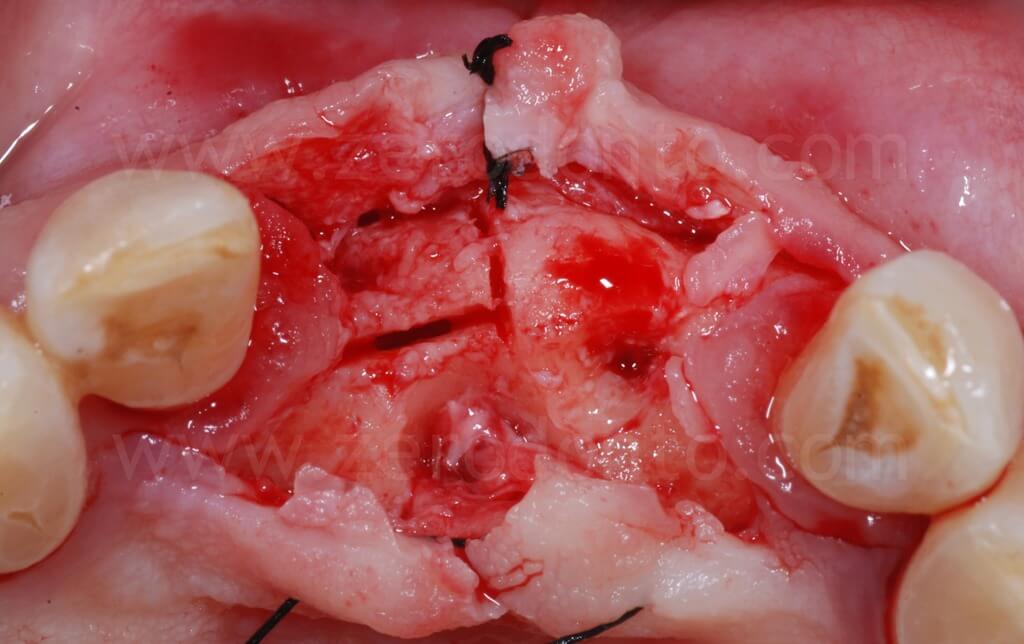
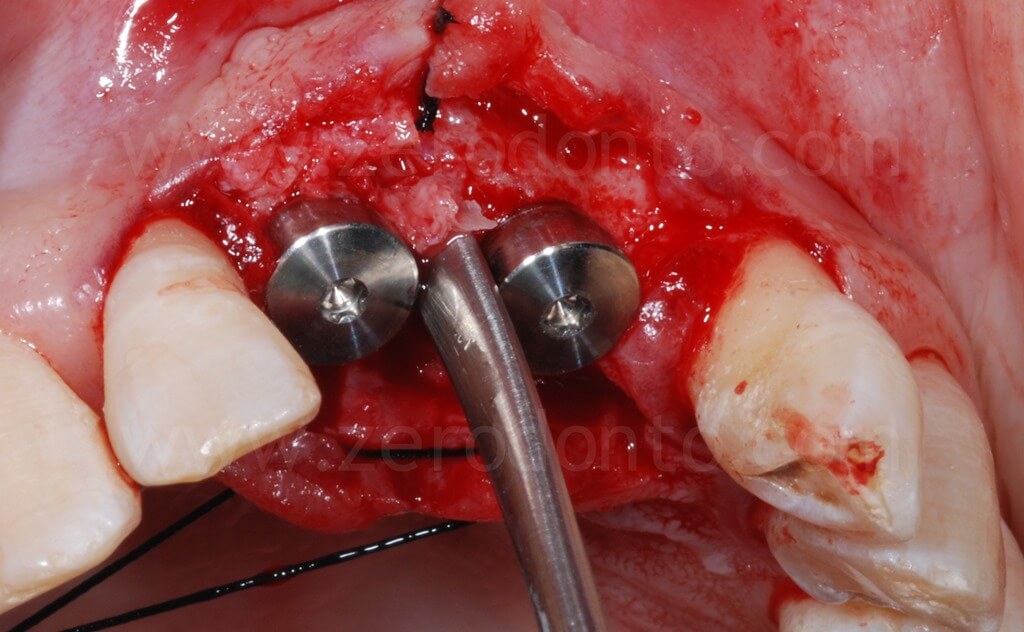
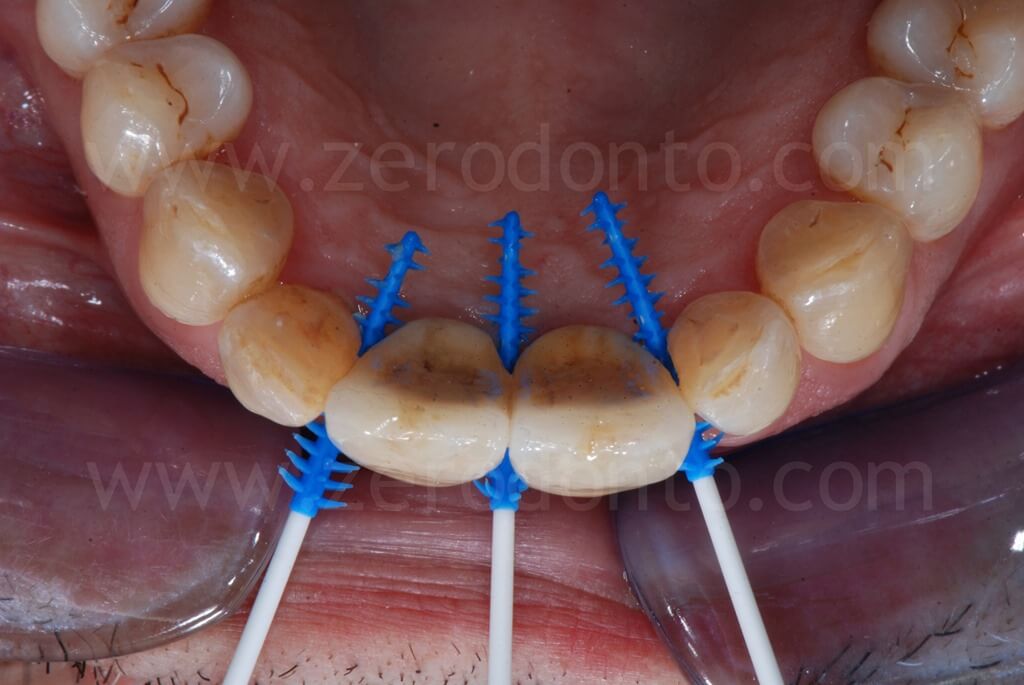
Then, a controlled bone augmentation with screw-type expanders with increasing diameters was performed. The expansion has to be done slowly and gently in multiple steps, so as to avoid any possible damage to the buccal bone. First, the expander is inserted up to reach a high torque. When a moderate bone resistance is encountered, the expansion is stopped for about 1 minute, allowing a delicate and atraumatic bone distraction. Subsequently, expanders of greater diameter are inserted and the previously steps are repeated until the desired expansion is achieved.
A final step with a drill or a dedicated sonic tip can correct any undesired fixture angulaion. Possible buccal fenestrations can be easily compensated with a GBR technique.
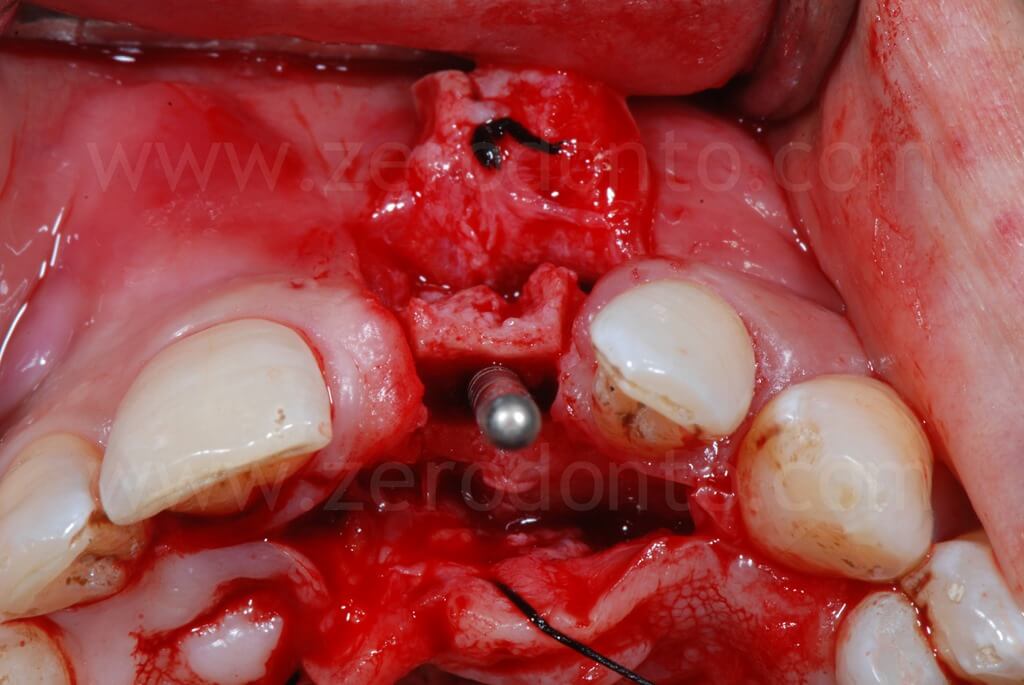


