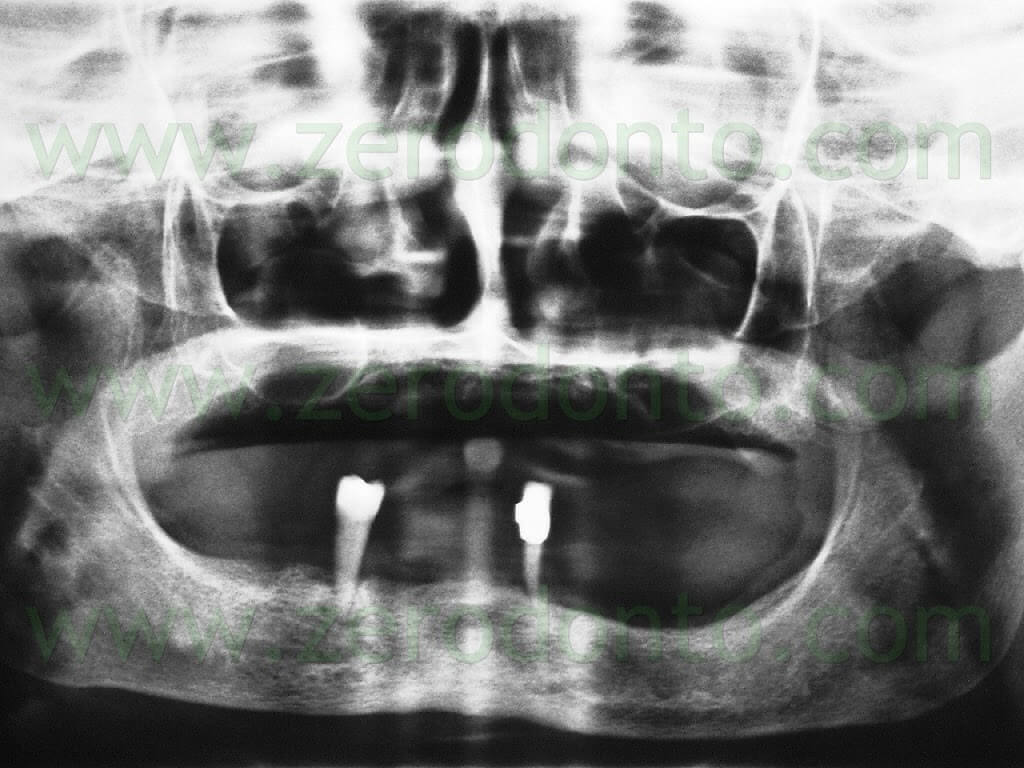
A 63-year-old female patient presented with a severe chronic periodontitis at the mandibular arch. Only teeth 33 and 44 were present and had been used as abutments for a resin removable partial denture which did not satisfy the functional and estethic needs of the patient. Moreover, a metal-ceramic crown with a supragingival margin and a mesial metal connector was evidenced on tooth 33; the patient reported that the mandibular front teeth had been previously prepared for a metal-ceramic fixed dental prosthesis, in order to limit the discomfort due to the mobility of such teeth.At the maxillary arch, the patient wore a complete removable denture which was esthetically unsatisfactory but valid to accomplish oral functions.
Consequently, since the patient wanted to postpone the maxillary rehabilitation for personal reasons, the maxillary denture was relined, in order to stabilize the occlusion and to use it for the intermaxillary registrations necessary to restore the mandibular arch.
The patient presented with good general health and was a moderate smoker (10/15 cigarettes per day). Although the authors explained all the risks related to smoking in the presence of implant-supported restorations, the patient refused to stop or reduce smoking.
After discussing with the patient all the possible removable and fixed prosthetic solutions and achieving a written consent form, it was decided to restore the mandibular arch by means of a full-arch fixed implant-supported restoration. A removable partial denture with a metal structure was used as temporary restoration before the implant placement and during the healing period. Tooth 33 was preserved in the arch in order to keep the vertical dimension unaltered.
Surgical procedures
A 2% solution of carbocaine was injected as local anesthesia; no inferior alveolar nerve block anesthesia was used, in order to allow the patient to answer any painful sensation due to proximity of the inferior alveolar nerve.
An incision was made in the mandibular crest using a 15C Bard Parker blade; the incision was slightly lingual, in order to preserve a sufficient amount of buccal keratinized mucosa.
