Coronavirus disease 2019, also known as COVID-19, has rapidly become a worldwide emergency. The World Health Organization (WHO) has recently declared the global pandemic. The pathogen responsible for such infection is the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although the new COVID-19 virus is different from SARS-CoV, it uses the same host receptor, namely human angiotensin-converting enzyme 2 (ACE2).
Why dentistry is a risk branch?
The COVID-19 virus was recently identified in saliva of infected patients. Saliva can have a pivotal role in the human-to-human transmission. Dentists and other healthcare professionals that perform aerosol-generating procedures may be unknowingly providing direct care for infected but not yet diagnosed COVID-19 patients, or those considered to be suspected cases for surveillance. As in bronchoscopy, inhalation of airborne particles and aerosols produced during dental procedures on patients with COVID-19 can be a high-risk procedure in which dentists are directly and closely exposed to this virus. Therefore, it is crucial for dentists to refine preventive strategies to avoid the COVID-19 infection by focusing on patient placement, hand hygiene and all personal protective equipment (PPE).
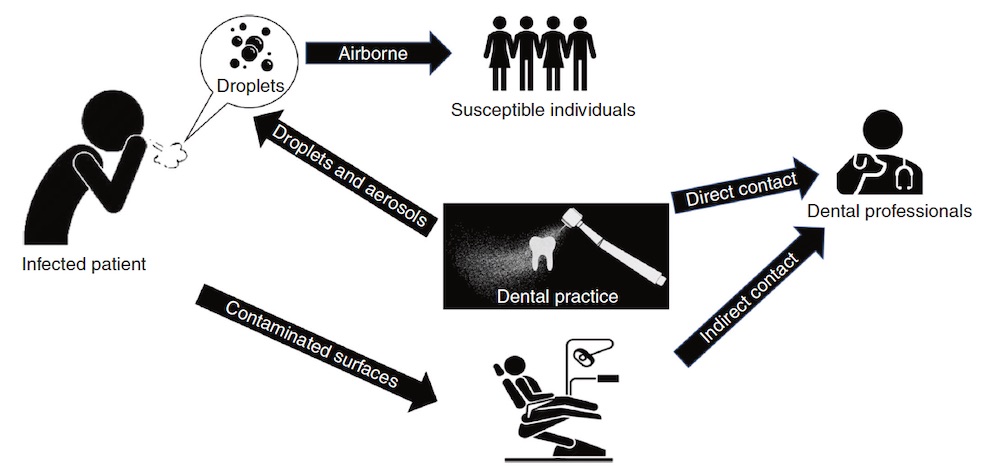
Figure taken from “Transmission routes of 2019-nCoV and controls in dental practice” – Peng et al. 2020
Due to the characteristics of dental settings, the risk of cross infections may be high between dental practitioners and patients. For dental practices and hospitals all over the world (the outbreak is pandemic), strict and effective infection control protocols are urgently needed. Due to the unique characteristics of dental procedures where a large number of droplets and aerosols could be generated, the standard protective measures in daily clinical work are not effective enough to prevent the spread of COVID-19, especially when patients are in the incubation period, are unaware they are infected or choose to conceal their infection.
What can dentists do to protect themselves and patients?
Hand hygiene has been considered the most critical measure for reducing the risk of transmitting microorganism to patients (Larson et al. 2000). SARS-CoV-2 can persist on surfaces for a few hours or up to several days, depending on the type of surface, the temperature or the humidity of the environment (WHO 2020c). This reinforces the need for good hand hygiene and the importance of thorough disinfection of all surfaces within dental clinics. Every surface in the waiting room must be considered at risk; therefore, in addition to providing adequate periodic air exchange, all surfaces, chairs, magazines and doors that come into contact with healthcare professionals and patients must be considered “potentially infected”. It may be useful to make alcoholic disinfectants and masks available to patients in waiting rooms. The entire air conditioning system must be sanitized very frequently.
The use of personal protective equipment (including masks, gloves, gowns and goggles or face shields) is recommended to protect skin and mucosa from (potentially) infected blood or secretions. As respiratory droplets are the main route of SARS-CoV-2 transmission, particulate respirators (e.g., N-95 masks authenticated by the National Institute for Occupational Safety and Health or FFP2-standard masks set by the European Union) are recommended for the routine dental practice.