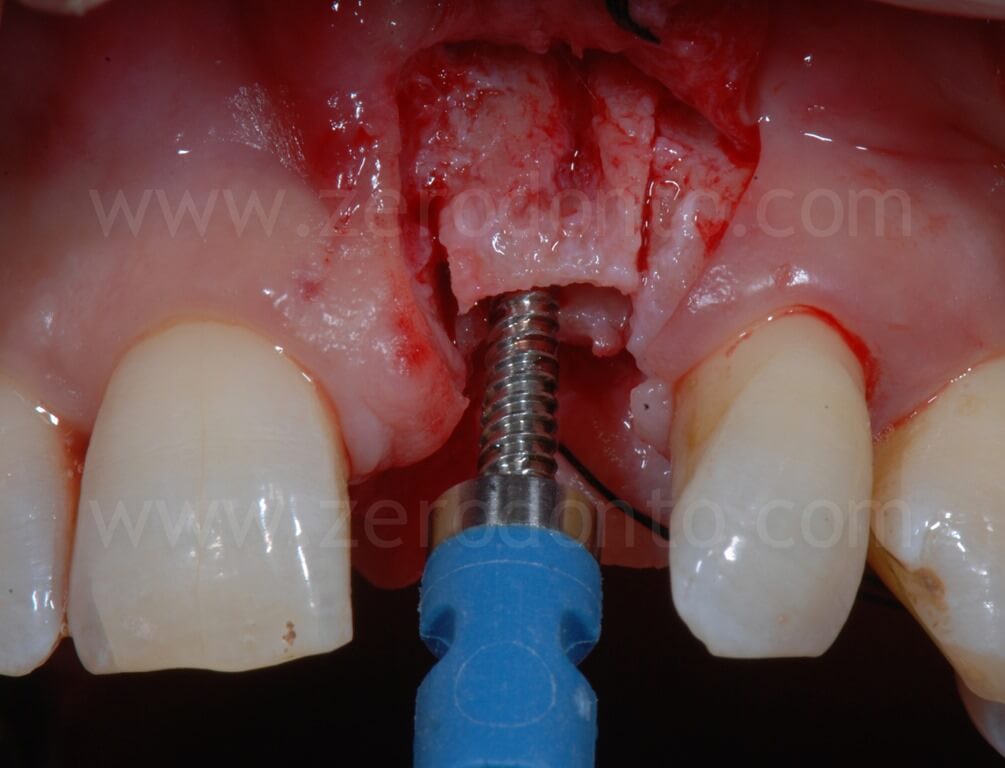
In the present case, a Straumann SLActive TE implant with diameter of 3.3 mm and length of 10 mm was used; therefore, a countersink drill was used to give a tapering shape to the coronal part of the implant site.


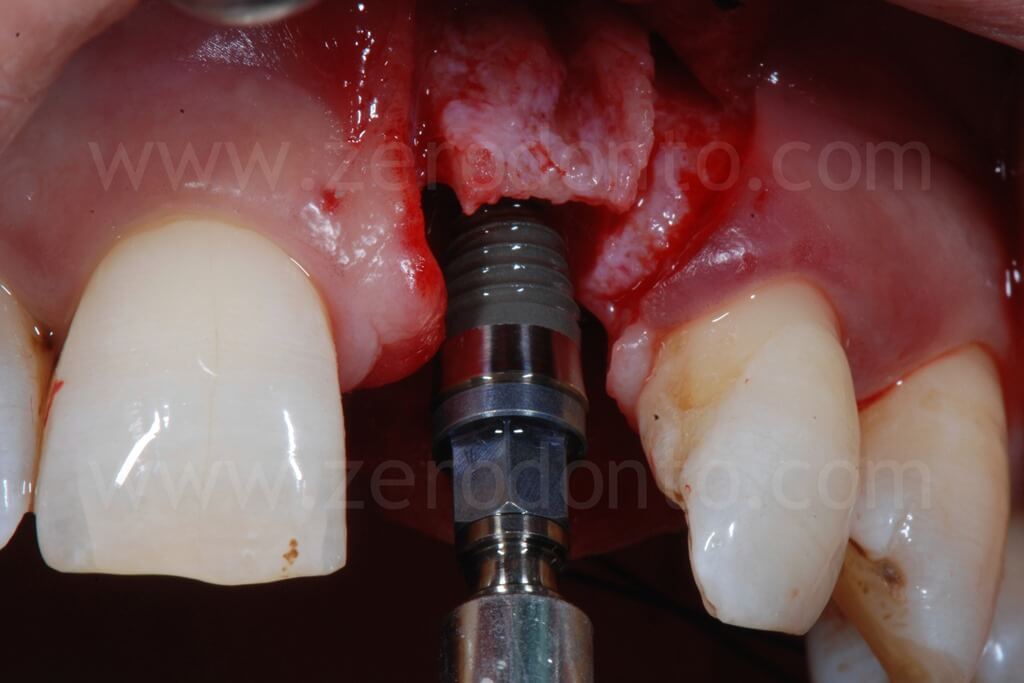
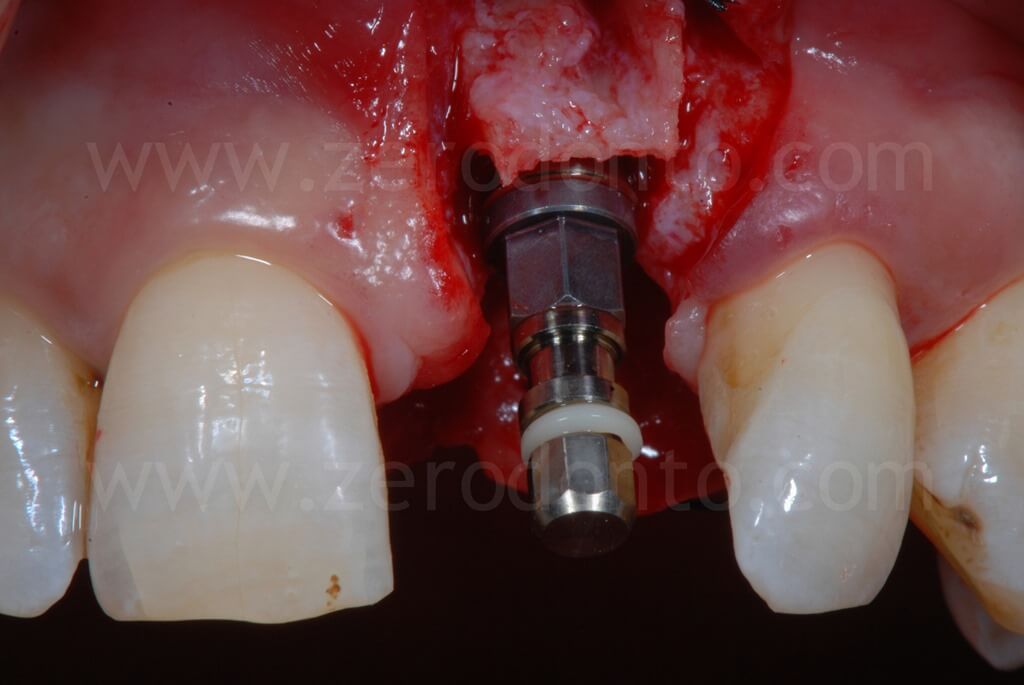
In the present case, a Straumann SLActive TE implant with diameter of 3.3 mm and length of 10 mm was used; therefore, a countersink drill was used to give a tapering shape to the coronal part of the implant site.

