Post updated on September 27, 2018
Bisphosphonates are a cathegory of drugs that inhibit bone remodelling mediated by osteochlasts. They are stable molecules, inhorganic pyrophosphates’ analogues, used in prevention and treatment of several methaboholic and oncohological disorders of skeleton as osteopenia, osteoporosis, Paget disease, osteogenesis imperfecta, multiple myeloma, malignant hypercalcemia and bone metmetastasis. Bisphosphonates reduce patpathological fractures incidence, inhibiting osteoclasts function and increasing bone density, to improve patients quality of life. Despite they have a short plasmatic half-life, since they are resistant to enzymatic hydrolysis and ligate Ca++ of hydroxyapatite, these molecules can stay for years in bone mineralized matrix and in high turnover seats. When osteoclasts start to release H+, making the pH acid, bisphosphonates are released from bone and phagocytized by these cells, who later will go in apoptosis.
Maxillary bones features
Bisphosphonates tend to settle in bone segments interested in active process of remodeling, as well as seats affected by inflammatory processes. Maxillary bones, under mechanical stress and frequent microfractures, “live” a continue remodeling state, therefore this is preferential seat where bisphosphonates accumulate.
The persistence of repeated traumas due to the presence of the dental elements and the development of the masticatory forces generates, at the level of the alveolar bone, a turnover 10 times greater than that of the long bones (e.g. tibia). It should be remembered that the maxillary bones, unlike the long bones and the vertebrae, undergo an intramembranous ossification and the jaw is the densest bone in absolute (the density is reduced in the molar and premolar area). The trabecular bone has a turnover of 6/7 times higher than that of the compact bone.
This allows a rapid accumulation of bisphosphonates and a slower release over time when they are suspended. Moreover, the jaws are scarcely protected from the risk of infection since the thin epithelium of the oral mucosa can be easily traumatized and expose the underlying bone to contact with over 500 different species of microorganisms. Unlike any other location, tissue healing can be continually compromised by the risk of bacterial contamination after surgery or a trauma. trauma.
trauma.
Classification and mechanism of action
Etidronate and Clodronate are simple bisphosphonates, the only ones to be metabolized into intracellular cytotoxic and non-hydrolysable ATP analogues, which accumulating in osteoclasts, induce their death.
Pamidronate, Alendronate, Risedronate, Ibandronate and Zolendronate are aminobiphosphonates, that are bisphosphonates endowed with an amine group in correspondence of the lateral chain R2, commonly used for intravenous preparations as they are poorly absorbed by the gastrointestinal apparatus. They are 100 to 10000 times more powerful than simple bisphosphonates. Moreover they are effective inhibitors of the enzyme farnesyl-diphosphate synthase that controls production of cholesterol and other prenylated proteins (GTPases), implicated in important intracellular osteoclast processes (eg cell morphology, cytoskeleton organization, vesicular traffic, apoptosis).
It also seems that the aminobisphosates have antiangiogenic effects, interferring with the endothelial growth factor (VEGF) and anticancer effects, promoting apoptosis of cancer cells and reducing the formation of metastases.
The affinity of bisphosphonates for hydroxyapatite depends on their chemical structure. From the affinest to less affine we have: Zolendronate, Pamidronate, Alendronate, Ibandronate e Risedronate. Finally, Clodronate has the poorest affinity.
The persistence of amino-bisphosphonates in the bone tissue last many years, but remains very short for Clodronate.
Zolendronate and Pamidronate are the most active molecules, with the highest affinity for hydroxyapatite and capable of weakly binding plasma proteins. Their prolonged use suppresses the activity of macrophages, angiogenesis, systemic bone turnover and the reparative processes of local microtraumas.
Maxillary osteonecrosys
The spread of bisphosphonates in recent years, supported by the excellent safety profile of these drugs, has generated the increasingly worrisome appearance of devastating side effects on maxillary bones. Osteonecrosis of the jaw is a multifocal disease that generally affects patients treated for long periods with intravenous administration of aminobiphosphonates and may occur spontaneously or, more frequently, following an invasive procedure involving teeth or oral tissues (e.g. tooth extractions). It appears as a necrotic area of non-vascularized bone, which occur in maxillofacial region and persists for more than 8 weeks. Signs and associated symptoms are: pain, dental mobility, edema, fistulae, paresthesias, ulcerations, susceptibility to pathological fractures.