After elevating a full thickness flap, buccal and lingual spreading sutures were made, in order to avoid the flaps to interfere with the surgical procedures.
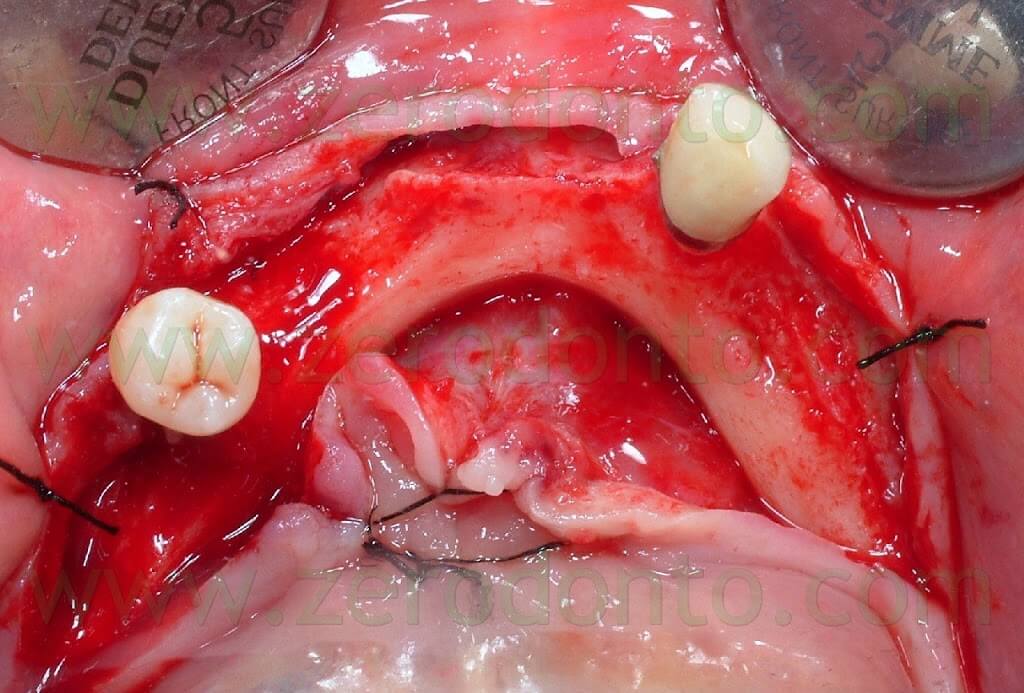
Due to the very thin thickness of the coronal part of the alveolar margin, osteotomy and osteoplasty of the edentulous ridge were made using a tungsten carbide bur mounted on a low speed handpiece under constant irrigation with physiological saline solution. Such a procedure allowed to regularize the edge of the ridge and to achieve a proper amount of basal bone to optimize implant placement.
In order to check the quantity of removed bone tissue, the osteoplasty was performed first on only one half of the arch; then, it was completed on the opposite half of the arch, so as to control the height of bone during its removal.
A periosteum detacher was carefully used to identify the mental foramina, in order to check the position of the inferior alveolar nerve previously analyzed by means of the CT scan.
Seven non-submerged implants were positioned; although 6 implants are usually considered a standard in the lower arch, one more implant was placed in the left distal area due to the local scarce bone quality.
An extremely careful approach was used not to damage the lingual cortical bone as well as the sublingual artery. The implants were positioned as much parallel to each other and perpendicular to an ideal occlusal plane as possible, in order to optimize the functional load distribution.
To achieve such a goal, tooth 33 was left in the arch during all the surgical procedures, so as to check the occlusion and the mutual parallel position of the implants intraoperatively.
After placing 2 mm high healing screws, an e-PTFE coated polyester suture was used.

Then, the patient was prescribed with antibiotics, painkillers and 0.2% chlorexidine.