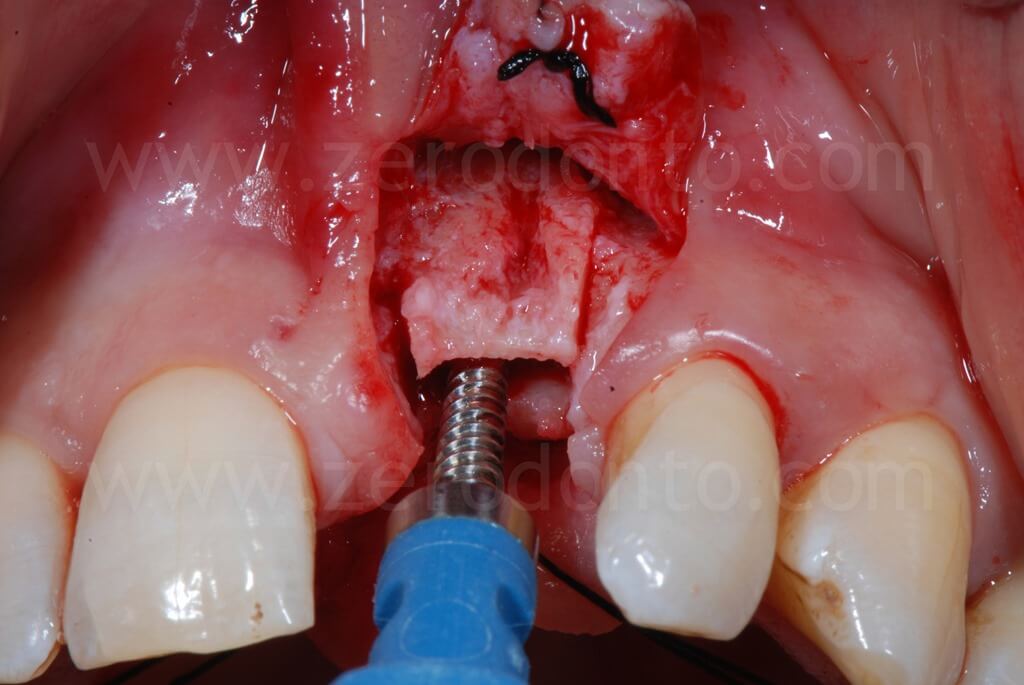
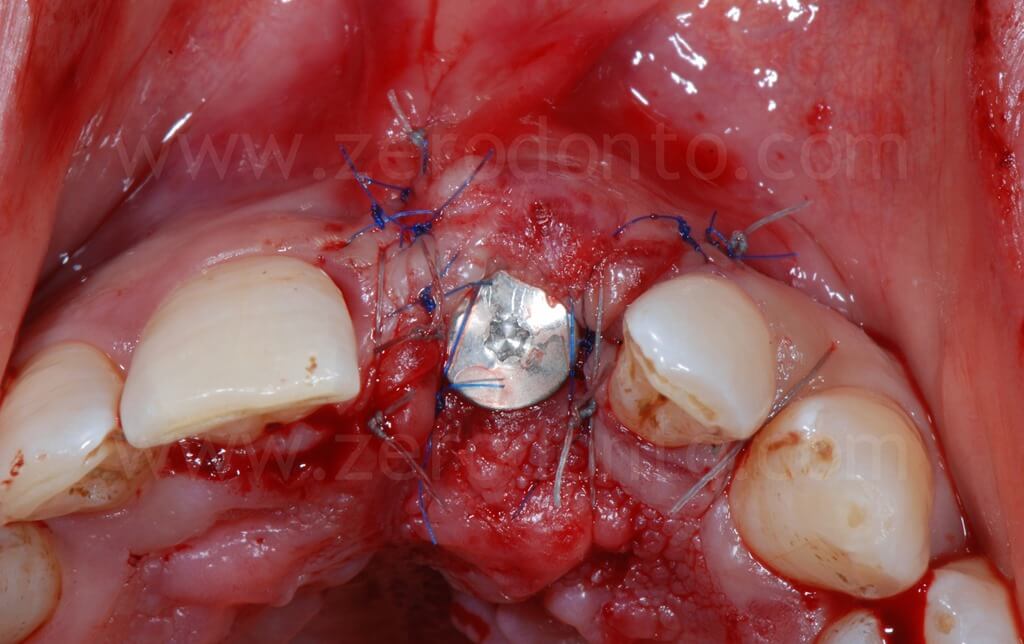
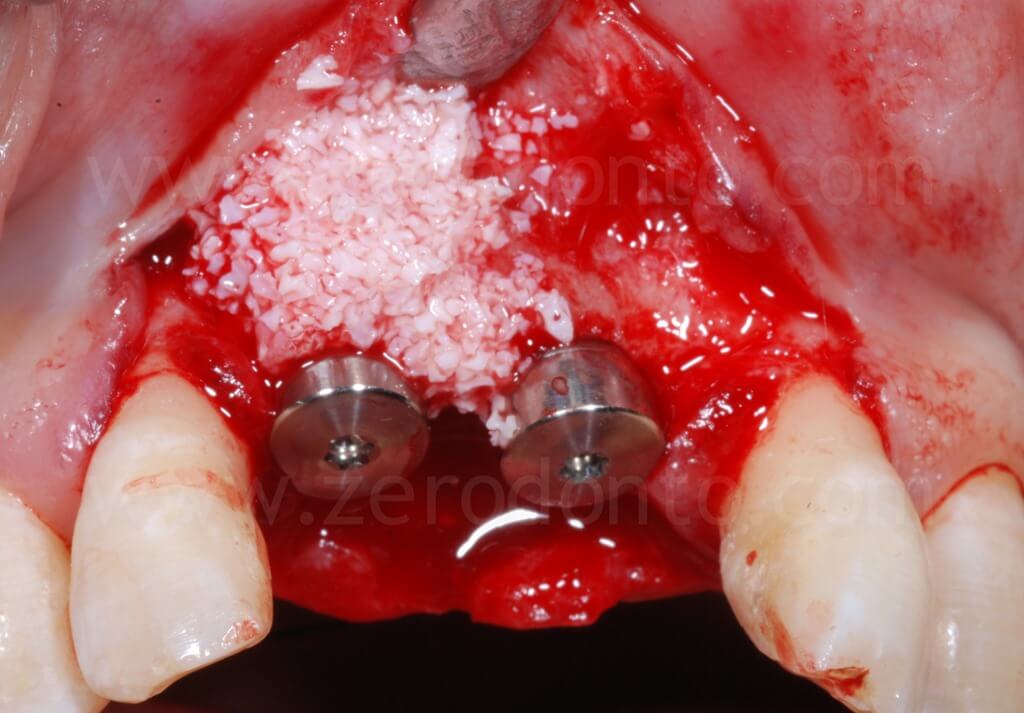
In order to preserve a greater buccal bone volume, to correct possible fenestrations and fill gaps between the bone and the implant surface, a GBR with a mixture of autogenous bone and Bio-Oss covered by a resorbable membrane (Bio-Gide) was performed. The sharp edges of the buccal bone were smoothed with a drill and a limited amount of autologous bone was collected by means of a bone scraper (Micross) from the palatal aspect of the ridge. The harvested bone was then mixed with Bio-Oss particles in a 1:1 ratio and placed into the defect.




Finally, Tevdek 3/0 and monothread polyamide 5/0 sutures were used for the proximal-crestal area and the release cuts respectively.
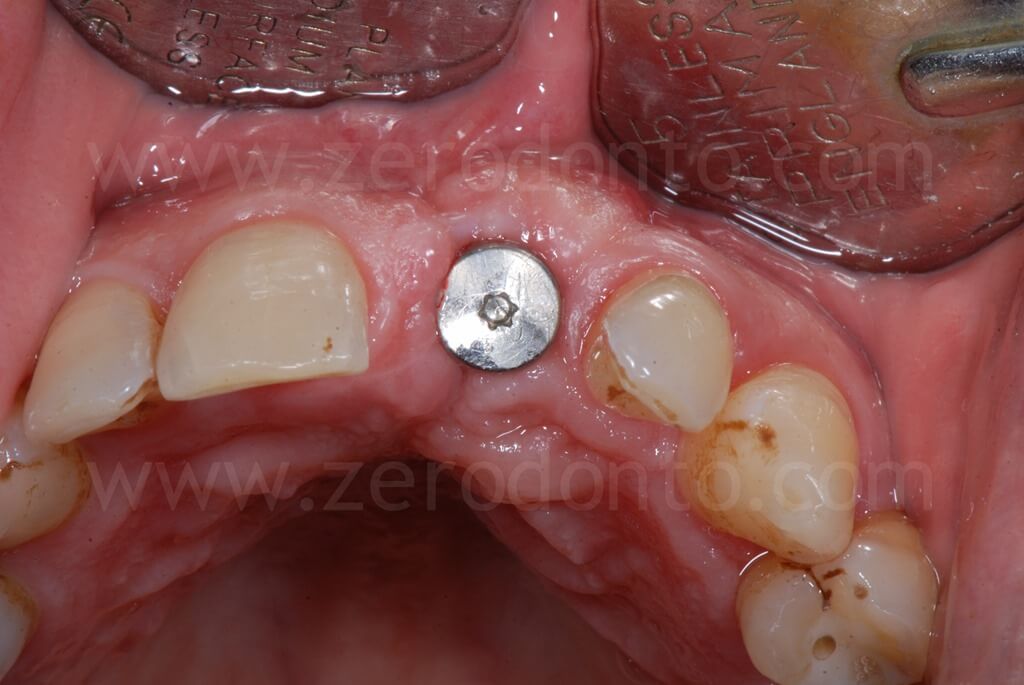

Ninety days after surgery, an impression with a screwed impression coping was taken to fabricate a screw-retained resin temporary crown. Such crown was modified intraorally about every 2 weeks in order to shape the transmucosal path and the peri-implant tissues.



The patient refused to close the interincisal diastema as proposed by the authors. A pre-visualization of the final result was made using a resin mock-up.