A chronic sinusitis, secondary to osteonecrosis of the upper jaw, with or without oroantral fistula, may be the first clinical manifestation of disease.
Sometimes the lesion can remain asymptomatic for long periods, even years, until the inflammation does not involve the surrounding tissues. Cases of cancer patients have been described, in which the lesions occurred spontaneously in edentulous areas or close to exostosis. Some patients may also report altered sensitivity of the affected area due to the compression on the vascular nerve bundles exerted by the inflamed tissues.
With advancing age, continuous traumas, the increase in bone turnover and periodontal disorders, the incidence of osteonecrosis tends to increase.
The hystological exam of necrotic area shows spreaded osteomyelitis and formation of a necrotic bone clot contaminated by bacteria and fungi.
In some cases, the bone surrounding the lesion may show several signs of micro-fractures that witness the loss of self-healing capacity.
Recently, a form of osteonecrosis of the jaws has been defined associated with the use of other drugs,as denosumab, monoclonal antibody with anti-osteoclastic activity, bevacizumab and sunitinib, which have antiangiogenic action. Therefore today we also speak of osteonecrosis of the jaws induced by drugs, since these substances increase the incidence and prevalence of the disease both in patients treated for osteoporosis and in cancer patients.
when bisphosphonates are administered together with corticosteroids, osteonecrosis may occur early and in a severe form.
Diagnosis
The conditions necessary for the diagnosis of ostenecrosis are:
- Established current or previous bisphosphonate intake.
- Necrotic bone exposure in maxillofacial region for more than 8 weeks.
- Negative anamnesis for radiation therapy in the craniofacial region and absence of neoplastic lesions.
Staging
The clinical staging (AAOMS 2009) includes 5 stages:
- At risk: patients treated with oral or intravenous bisphosphonates who have no obvious lesions.
- Stage 0: patients with nonspecific symptoms and radiological changes in the absence of bone necrosis.
- Stage 1: asymptomatic patients with exposed necrotic bone or fistulae.
- Stage 2: symptomatic patients (e.g. pain, erythema, infections) with exposed necrotic bone or fistulae.
- Stage 3: Stage 2 patients who have one of the following conditions: pathological fractures extending beyond the alveolar bone, extraoral fistulae, oroantral or oronasal communications, osteolysis extended to the lower edge of the jaw or to the floor of the maxillary sinus.
The severity of the disease is closely related to patient age and renal function, whisch is influenced by various systemic diseases: arterial hypertension, diabetes, glomerulonephritis, infections, liver thyroid and kidney diseases.
Differential diagnosis
The differential diagnosis should be placed with the following deseases: alveolar osteitis, chronic sclerosing osteomyelitis, sinusitis, periodontal disease, periapical lesions, osteoradionecrosis, bone metastases, bone sequestration, TMJ disorders.
Seat
The osteonecrotic lesions occur in 65% of cases in the jaw, in 28.4% of cases in the maxilla, in 6.5% in both, in 0.1% in other locations, and with greater prevalence in correspondence of prominences bones (ie bulls, exostoses, miloioidea crest). The most affected area of the jaw is the molar and premolar region, where bone density is reduced and the oral mucosa is thinner. An unusual form of osteonecrosis of the external auditory canal was then described.
Risk factors
The main risk factors are:
- Factors related to the intake of bisphosphonates (i.e. power and duration of therapy)
- Local factors (e.g. previous dental extractions, dento-alveolar surgery, use of incongruous prostheses, exostoses, oral infections, poor oral hygiene)
- Systemic factors (e.g. diabetes mellitus, chemotherapy, corticosteroid therapy, malnutrition, tobacco smoke, advanced age)
Among patients taking bisphosphonates, those treated for at least one year with intravenous infusions and those treated for at least 3 years with oral therapies are considered to be at high risk of getting osteonecrosis of the jaws.