The English researcher and writer John Dotz wrote a really interesting post on the differences between the various type of masks.
The management practice of the operating area should be quite similar to what happens with other patients affected by infectious and highly contagious diseases. As often as possible, the staff should work at an adequate distance from patients; furthermore, handpieces must be equipped with anti-reflux devices to avoid contaminations, improving the risk of cross-infections. Dentists should take strict personal protection measures and avoid or minimize operations that can produce droplets or aerosols. The 4-handed technique is beneficial for controlling infection. The use of saliva ejectors with low or high volume can reduce the production of droplets and aerosols (Kohn et al. 2003; Li et al. 2004; Samaranayake and Peiris 2004).
More useful recommendations for dental practice – as about evaluation of patients and oral examination or treatment of emergency cases – can be found in L. Meng1, F. Hua2 , and Z. Bian1 and also in Xian Peng1, Xin Xu1, Yuqing Li1, Lei Cheng1, Xuedong Zhou1 and Biao Ren (See References).
The need to stop and the need for clear guidelines
On 15 March 2020, the New York Times published an article entitled “The Workers Who Face the Greatest Coronavirus Risk”, where an impressive schematic figure described that dentists are the workers most exposed to the risk of being affected by COVID-19. As stated before, it is essential to give clear and easy guidelines to manage dental patients and to make working dentists safe from any risk. The transmission of the virus is mainly through inhalation/ingestion/direct mucous contact with saliva droplets; it is also critical to remember that the virus can survive on hands, objects or surfaces that were exposed to infected saliva.
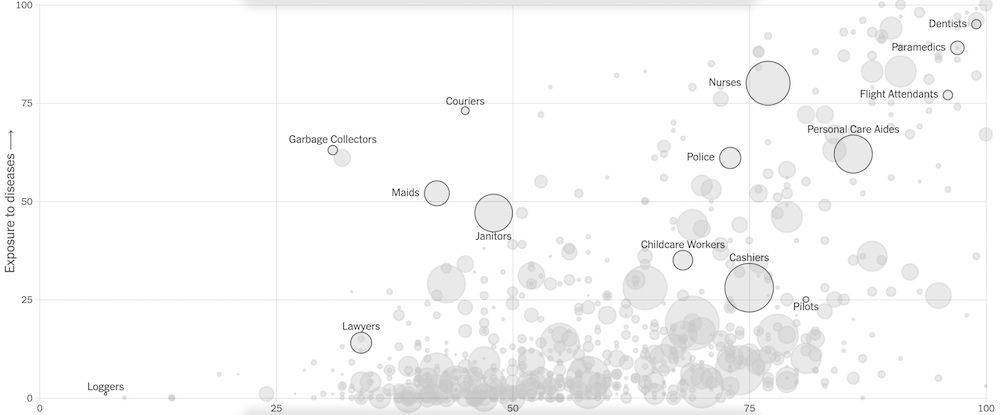
Figure is taken from the NYT article: The Workers Who Face the Greatest Coronavirus Risk
Although in some countries dental offices have been closed during the epidemic, a large number of emergency patients still go to dental clinics and hospitals for treatment. In any case, the most recommended guidelines indicate that dentists should avoid scheduling any patient: only such urgent dental diseases should be considered for intervention during the COVID-19 outbreak. This action will drastically limit interpersonal contacts, waiting time of patients in dental cabinets and, in general, conditions predisposing patients to be infected.
Recently, the European organisations of Health Professionals published a statement on COVID-19. In that document, they urged the European Commission and governments to support and protect healthcare professionals fighting SARS-CoV-2.
Prediction models
Several prediction models for Covid-19 have been recently published to support decision-making processes. Nonetheless, data are still scant, at high risk of bias and probably optimistic. More rigorous prediction models are needed and should be verified. (in Wynants, Van Calster…)
Specific protocols for weak patients, just like older adults (in Montero-Odasso, Goens, Kamkar…) and young pediatric patients (in Mallineni, Innes, Raggio…), should be urgently developed and shared to increase the efforts of the international dental community to manage properly the Covid-19 crisis.