The restoration was finalized with a zirconia abutment and a cemented zirconia-ceramic crown.










4 years follow-up


Clinical case 2
A 55 year-old male patient presented with teeth missing 11 and 21.

The patient had been previously provided with a removable partial denture, unsatisfactory for both function and esthetics. The patient asked for a fixed prosthesis.


After a careful study of the case, an implant-supported prosthetic rehabilitation with 2 single crowns was planned.
The case was analyzed with the ITI SAC classification software tool and resulted of advanced complexity.
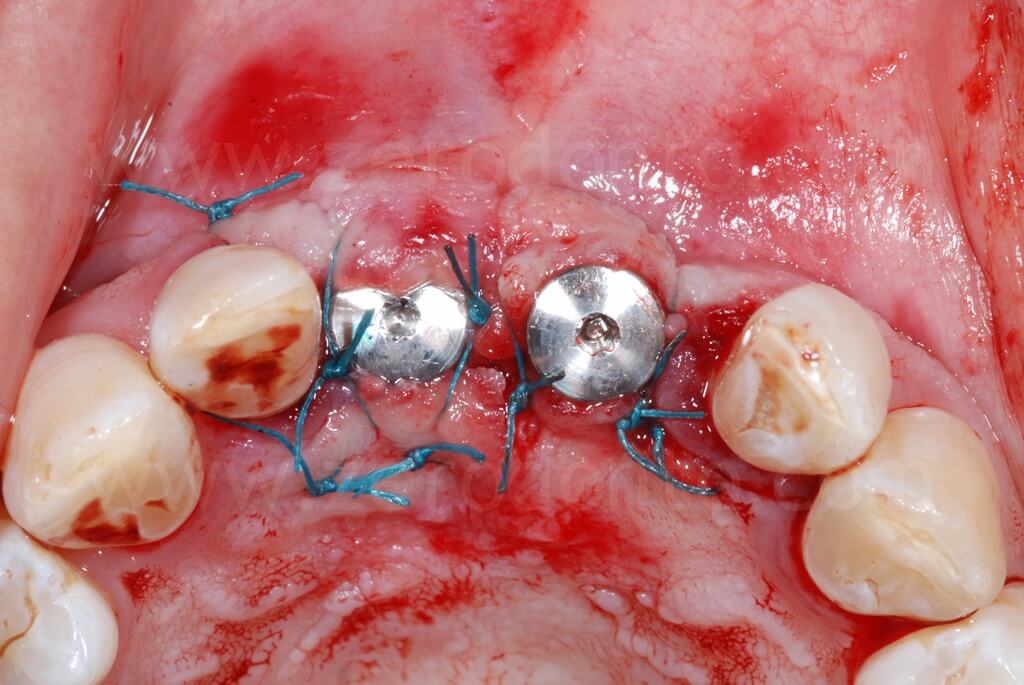
The design of the flap was performed preserving the papillae of the lateral incisors, in order to minimize any possible post-surgical soft tissue recession.
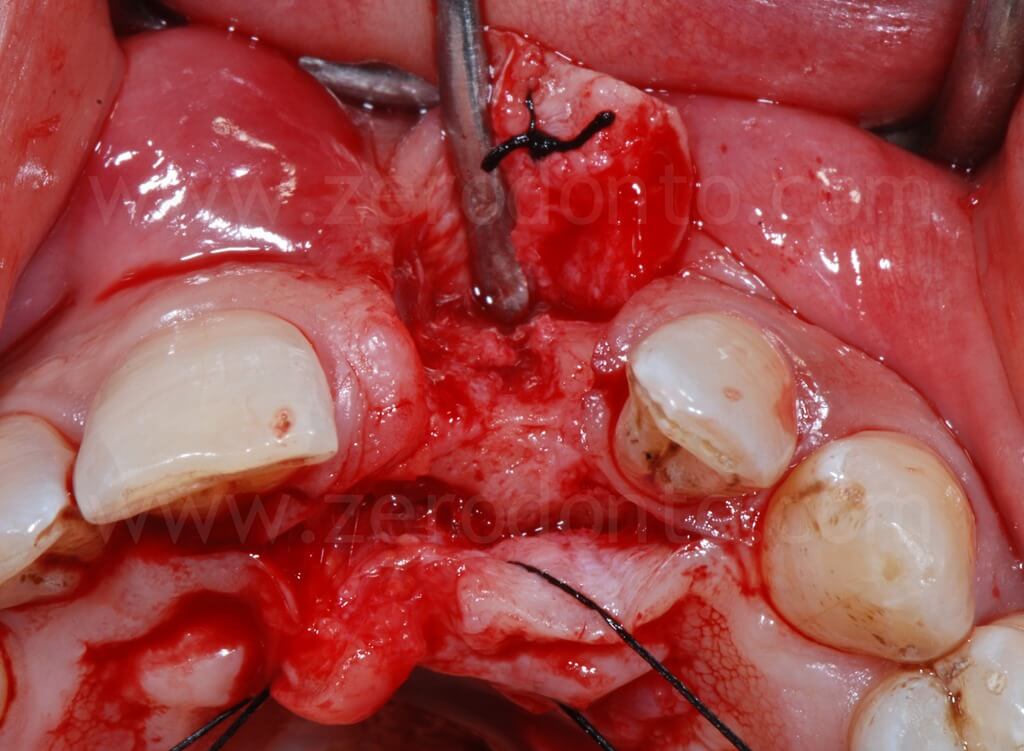
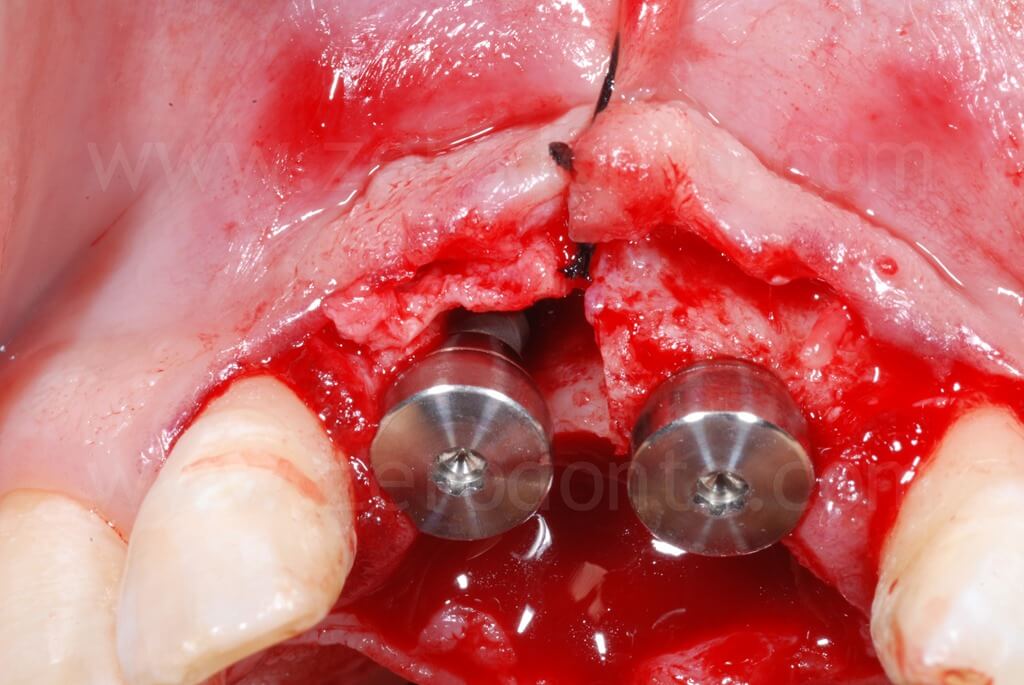
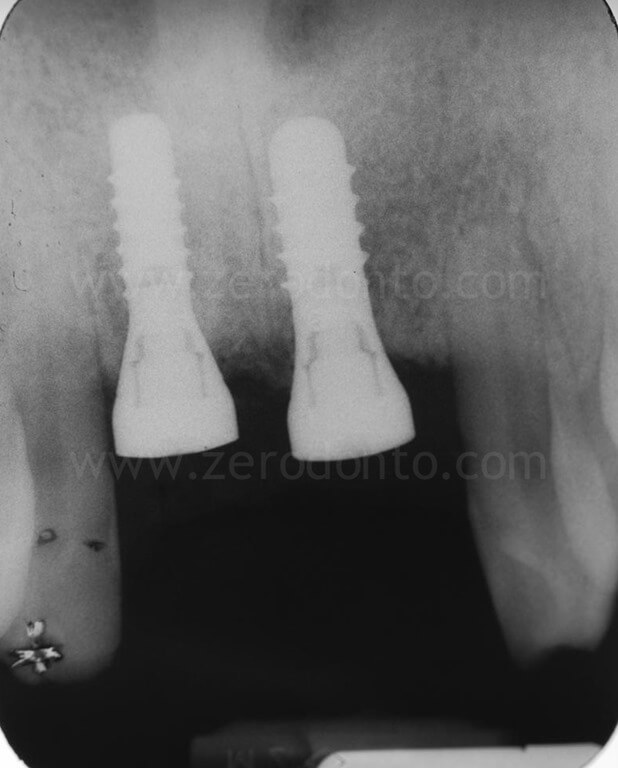
The alveolar bone showed a severe buccal horizontal defect in region 11, while the bone volumes in region 21 were considered sufficient.
Therefore, a split-crest in 11 area was performed, so as to harmonize the buccal aspect of the alveolar bone.