Incidence and Prevalence
The close association between intravenous aminobiphosphonates and maxillary osteonecrosis suggests that these drugs are more bioavailable than those for oral use and are literally incorporated into the bone matrix without being degraded. The incidence in oncologic patients is dependent on the primary neoplasm, on the doses and duration of therapy, on possible concomitant therapies (glucocorticoids, antiangiogenic drugs) and ranges from 0.8% to 12%.
The highest incidence was found in patients treated with a combination of pamidronate and zolendronate for the treatment of multiple myeloma (5-51%). The major factor predisposing to osteonecrosis of the jaws in patients with multiple myeloma is dental extraction. The prevalence in oncologic patients ranges from 0.12% to 0.186% to reach 20% in special high-risk subgroups.
The incidence in patients treated for osteoporosis is quite low, between 0.01% and 0.04%, and only slightly higher than the frequency observed in the entire population; the prevalence is between 0% and 0.04%.
Etiopathogenetic hypotheses
The exact etiopathogenesis of this disease is currently unknown. In particular, it is not clear if the infectious process, certainly involved in the pathophysiology of the disease, precedes or follows bone necrosis. The inhibitory action of bisphosphonates on the proliferation of oral epithelial keratinocytes could contribute to damage oral mucosa exposing it to the risk of bacterial infection. This, in turn, is able to stimulate bone resorption and directly contribute to necrosis. Another theory (outside-inside) supposes that the bisphosphonates generate a local immunosuppression that would favor the establishment of inflammatory and infectious processes that, once the bone tissue is reached, would cause osteonecrosis.
Pharmacogenomics is object of study too, since genetic polymorphisms of the enzyme farnesyl pyrophosphate synthase or CYP2C8 genes of cytochrome P450 are thought to represent predisposing factors to the disease.
It has also been advanced the hypothesis that the acidic environment created in the presence of an inflammatory state could favor a cytotoxic action by the bisphosphonates. This action, directed to the soft tissues of the oral cavity (ie keratinocytes, fibroblasts, endothelial cells) could be the primum movens of the degenerative process that culminates in bone necrosis. The damage to the oral mucosa, therefore, and the partial inactivation of the macrophages by the bisphosphonates, would allow the microorganisms to penetrate and so the spread of the infection.
Clinical indications
Bone metastases are the main indication for the use of bisphosphonates.
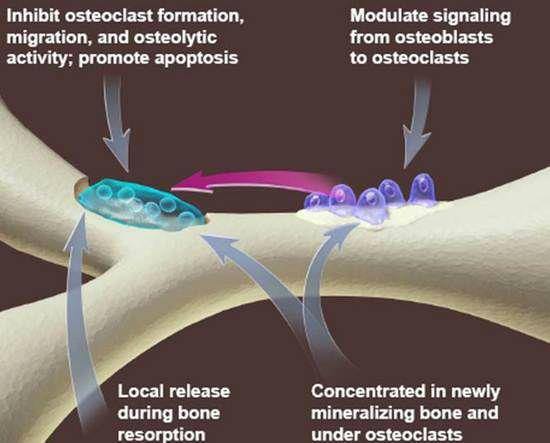
Bone remodeling is a physiological process involving bone-producing osteoblasts and osteoclasts that destroy it. Any alteration of this balance is reflected in an increase or decrease in bone density. Healthy bone homeostasis is regulated by the RANK / RANKL / OPG system. The RANKL polypeptide expressed on the surface of the osteoblasts binds its RANK receptor expressed on the surface of the osteoclast precursors, or alternatively, the OPG receptor (osteoprotegerine) produced by osteoblasts, gingival fibroblasts and periodontal ligament cells. The RANKL / RANK interaction induces differentiation and activation of osteoclast precursors in mature cells. OPG can block osteoclastogenesis and therefore bone resorption by binding the RANKL. The tumor cells, in fact, after invading the bone microenvironment, produce osteolytic lesions by reducing the action of OPG through the production of proteins such as PTH (parathormone). These metastases also alter bone homeostasis through the expression of growth factors and cytokines that increase the activity of osteoclasts. Excessive bone metabolism leads to the appearance of clinical symptoms (pain, hypercalcaemia, pathological fractures) that can be controlled by drug therapy, that can prevent severe skeletal complications and improve the quality of life of patients.