Prosthetic Procedures
Three months after surgery, osseointegration of the implants was verified both clinically and radiographically
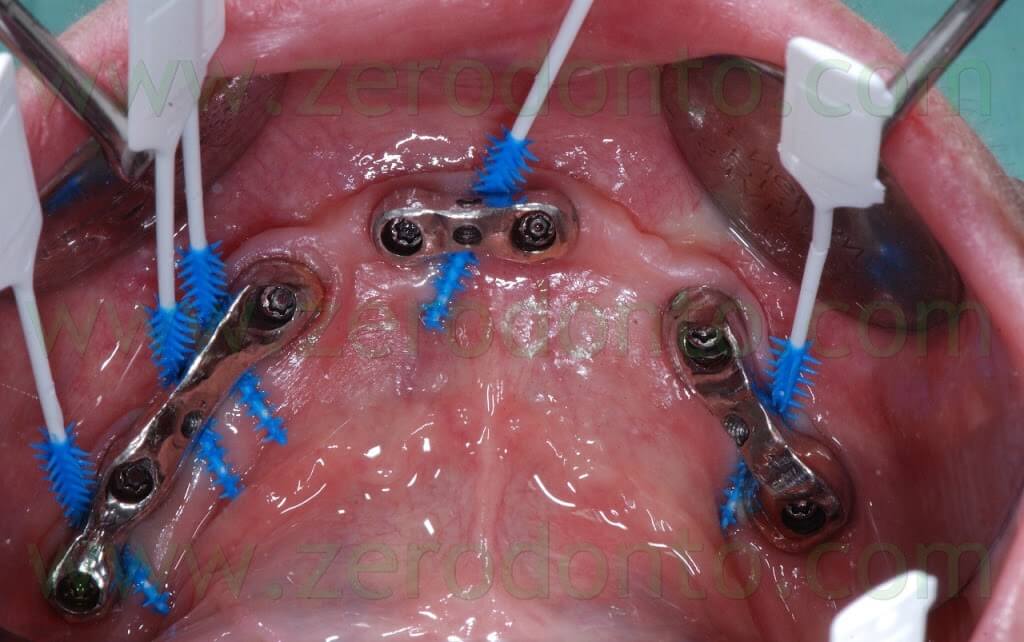
A first impression with screwed transfer copigs was made to fabricate a screw-retained fixed temporary prosthesis. In order to ease the following prosthetic procedures but respecting the restorative biomechanics, such temporary prosthesis weas screwed only onto 4 implants using a metal bar coated with veneering resin. The interim prosthesis was used to check the occlusal schemes, stability and functions for a satisfactory period of time.
Three months after the placement of the temporary full-arch bridge, the final prosthesis was fabricated.
A precision impression was made by means of a custom made light-curing resin tray. The open tray technique with a medium-body polyether was used. An adhesive for polyethers was applied in the impression tray.
The screwed impression copings were splinted with a dental wire and pattern resin, in order to reduce distortions due to polyether shrinkage and tray removal from the oral cavity.

The proper fit between impression copings and implants was verified by means of periapical radiographs.
Once the intraoral setting of the polyether was completed, the impression material was removed from the screw access holes of the impression copings with a blade and a dental explorer.
Although nowadays there are no clinical methods to verify the passive fit of a prosthetic structure onto implants, the precision of the impression was checked fabricating a resin bar screwed onto the implants. The one-screw test (Sheffield’s test) was used to try-in intraorally the resin bar; its fit onto the implants was evaluated both clinically under magnification and radiographically as previously described.
Then, 3 metal fixation cylinders were welded onto the bar to make a diagnostic wax-up of the shape and volume of the veneering materials, so as to check the intermaxillary relations and to perform the estetic and phonetic try-in.
Occlusal adjustments were transferred to the dental laboratory by means of pattern resin occlusal checks.
Then, 3 nobel alloy mesostructures screwed onto the implants were fabricated: 1 in the anterior region and 2 in the posterior areas. Each mesostructure was designed to hold a lingual screw to fix the prosthesis. The choice of a screw-retained prosthesis was due to its retrievability, since the patient did not want to reduce smoking.
The mesostructures were tried-in intraorally and the passive fit was evaluated as previously described.
Particular attention was devoted to the home hygienic maintainability of the prosthesis, allowing the patient to use implant brushes.
Once the diagnostic wax-up was accepted, a resin model of the final prosthesis was fabricated. A cut back of the thickness necessary to stratify the veneering ceramic was performed.
Then, the resin model was scanned and a CAD-CAM system was used to fabricate the zirconia framework.

Tapered occlusal screws with smooth head were used, in order to be settled in the metal mesostructures without creating any tensile stress in the zirconia framework. The head of each screw was cut according to the height requested by the functional needs and the esthetic veneering of the prosthesis.