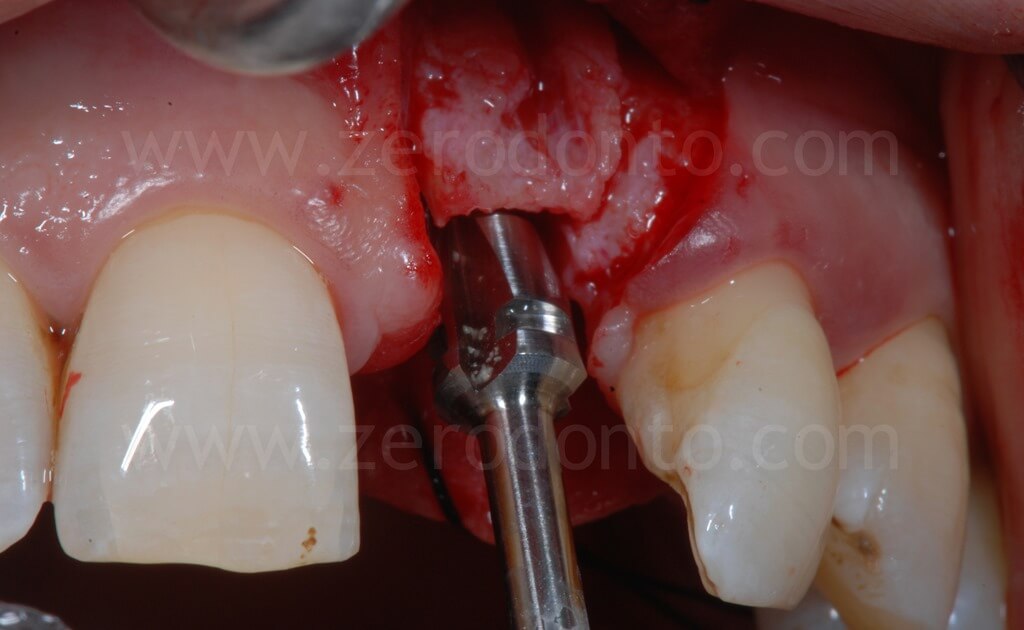
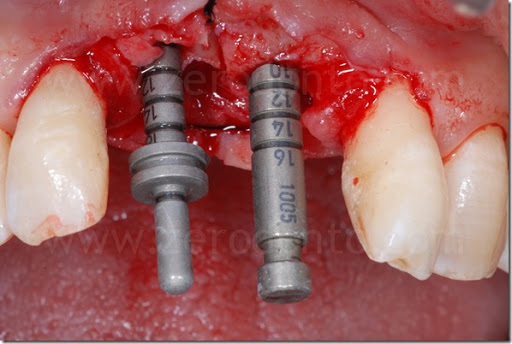
Horizontal and vertical buccal osteotomies were performed with a split-crest dedicated sonic tip mounted on a sonic handpiece.
As described above, a controlled bone augmentation was achieved by means of screw-type expanders with increasing diameters.
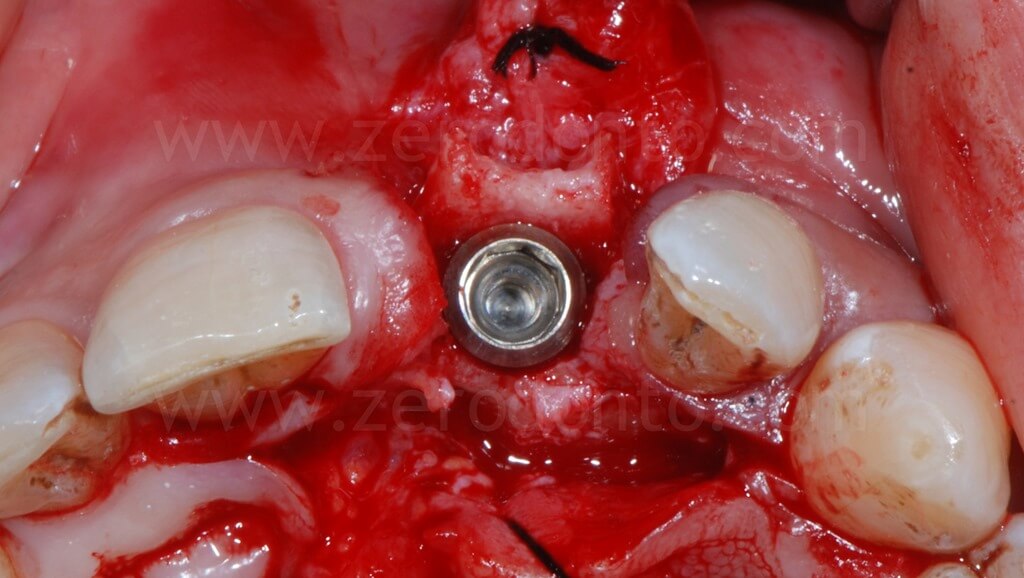
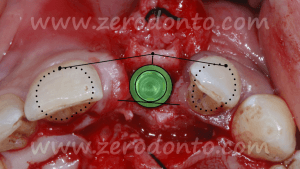
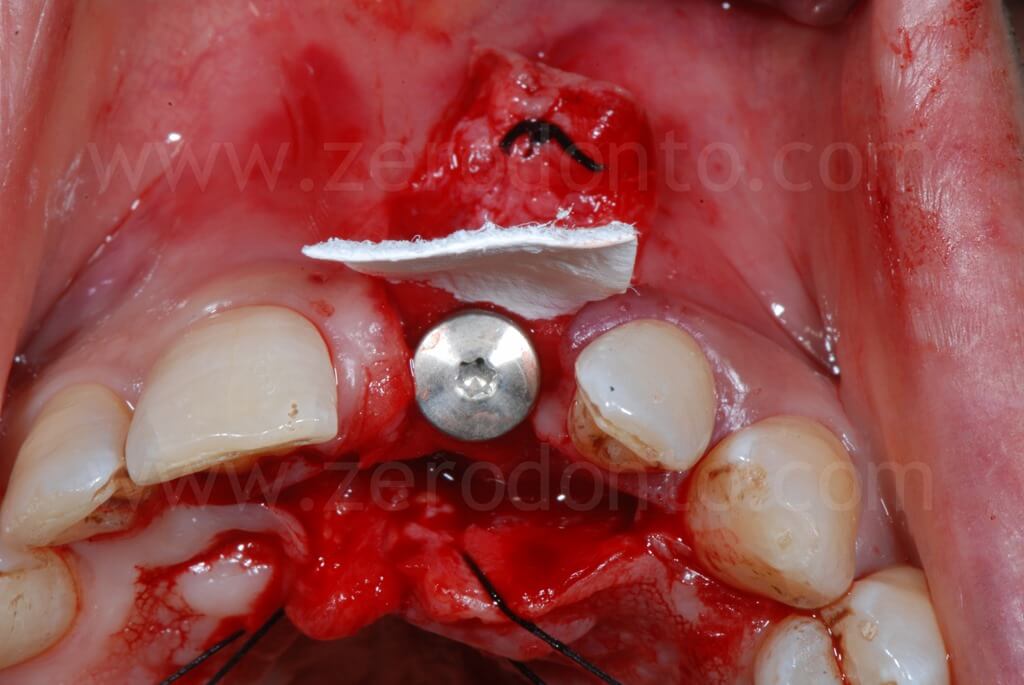
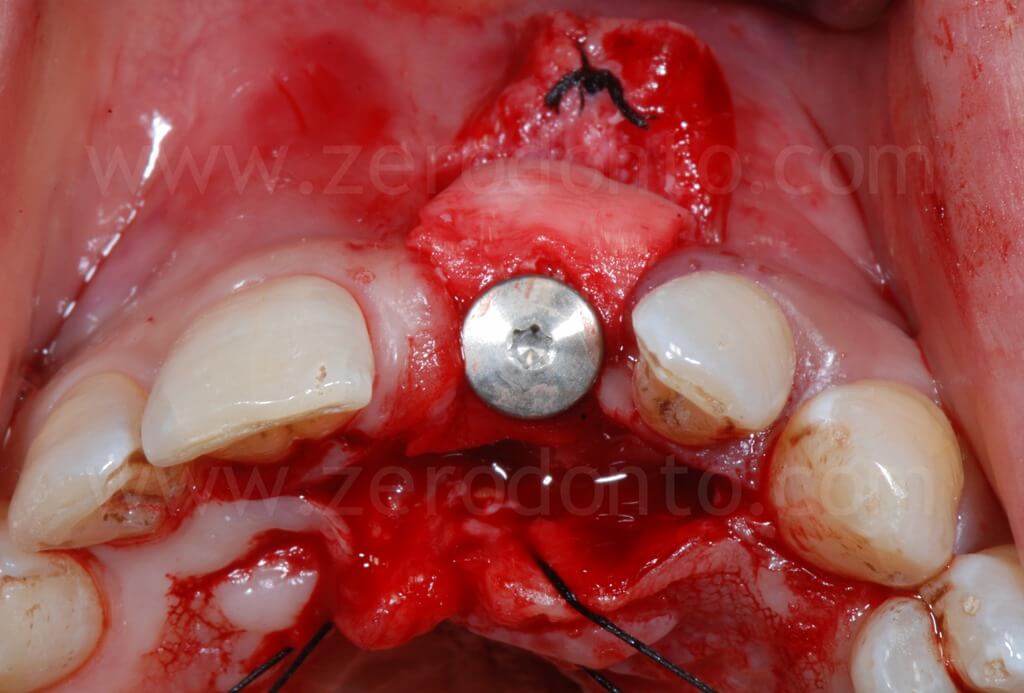
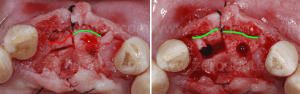
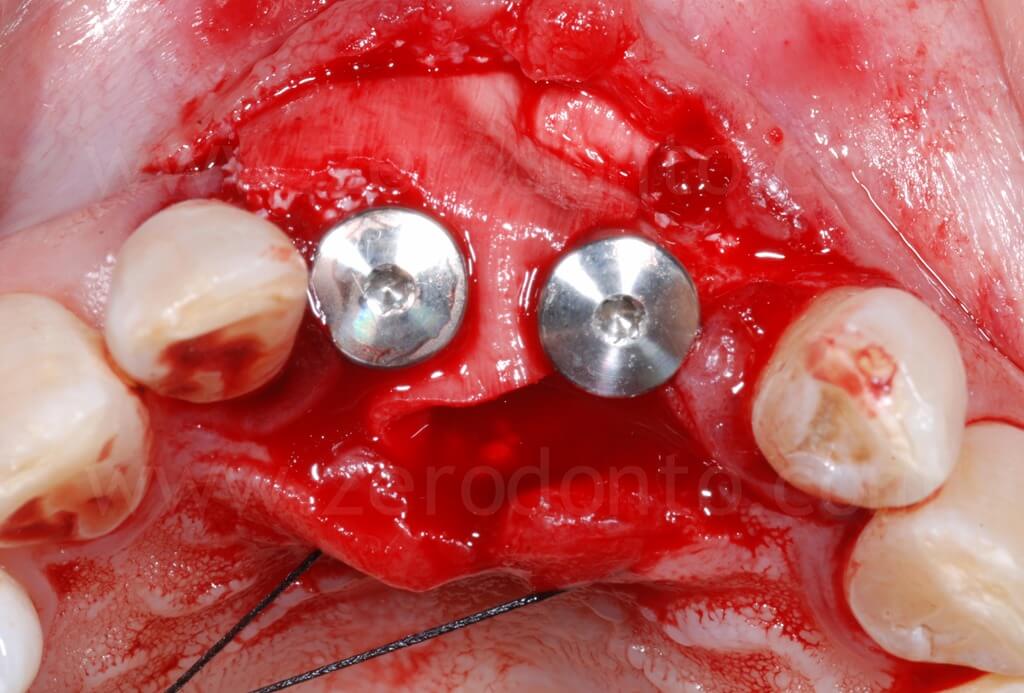
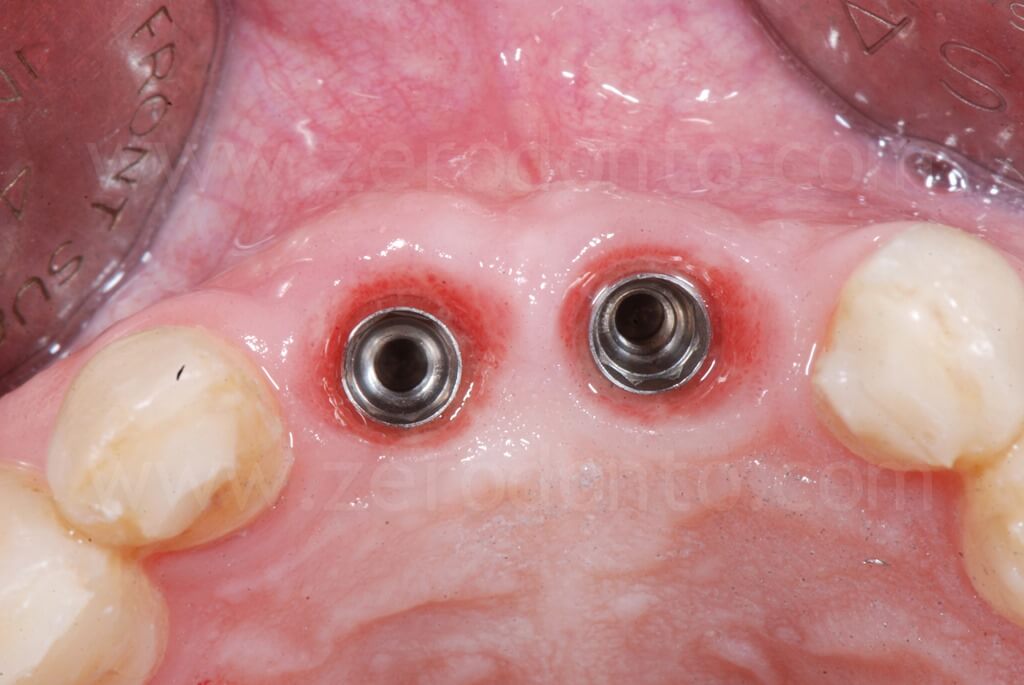
After the ridge expansion was completed, it was evident that the buccal edge in region 11 was at a more apical level than that in region 21. This was due to the rotation of the buccal bone during the split-crest: the buccal plate remains tied to the basal portion of the alveolar ridge, working as a fulcrum, while the free edge of the bone move along an arc. Therefore, the greater the expansion is, the more apical the buccal edge will be.
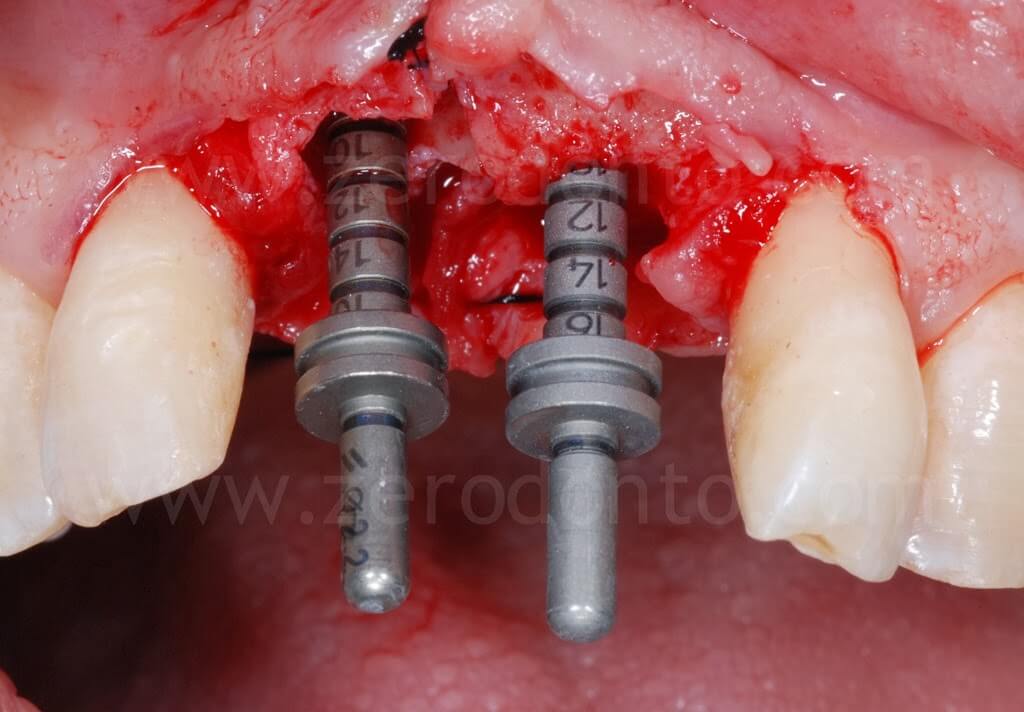
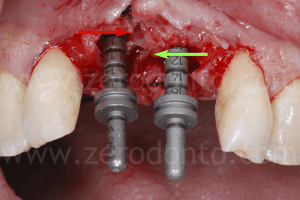