The powerful amino-bisphosphonates administered intravenously to oncologic patients have antiangiogenic properties that are directly implicated in the development of jaw osteonecrosis and, in this regard, the plasma concentration of VEGF (endothelial growth factor) can be considered a predictive marker for risk to develop the disease.
Bisphosphonates also represent the largest class of drugs prescribed for the treatment of osteoporosis and other diseases characterized by excessive bone resorption. The direct action to osteoclasts restores the balance between bone apposition and reabsorption.
Diagnostic tools
High-resolution bitewing and periapical radiographs, in addition to ensure the control of local risk factors (eg caries, periodontal and periapical lesions), allow to observe some anatomical details suggestive of a possible diagnosis of osteonecrosis: hard lamina thickening, density increases of the trabecular portion of the alveolar bone, enlargements of the periodontal space.
Panoramic radiographs, useful to provide a general picture that includes images related to adjacent anatomical structures, allow to observe the eventual incomplete healing of post-extraction sites, the formation of seizures, thickening of the mandibular canal or of the maxillary sinus walls, periosteal reactions , oroantral fistulae.
Radiographically, the osteonecrosis of the jaws manifests itself as a radiopaque area corresponding to a bone sequestration generally surrounded by an irregular radiotransparent zone. In the advanced phases, a poorly defined osteolytic area is observed in the context of the cortical bone, loss of spongy bone (trabeculation), reduction of bone density. These images appear quite similar to the radiological aspects typical of osteomyelitis.
Since radiological findings do not provide pathognomonic images, the differential diagnosis with lesions deriving from other diseases (e.g. chronic sclerosing osteomyelitis, osteoradionecrosis, bone metastasis and Paget’s disease) is fundamental.
Computed tomography, if performed in time, can reveal some aspects that arise in the early asymptomatic or prodromal phase of the disease: alterations of the skeletal architecture, increases in the trabecular density, initial signs of osteosclerosis.
CBhjkghjklghjkl’CT can detect the same alterations but with the advantage of emitting less radiation doses and providing more details on periapical and periodontal lesions.
Magnetic resonance, on the other hand, can be useful to highlight edema, soft tissue thickening and cervical lymphadenopathy.
Scintigraphy using Tc99 MDP or HDP is the most sensitive diagnostic tool to formulate an early diagnosis. An increase in radionuclide uptake may in fact indicate the future development of osteonecrosis in a given area, but is not able to distinguish lesions resulting from bone metastases, osteoradionecrosis, osteomyelitis or steroid-induced osteonecrosis.
A precise localization of osteonecrotic areas can be obtained by PET or SPECT.
Implant-prosthetic rehabilitation
The establishment of an inflammatory state (peri-implantitis), following the insertion of dental implants, is a possible complication that could trigger an osteonecrotic process. The individual risk of each patient is influenced by the primary pathology and the chosen therapy (bisphosphonates), the duration and frequency, the presence of other disorders and other treatments. In view of these considerations, it is convenient to resolve any inflammatory and infectious foci before proceeding with surgery and to monitor the affected site clinically and radiographically until complete recovery. Perioperative antibiotic prophylaxis is strongly recommended. Bisphosphonates do not represent an absolute contraindication to implant therapy as there are cases of successful osseointegration, even in oncologic patients (the implants most at risk will be those positioned in the posterior portion of the mandible). Naturally, a careful evaluation of clinical cases and of possible candidates for implant-prosthetic rehabilitation will be opportune, providing patients with complete and detailed information on possible risks. The decision will also be influenced by the possible need to increase bone thickness and maxillary sinus surgery. Compliance and motivation to maintain an adequate oral hygiene are decisive factors in projecting the individual risk of each patient. The mobile prosthesis, alternative therapy to implants, represents in turn a predisposing factor for the development of osteonecrosis of the jaws due to its ability to damage soft tissues.