Decision making processes in patient management
In order to perform a clinically- and ethically-driven decision-making process, dental interventions can be divided in the following categories:
- Emergency management of life-threatening conditions;
- Urgent conditions that can be managed with minimally invasive procedures and without aerosol generation;
- Urgent conditions that need to be managed with invasive and/or aerosol-generating procedures;
- Non-urgent procedures;
- Elective procedures.
Furthermore, the following considerations should be assessed before starting any urgent treatment.
- Operative procedures should be as minimally invasive as possible and aerosol-generating interventions should be avoided whenever possible;
-
Disposable devices and instrumentation should be used whenever possible to limit cross-infection risks;
-
Potential viral load in patients’ saliva could be reduced with 0.23% povidone-iodine mouthwash for 15 s before intervention ( Eggers et al., 2018);
-
Isolation with rubber dam should be used whenever possible to limit the spread of microorganisms (Cochran et al., 1989);
-
Intraoral radiographs should be limited in favor of extraoral imaging, in order to reduce salivation and gag reflex;
-
If pharmacologic management of pain is necessary, ibuprofen should be avoided in suspected and confirmed COVID-19 cases ( Day, 2020). (in Alharbi et al, 2020)
How to identify urgency and emergency treatments?
The American Dental Association (ADA) published guidance on dental emergency, nonemergency care in the last weeks called: What constitutes a Dental Emergency? Here below you will find a summary.
On 1st April the ADA also published an Interim Guidance for Management of Emergency and Urgent Dental Care. In the references, you can find all the resources from the ADA and download them.
Dental emergencies
- Uncontrolled bleeding
- Cellulitis or a diffuse soft-tissue bacterial infection with intra-oral or extra-oral swelling that potentially compromises the patient’s airway
- Trauma involving facial bones, potentially compromising the patient’s airway
Dental urgencies
- Severe dental pain from pulpal inflammation
- Pericoronitis or third-molar pain
- Surgical post-operative osteitis, dry socket dressing changes
- Abscess, or localized bacterial infection resulting in localized pain and swelling
- Tooth fracture resulting in pain or causing soft tissue trauma
- Dental trauma with avulsion/luxation
- Dental treatment required prior to critical medical procedures
- Final crown/bridge cementation if the temporary restoration is lost, broken or causing gingival irritation
- Biopsy of abnormal tissue
Non-urgent dental treatments that can be postponed
- Initial or periodic oral examinations and recall visits, including routine radiographs
- Routine dental cleaning and preventive therapies
- Orthodontic procedures other than those to address acute issues (e.g. pain, infection, trauma) or other issues critically necessary to prevent harm to the patient
- Extraction of asymptomatic teeth
- Restorative dentistry including treatment of asymptomatic carious lesions
- Aesthetic dental procedure
Conclusions (21 April 2020)
The treatment of COVID-19 is fundamentally based on containment measures: in China and South Korea, the severe application of such interventions has regularly and drastically reduced new cases and this experience shows that a reversion of epidemic growth is possible in the short-term. Many countries are investigating to get a possible vaccine as soon as possible. In the meantime, doctors are testing promising medicines to relieve symptoms and countries are all trying to avoid health systems crisis.
Financial Problems
The pandemic resulted in serious financial problems faced by dental offices, hospitals and healthcare operators. Dental interventions are currently limited to urgencies and the management of patients has become expensive and unpredictable. Healthcare workers are facing serious financial challenges and the intervention of competent authorities is claimed as very urgent to provide support and help to dental offices, hospitals and healthcare operators. (Farooq, Ali)
So, it is doubtful that the significant limitation of clinical and surgical activities in the medical and dental sector has represented a very impactful measure on the economy of the sector.
Impact of the interventions
Nevertheless, this drastic intervention can make it possible to protect the health and safety of citizens and contain the expansion of the COVID-19.
Citizens do their part. For example, speaking of children’s oral health, parents should be helping children develop good oral and diet habit such as effective brushing and flossing to avoid oral diseases and emergency.
On its webpage, the American Dental Association (ADA) has also published a link to frequently asked questions useful to dental professionals, mainly regarding personal protective equipment and patient communications. See references and online resources below for more info.
REFERENCES
• Alharbi A1, Alharbi S2, Alqaidi S2.