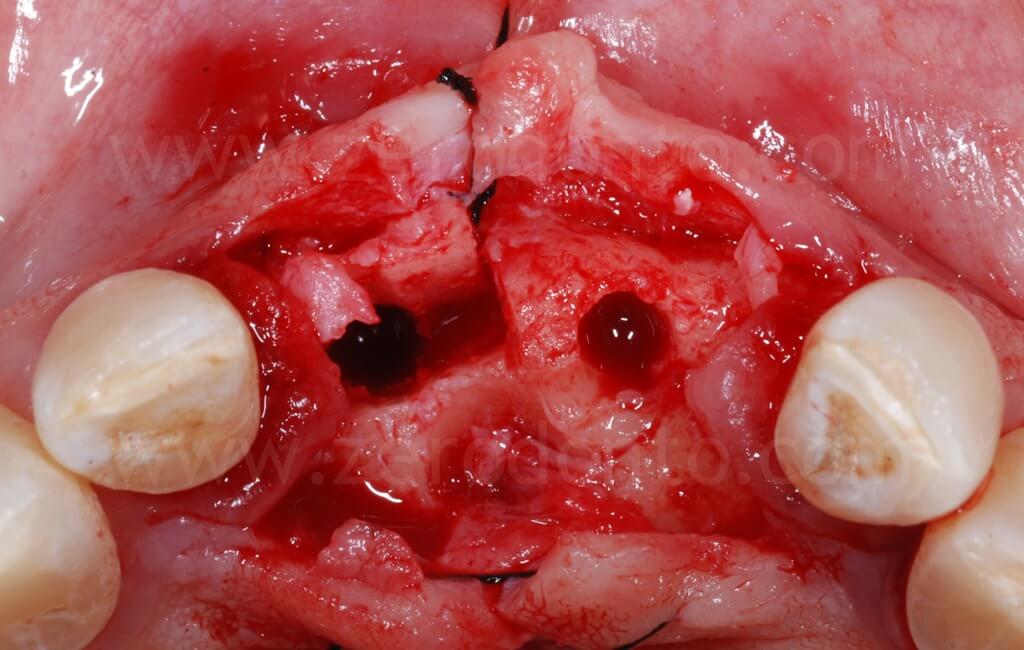
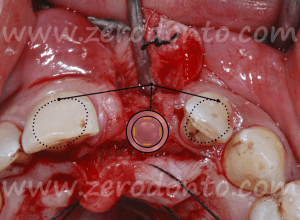
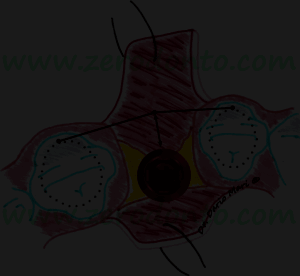
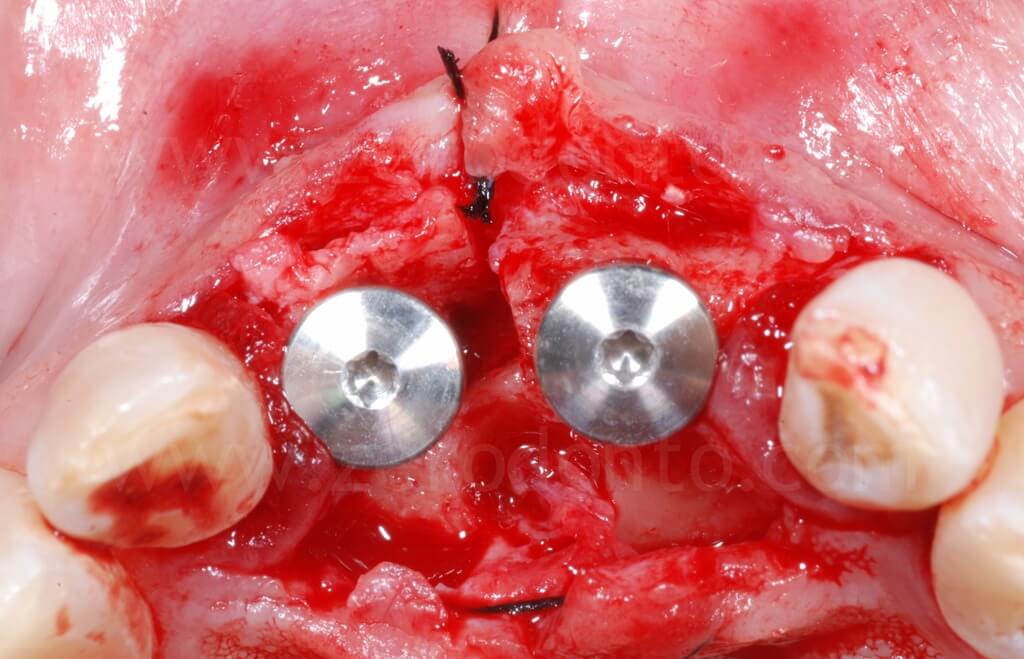
In occlusal view, it is evident that the alveolar ridge profile was regularized after the dislocation of the buccal bone.
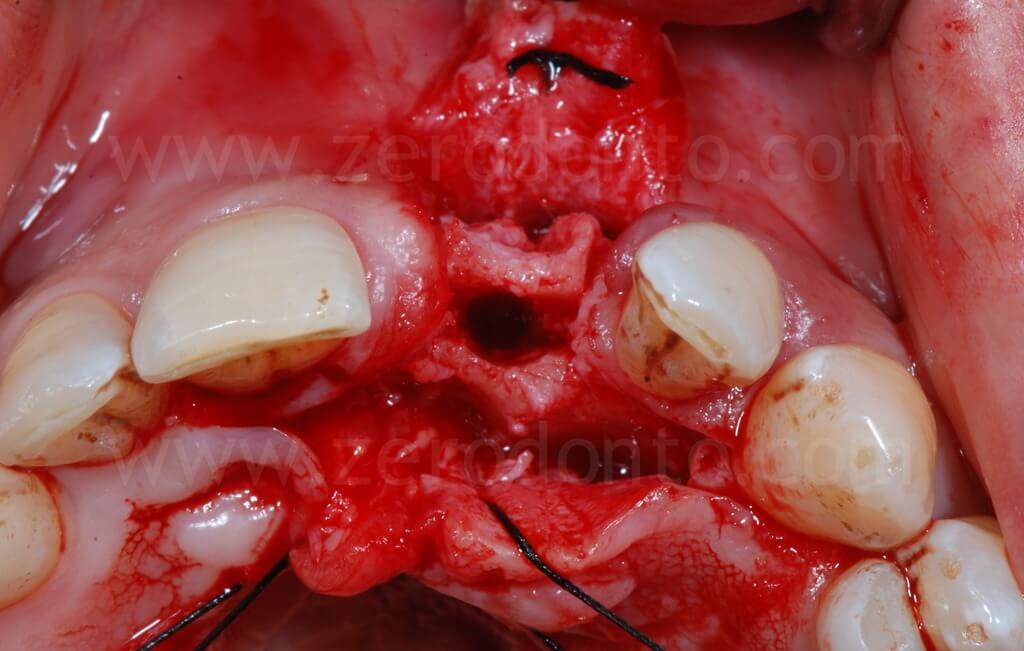
To optimize esthetics, the gap between the bone edges in region 11 and 21 was compensated by means of a GBR. As previously described, a mixture of autologous bone and Bio-Oss in a 1:1 ratio was placed above the displaced buccal plate and into the bone-to-implant gap with a resorbable membrane (Bio-Gide).
Two Straumann SLActive implants with diameter of 3.3 mm and 4.1 mm and length of 10 mm were used respectively in position 11 and 21. In comparison with the 4.1 mm TE fixture, the 3.3 mm Standard Plus implant allowed to achieve a more correct emergence profile and less bone removal at the apical part of the site.
The implants were placed centered considering the upper dental midline, then planning a further orthodontic alignment in order to optimize the prosthetic spaces; in particular, the space between crown 1.1 and 1.2 was considered too tight for a proper soft tissue management.
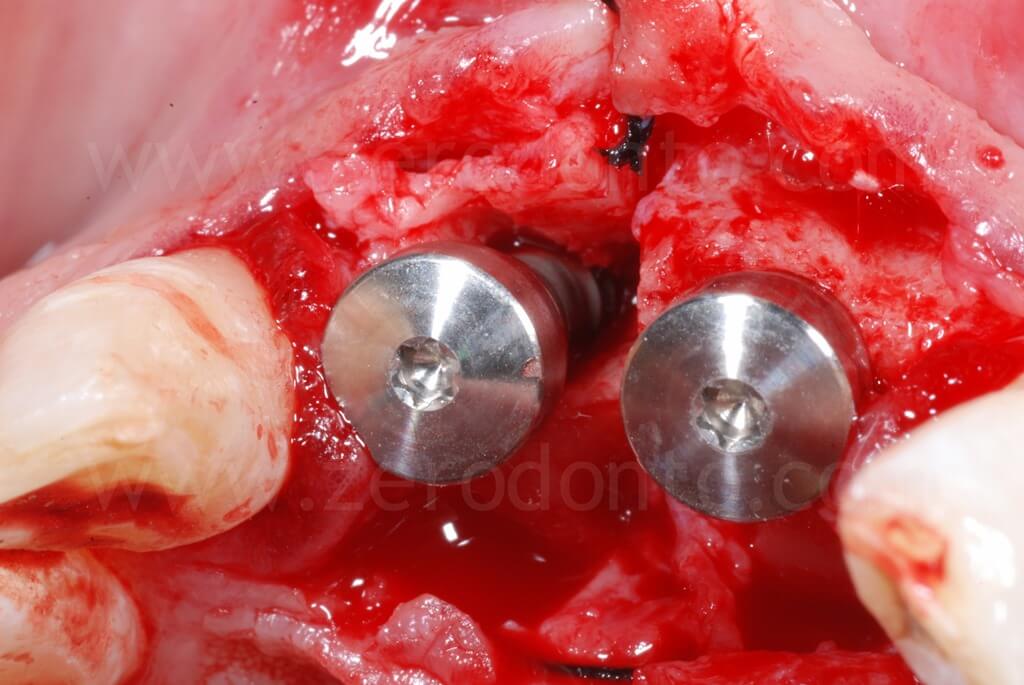