Prevention
Prevention and control of risk factors are very important and often overlooked aspects of this pathology. During a preliminary dental examination, it is useful to subject to a careful intra-oral examination the patients who must be treated with intravenous bisphosphonates, in order to plan treatments aimed to ensure dental and periodontal health for starting the therapy. If surgical procedures are required, it will be necessary to wait for complete healing of the tissues (14-21 days), to prescribe antibiotics and local antiseptics before and after the procedures, to ensure that the patients are able to maintain good oral hygiene. All non-urgent procedures may be postponed or scheduled during therapy. With regard to patients taking oral bisphosphonates for less than 3 years, it appears that there are no contraindications to oral surgery. If, on the other hand, these patients take corticosteroids at the same time, it would be advisable to prescribe a “holiday drug” for the 3 months preceding the surgery and the 3 months that follow it, if the general conditions allow. In case of extensive surgery and in presence of multiple risk factors (e.g. diabetes, parodontopathies, glucocorticoid therapy, immune deficiency, smoking) it is recommended to prescribe a drug holiday, assumed that patients are not exposed to harmful consequences for bone health. From a pharmacological point of view, prevention strategies for patients treated with bisphosphonates both orally and intravenously are aimed at controlling infections since these, although the exact sequence of events are not known, are certainly implicated in the process of etiopathogenesis of the disease . Antibiotic prophylaxis is necessary in view of the systemic and local effects of bisphosphonates (e.g. suppression of bone remodeling and angiogenesis, soft tissue toxicity, interference with the immune system and delayed healing) and is imperative in case of dental extraction. The pharmacological regimen should be followed before surgery and subsequently, until the surgical site is fully recovered. From a preventive perspective, atraumatic extraction, obtained by using orthodontic forces, can be a valid alternative to traditional surgery. The conservative approach, including root canal therapy and non-invasive periodontal surgery, is highly recommended and, for non-recoverable teeth, the removal of the crown and the endodontic therapy of the remaining roots can be indicated. Ultimately, the best preventative approach towards patients is the individual one, by evaluating concomitant pathologies and risk factors
Treatment of osteonecrosis of the jaws
The approach pursued so far is palliative and aimed to improve the quality of life of patients through the control of clinical symptoms (pain, infections) and the progression of necrosis. The initial stages (stages 0 and 1) of the osteonecrosis of the jaws are treated conservatively, through the elimination of all the active oral and periodontal lesions and the administration of antibiotics, local antiseptics, analgesics, antifungals and fluorine. The antibiotic of first choice is amoxicillin which, in the case of documented allergies, can be replaced by erythromycin, clindamycin, lincomycin and metronidazole. As the action of the drug is subordinated to the local microcirculation and to the degree of penetration into the infected site, with the progression of the disease, the lesions become poorly vascularized and less sensitive to systemic antibiotic therapy. The topical applications of chlorhexidine gluconate are effective both against bacteria and against fungi (especially Candida spp).
In the case of injuries that are not sensitive to this conservative approach and for the most severe cases, one can opt for a surgical treatment of the necrotic area. The majority of authors recommend to follow a conservative approach aimed to superficial debridement and to the removal of bone sequestration for patients in stage 2. On the contrary, they propose an aggressive therapy consisting of partial or total bone resection for patients with stage 3. In any case and regardless of the severity of the disease, injuries that cause constant damage to the soft tissue should be removed. The osteotomy should be performed after elevating a full-thickness flap in the periosteum, in order to have resection margins that reach healthy and bleeding tissue. Soft tissues should be repositioned without tension to cover blunt bone margins, which can not cause damage or bleeding by absorbable sutures in 7 days. Surgical therapy seems effective at reducing pain, infection, osteolysis, and improving the soft tissue state. In addition to surgical debridement, and for stage 2 patients, it may be helpful to apply platelet-rich autologous growth factors (PDGF) or platelet-rich autologous plasma (PRP) locally to promote complete recovery of the surgical site.