Guidelines for dental care provision during the COVID-19 pandemic
Saudi Dent J. 2020 Apr 7. doi: 10.1016/j.sdentj.2020.04.001
• Amber Ather, BDS, DDS∗, Biraj Patel, BDS, Nikita B. Ruparel, MS, DDS, PhD, Anibal Diogenes, DDS, MS, PhD, Kenneth M. Hargreaves, DDS, PhD
Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care
JOE � Volume -, Number -, – 2020
• Farooq I1, Ali S2.
COVID-19 outbreak and its monetary implications for dental practices, hospitals and healthcare workers.
Postgrad Med J. 2020 Apr 3. pii: postgradmedj-2020-137781. doi: 10.1136/postgradmedj-2020-137781. [Epub ahead of print
• R. Izzetti1 , M. Nisi1, M. Gabriele1, and F. Graziani1
COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy
Journal of Dental Research 2020 DOI: 10.1177/0022034520920580
• Mallineni SK1, Innes NP2, Raggio DP3, Araujo MP2, Robertson MD2, Jayaraman J4.
Coronavirus Disease (COVID-19): Characteristics in children and considerations for Dentists providing their care.
Int J Paediatr Dent. 2020 Apr 6. doi: 10.1111/ipd.12653. [Epub ahead of print]
• Meng L, Hua F, Bian Z.
Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine.
J Dent Res. 2020 Mar 12:22034520914246
• Montero-Odasso M1,2,3, Goens SD2, Kamkar N2, Lam R4, Madden K5, Molnar F6, Speechley M3, Stranges S3.
Canadian Geriatrics Society COVID-19 Recommendations for Older Adults. What Do Older Adults Need To Know?
Can Geriatr J. 2020 Mar 1;23(1):149-151. doi: 10.5770/cgj.23.443. eCollection 2020 Mar.
• Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B.
Transmission routes of 2019-nCoV and controls in dental practice.
Int J Oral Sci. 2020 Mar 3;12(1):9
• Sabino-Silva R, Jardim ACG, Siqueira WL.
Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis.
Clin Oral Investig. 2020 Feb 20
• Spagnuolo G, De Vito D, Rengo S, Tatullo M.
COVID-19 outbreak: an overview on Dentistry.
Int J Env Res Publ Health, 2020; 17:2094
• Wynants L1,2, Van Calster B2,3, Bonten MMJ4,5, Collins GS6,7, Debray TPA4,8, De Vos M2,9, Haller MC10,11, Heinze G10, Moons KGM4,8, Riley RD12, Schuit E4,8, Smits LJM13, Snell KIE12, Steyerberg EW3, Wallisch C10,14,15, van Smeden M4.
Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal.
BMJ. 2020 Apr 7;369:m1328. doi: 10.1136/bmj.m1328.
• Yan Wang, Chen-Chen Zhou, Rui Shu, Jing Zou
[Oral Health Management of Children During the Epidemic Period of Coronavirus Disease 2019]
J Sichuan Univ ( Med Sci Edi ), 2020, 51(2): 151 − 154
• LINEE GUIDA COVID-19 RESTART – AIO
• Summary of ADA Guidance During the COVID-19 Crisis (Full text download)
• ADA Interim Guidance for Management of Emergency and Urgent Dental Care (Full text download)
• ADA Interim Guidance for Minimizing Risk of COVID-19 Transmission (Full text download)
More resources online:
Latest updates about Corona virus disease-2019
Clinical resource on COVID-19 outbreak
Open-source health and medical research on the novel coronavirus (SARS-CoV-2) and COVID-19
Routes of transmission of COVID-19
Recommendations for putting on and removing personal protective equipment
Interim infection control recommendations (Includes details on protective equipment, hand hygiene practices and negative pressure rooms)
Recommendations on N95 respirators use and reuse
Steps for Healthcare Facilities to prepare for COVID-19
Risk Assessment and Public Health Management of Persons with Potential COVID-19 exposure
Environmental protection agency approved COVID-19 chemical disinfectants
Interim Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response
DISCLAIMER: This is fundamentally a summary of the most important concepts taken from the articles published on PubMed about Dentistry and the new coronavirus, The purpose is educational. We, as a point of reference for the dentists on the web, want to help everyone to get clear, trustful, information.