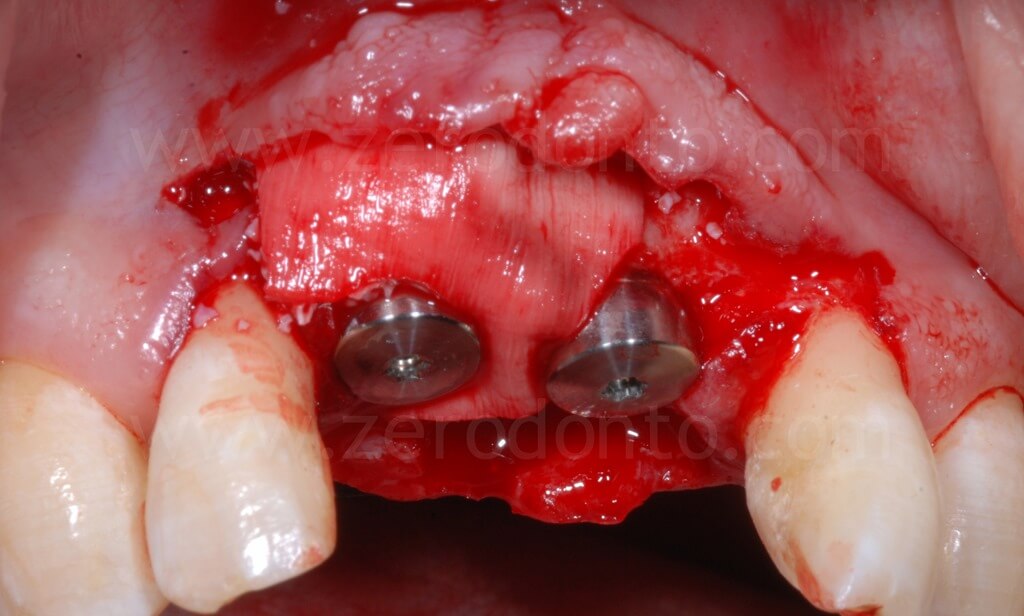
Finally, a suture with threaded polyester was performed.