It’s possible to use also resorbable fillers containing antibiotics at high concentrations (Collatamp and Syntacoll) based on purified type I bovine collagen and gentamicin sulfate (2.0 mg / cm2), which are applied locally at surgically and potentially infected sites. These spongy devices release high concentrations of antibiotic in order to avoid the harmful effects on the organism linked to long-term and high-dose systemic antibiotic therapy.
In patients with multiple myeloma and those treated with low doses of bisphosphonates for the treatment of osteoporosis, surgical therapy gave the best results.
Recently, the administration of teriparatide, recombinant parathyroid hormone with osteoanabolic action, has given good results in facilitating the healing of mandibular alveolar bone lesions in patients with osteoporosis.
Additional therapies to traditional surgery use laser systems to remove bone lesions (Er: YAG and Nd: YAG). Low level laser therapy (GaAlAs, Nd: YAG) is indicated both in conjunction with conservative and surgical therapies, as it improves the vascularization of the mucosa, promotes bone regeneration and reduces pain. There are also therapeutic protocols that offer laser phototherapy (InGaAlP) combined with drug therapy and surgical treatment with topical application of PRP.
Hyperbaric oxygen therapy can also aid surgical and non-surgical treatments to promote bone healing.
Finally, the grafting of mesenchymal stem cells and the neural crest is the subject of a therapeutic strategy aimed at reducing the inflammation that characterizes the osteonecrosis of the jaws and to exploit immunomodulatory properties capable of facilitating endogenous tissue regeneration and angiogenesis.
Conclusions
The wide variety of therapeutic protocols available has provided controversial results to this day and does not yet allow standardization of collected data to arrive at official “guidelines”.
Collecting a complete medical history, providing tools for good oral hygiene and prevention, carrying out frequent clinical checks and choosing minimally invasive treatments are the appropriate behavior to avoid, as far as possible, the development of the disease, which, it should be remembered, can also arise 10 years from taking drugs.
While there is a solid epidemiological evidence to support the association between intravenous bisphosphonate administration and the onset of the disease, on the other hand, the increase in cases recorded in recent years linked to prolonged oral therapies for osteoporosis suggests that the incidence of jaw osteonecrosis in such patients is higher than previously believed. Therefore it is essential to focus on patients affected by osteoporosis, to identify among these high-risk cases and enhance preventive measures. The synergy among all the specialists interested in the management of patients taking bisphosphonates is fundamental to implement a strategic preventive and / or therapeutic individual plan, according to a multidisciplinary approach.
References
• Bisphosphonate Related Osteonecrosis of the Jaw: An Update. Vijay Kumar Raman Kant Sinha J. Maxillofac. Oral Surg. (Oct–Dec 2014) 13(4):386–393
Medication-related osteonecrosis of the jaw: a preliminary retrospective study of 130 patients with multiple myeloma. Woo-Sung Choi, Jae-Il Lee, Hyun-Joong Yoon, Chang-Ki Min and Sang-Hwa Lee Choi et al.