A veneering ceramic with a coefficient of thermal expansion dedicated to zirconia was used. An anatomically-guided stratification of the ceramic was performed to reduce the risk of ceramic chipping; consequently, an even thickness of 0.6 mm of veneering ceramic was used. Moreover, the slow cooling of the ceramic was performed to dissipate residual mechanical and thermal stresses avoiding the formation of microcracks.
The insertion axes of the lingual screws were designed not to interfere with the tongue and the oral tissues, in order to facilitate the screwing of the prosthesis.
Moreover, the screw access holes were placed on the lingual area of the prosthesis; consequently, they did not alter either the occlusal morphology of the teeth of the functional paths studied in the articulator and verified with the temporary prosthesis.
The hygienic maintainability of the restoration was verified by means of implant brushes.
In order to finalize the treatment, the mesostructures were screwed onto the implants at 30 Ncm using a torque limiting dynamometric device following the manufacturer’s instructions. The screw access holes were filled with a light-curing composite resin. The proper fit of the implant components was verified both clinically and radiographically as previously described.
A silicone disclosing agent weas used to verify the adaptation of the mesostructures to the soft tissues: no pressure areas were identified. The prosthesis was screwed onto the mesostructures at 25 Ncm as reported above.
The chromatic integration of the prosthesis (Dental Technician Mr. Vincenzo Mutone) was rated as excellent by both the clinicians and the patient. Centric and non axial contacts were checked and adjusted.
At the 1-week follow-up, all the screws were tightened due to the settling under load.
Furthermore, static and dinamycal occlusal relations were checked, as well as the quality of periimplant soft tissues.
No flogosis was evidenced and the home hygienic maintenance was considered very satisfactory. The patient rated both the functional and the psychological comfort as excellent.
Although the clinical results were considered optimal, it is worth remembering that, to date, there is no evidence in the literature of the success of such long spam zirconia prostheses (just like full-arch bridges) in the long term. As a consequence, the clinical reliability of the restoration will be monitored over time.
The prosthetic design of the full-arch was performed according to the biological and mechanical standards described in the literature.
Nonetheless, such a one-piece zirconia framework could be affected by aging phenomena over time; consequently, further clinical follow-ups will be necessary to verify the effectiveness of the prosthesis in the long term.
As to the choice of a screwed restoration, it is worth remembering that the unscrewing of a prosthesis should not be considered a standard procedure (e.g. hygienic mainteinance) but only an option for retrievability in case of biological or mechanical complications. In fact, the routinary unscrewing of prostheses has been clearly related to loss of retention of screws.
REFERENCES
1. Zarone F, Russo S, Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent Mater. 2011 Jan;27(1):83-96.
2. Guess PC, Att W, Strub JR. Zirconia in Fixed Implant Prosthodontics. Clin Implant Dent Relat Res. 2010 Dec 22;Epub ahead of print
3. Larsson C, Vult von Steyern P, Nilner K. A prospective study of implant-supported full-arch yttria-stabilized tetragonal zirconia polycrystal mandibular fixed dental prostheses: three-year results. Int J Prosthodont. 2010 Jul-Aug;23(4):364-9.
4. Hjalmarsson L, Smedberg JI, Pettersson M, Jemt T. Implant-level prostheses in the edentulous maxilla: a comparison with conventional abutment-level prostheses after 5 years of use. Int J Prosthodont. 2011 Mar-Apr;24(2):158-67.
5. Dierens M, Collaert B, Deschepper E, Browaeys H, Klinge B, De Bruyn H. Patient-centered outcome of immediately loaded implants in the rehabilitation of fully edentulous jaws. Clin Oral Implants Res. 2009 Oct;20(10):1070-7.
6. Van de Velde T, Collaert B, Sennerby L, De Bruyn H. Effect of implant design on preservation of marginal bone in the mandible. Clin Implant Dent Relat Res. 2010 Jun 1;12(2):134-41.
7. Arvidson K, Esselin O, Felle-Persson E, Jonsson G, Smedberg JI, Soderstrom U. Early loading of mandibular full-arch bridges screw retained after 1 week to four to five Monotype implants: 3-year results from a prospective multicentre
study. Clin Oral Implants Res. 2008 Jul;19(7):693-703.
8. Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003 Sep-Oct;18(5):719-28.
9. Lee A, Okayasu K, Wang HL. Screw- versus cement-retained implant restorations: current concepts. Implant Dent. 2010 Feb;19(1):8-15.
For Information:
zerodonto@gmail.com
tel. 0039 081 2451805