Ninety days after surgery, an impression with screwed impression copings was taken to fabricate screw-retained resin temporary crowns.
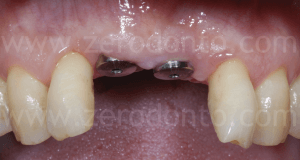



As previously planned, after screwing the first set of provisionals, the orthodontic implant anchorage was used to harmonize the prosthetic spaces, in particular between tooth 1.1 and 1.2.



After the orthodontic alignment, the gingival levels improved and the prosthetic spaces were considered sufficient for the case finalization.


Such crowns were modified intraorally about every 2 weeks in order to shape the transmucosal paths and the peri-implant tissues.

Due to the unfavorable crown-to-implant ratio (CIR), the case was finalized with titanium abutments and metal-ceramic single crowns, although to date they do not represent the first choice in esthetic sites.



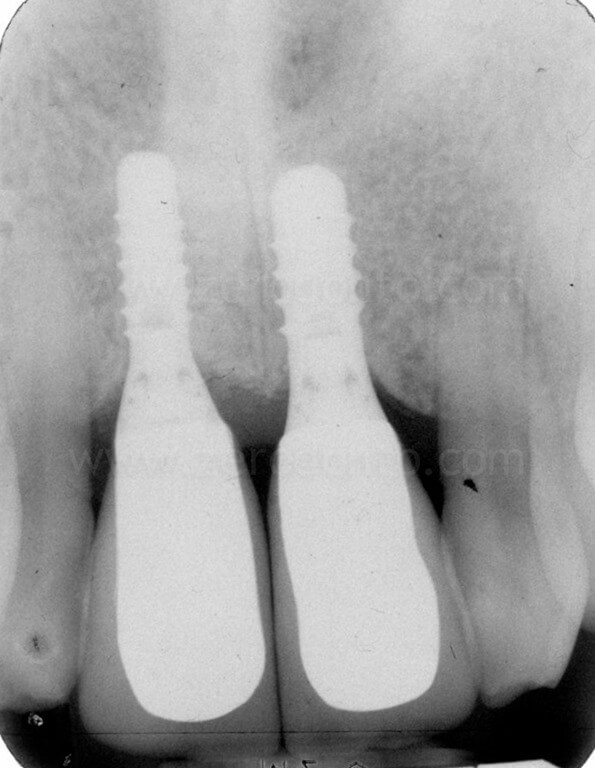
1 year follow-up



5 years follow-up

Conclusions
In the authors’ experience, the controlled split crest technique performed with screw-type expanders with increasing diameters, a full thickness flap and associated with a GBR is a predictable procedure in the esthetic area. Nevertheless, the technique is strictly related to the operator’s experience, thus requiring an adequate learning curve.
In case of fracture of the buccal bone, it has to be fixed with titanium screws, then performing a GBR and deferring implant placement.
Managing the correct axis of insertion is difficult, since it is related to multiple variables as the orientation of the adjacent teeth, the site of the correct horizontal osteotomy, the amount of desired bone expansion, the shape and diameter of the implant itself.
The association of a GBR allows to manage any gap or fenestration at the implant site, thus giving a greater predictability in the long-term maintenance of hard and soft tissues.
However, as previously discussed, if the anatomical conditions would not ensure adequate bone thickness suitable for a correct implant placement, a two-stage surgery is advisable, using the split-crest as support for GBR procedures with membranes and bone grafts.
REFERENCES
-
Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol, 2005; 32: 212–218.
-
Belser U, Buser D, Hess D, Schmid B, Bernard JP, Lang K. Aesthetic implant restorations in partially edentulous patiens: A critical appraisal. Periodontol 2000, 1998; 17:132-150.
-
Dawson A, Chen S, Buser D, Cordaro L, Martin W, Belser U. The SAC classification in implant dentistry. Quintessence Publishing, Berlin, 2009
-
Donos N, Mardas N, Chadha V. Clinical outcomes of implants following lateral bone augmentation: systematic assessment of available options (barrier membranes, bone grafts, split osteotomy). Journal of Clinical Periodontology, 2008; 35: 173–202.
-
Ferrigno N, Laureti M. Surgical advantages with ITI TE implants placement in conjunction with split crest technique. 18-month results of anongoing prospective study. Clin Oral Implants Res, 2005; 16(2):147-55
-
Han J-Y, Shin S-I, Herr Y, Kwon Y-H, Chung J-H. The effects of bone grafting material and a collagen membrane in the ridge splitting technique: an experimental study in dogs. Clin. Oral Impl. Res. xx, 2011; 000–000
-
Koo S, Dibart S, Weber H.P. Ridge-splitting technique with simultaneous implant placement. Compendium of Continuing Education in Dentistry, 2008; 29: 106–110.
-
Malchiodi L, Scarano A, Quaranta M, Piattelli A. Rigid Fixation by Means of Titanium Mesh in Edentulous Ridge Expansion (ERE) and Microbone Grafting for Horizontal Ridge Augmentation in the Maxilla. The International Journal of Oral & MaxilloFacial Implants, 1998; Vol.13, 5: 701-705
-
Scipioni A, Bruschi GB, Calesini G. The edentulous ridge expansion technique: a five-year study. Int J Periodontics Restorative Dent. 1994; 14(5): 451-459.
-
Simion M, Baldoni M, Zaffe D. Jawbone enlargement using immediate implant placement associated with a split-crest technique and guided tissue regeneration. Int J Periodont Res Dent, 1992; 12: 463-471.
-
Vercellotti T, Piezoelectric surgery in implantology: a case report–a new piezoelectric ridge expansion technique. The International Journal of Periodontics & Restorative Dentistry, 2000; 20: 358–365.
INFO:
zerodonto@gmail.com