Maxillofacial Plastic and Reconstructive Surgery (2017) 39:1
• Osteonecrosis of the jaw during biyearly treatment with zoledronic acid for aromatase inhibitor associated bone loss in early breast cancer: A literature review HampigRaphaelKourien,JoelleAntoun,ElieElRassy,MarcRassy,ClaudeSader-Ghorra, Joseph Kattan. Journal of Bone Oncology4(2015)77–79
• Bisphosphonate-related osteonecrosis of the jaw: specificities
Siri Paulo, Ana Margarida Abrantes, Mafalda Laranjo, Lina Carvalho, Arménio Serra, Maria Filomena Botelho, Manuel Marques Ferreira. Oncology Reviews 2014 volume 8: 254
• Dental implants in patients treated with antiresorptive medication – a systematic literature review Christian Walter, Bilal Al-Nawas, Tim Wolff, Eik Schiegnitz and Knut A. Grötz Walter et al. International Journal of Implant Dentistry (2016) 2:9
• Diagnosis and Management of Osteonecrosis of the Jaw: A Systematic Review and International Consensus. Aliya A Khan, Archie Morrison, David A Hanley, Dieter Felsenberg, Laurie K McCauley, Felice O’Ryan, Ian R Reid, Salvatore L Ruggiero, Akira Taguchi, Sotirios Tetradis, Nelson B Watts, Maria Luisa Brandi, Edmund Peters, Teresa Guise, Richard Eastell, Angela M Cheung, Suzanne N Morin, Basel Masri, Cyrus Cooper, Sarah L Morgan, Barbara Obermayer-Pietsch, Bente L Langdahl, Rana Al Dabagh,K. Shawn Davison, David L Kendler, George K Sándor, Robert G Josse, Mohit Bhandari, Mohamed El Rabbany, Dominique D Pierroz, Riad Sulimani, Deborah P Saunders, Jacques P Brown, and Juliet Compston, on behalf of the International Task Force on Osteonecrosis of the Jaw
Review Journal of Bone and Mineral Research, Vol. 30, No. 1, January 2015, pp 3–23
• Bisphosphonate-Related Osteonecrosis of the Jaw:
A Review of the Literature Eder Alberto Sigua-Rodriguez, Renato da Costa Ribeiro, Ana Caroline Ramos de Brito, Natalia Alvarez-Pinzon, and José Ricardo de Albergaria-Barbosa Hindawi Publishing Corporation International Journal of Dentistry
Volume 2014, Article ID 192320, 5 pages
• Understanding bisphosphonates and osteonecrosis of the jaw: uses and risks S. ROSINI, S. ROSINI, I. BERTOLDI, B. FREDIANI. European Review for Medical and Pharmacological Sciences 2015; 19: 3309-3317
• Medication-Related Osteonecrosis of the Jaw: New Insights into Molecular Mechanisms and Cellular Therapeutic Approaches Thomas Lombard, Virginie Neirinckx, Bernard Rogister, Yves Gilon, and SabineWislet Hindawi Publishing Corporation
Stem Cells International Volume 2016, Article ID 8768162, 16 pages
• Prevention of medication-related osteonecrosis of the jaws secondary to tooth extractions. A systematic review Márcio Diniz-Freitas, Jacobo Limeres Med Oral Patol Oral Cir Bucal. 2016 Mar 1;21 (2):e250
• Prophylaxis and antibiotic therapy in management protocols of patients treated with oral and intravenous bisphosphonates
Elena-Beatriz Bermúdez-Bejarano, María-Ángeles Serrera-Figallo, Aida Gutiérrez-Corrales, Manuel- María Romero-Ruiz , Raquel Castillo-de-Oyagüe, José-Luis Gutiérrez-Pére , Daniel Torres-Lagares. J Clin Exp Dent. 2017;9(1):e141-9
• Relationship between disease stage and renal function in bisphosphonate-related osteonecrosis of the jaw Yun-Ho Kim, Han-Kyul Park, Na-Rae Choi, Seong-Won Kim, Gyoo-Cheon Kim, Dae-Seok Hwang, Yong-Deok Kim, Sang-Hun Shin, Uk-Kyu Kim
J Korean Assoc Oral Maxillofac Surg 2017;43:16-22
• Surgical treatment vs. conservative treatment in intravenous bisphosphonate-related osteonecrosis of the jaws. Systematic review
Aida Comas-Calonge, Rui Figueiredo, Cosme Gay-Escoda
J Clin Exp Dent. 2017;9(2):e302-7
• Treatment of bisphosphonate related osteonecrosis of the jaws – a report of seven cases Joanna Jakiel, Mansur Rahnama, Joanna Szczerba-Gwóźdź. Contemp Oncol (Pozn) 2016; 20 (6): 486–490
• Dental extraction following zoledronate, induces osteonecrosis in rat´s jaw
Ximena Vidal-Gutiérrez , José-Francisco Gómez-Clavel, Luis-Alberto Gaitán-Cepeda.
Med Oral Patol Oral Cir Bucal. 2017 Mar 1;22 (2):e177

