IMPLANT-SUPPORTED PROSTHETIC REHABILITATION WITH CONTROLLED BONE EXPANSION BY MEANS OF SONOSURGERY SONIC TIPS AND OSTWILL BONE EXPANDERS
In implant-prosthodontics, the prosthetically-guided implant placement is paramount: implants have not to be positioned where bone is present (as it was advised before bone augmentation techniques were introduced) but the oral surgeon has to place fixtures with shape and dimensions proper to substitute the missing teeth. Moreover, correct emergence profiles as well as proper mesial-distal and buccal-palatal position have to be achieved, in order to dissipate occlusal loads evenly, mainly along the long axis of implants.
Horizontal bone resorption occurring after the extraction of a tooth is one of the most frequent anatomical limitations that do not allow the ideal placement of an implant. Sometimes, although the buccal-palatal amount of bone seems to allow a proper positioning of a fixture without bone augmentation, such horizontal resorption moves the center of the ridge palatally in the upper jaw and buccally in the lower jaw. Implant placement without correcting such conditions would probably result in a wrong emergence profile of the prosthesis.
One of the most predictable regenerative technique to improve the amount of buccal bone is the sagittal osteotomy of the ridge (E.R.E.), developed by Dr. Bruschi and Dr. Scipioni. Such technique was reported to have very high success rates (98-100%) and showed the minimum volumetric contraction in the long-term, since the buccal bone is maintained in situ provided with both endosteal and periosteal blod vessels, limiting secondary bone resorption.
In the present clinical case, a patient needing a single implant in region 13 was treated; the tooth was extracted one year before implant treatment because of severe periodontal damage.


The premolar had been previously endodontically treated and restored by means of a glass fiber post. The patient was wearing an acrylic resin temporary restoration luted on tooth 14 with a cantilever in region 13. The provisional restoration was considered incongruous because of both esthetics (too light color) and function (absence of the mesial contact area).


A severe buccal-palatal bone resorption was evidenced in the implant site; consequently, it was decided to use the split-crest technique, in order to improve bone thickness and restore the original bone morphology due to the presence of the canine root.

A cut was made in the center of the ridge, extending distally with an intrasulcular cut at level of the 15 and a release cut at level of the 12. A total thickness flap was elevated.
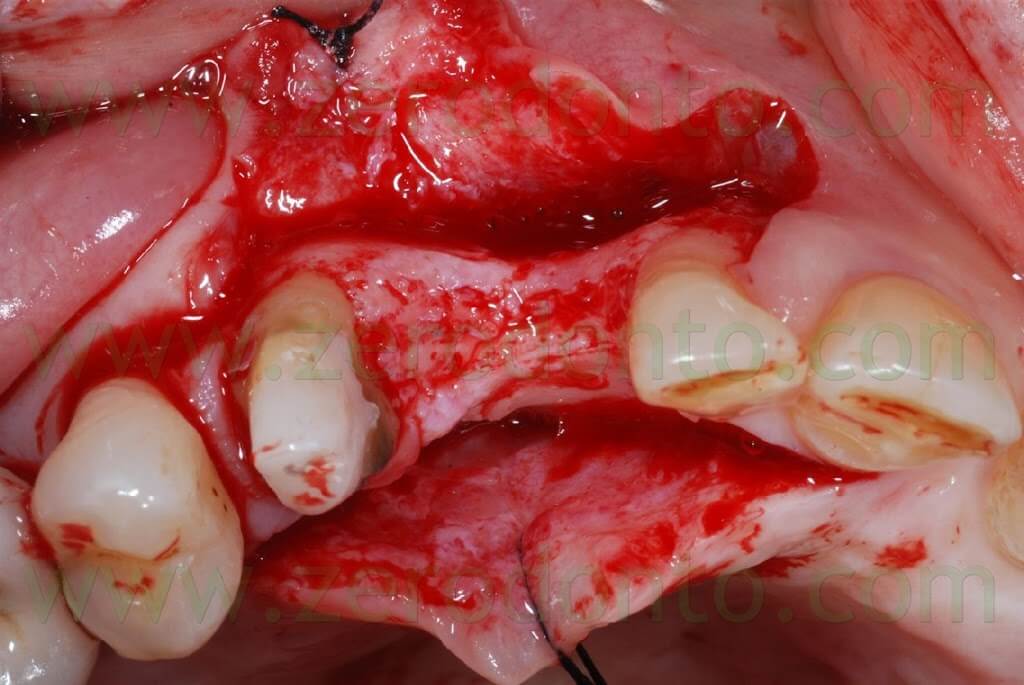

Such a cut with an internal bevel on the 14 will allow to thin the flap on the premolar, so that in the healing phase the soft tissues will creep over the preparation margin, establishing a correct biologic width.
The position of the ridge cut is paramount and has to be planned considering the implant diameter, which will be placed in contact with the palatal bone, since the buccal segment will be moved.
The Sonosurgery sonic tips (Komet) developed by Dr. Agabiti mounted on the Sonicflex device (Kavo) were used for the split-crest.
By means of these instruments which use the microvibrations of the sonic movement, it is possible to achieve 0.2 mm thick cuts with an optimal control and a minimal traumatism to the bone. A greater amount of bone is consequently preserved and this could be paramount for the long term success of the treatment.

The Sonosurgery sonic tips are produced in 3 shapes which allow to reach comfortably all oral regions.
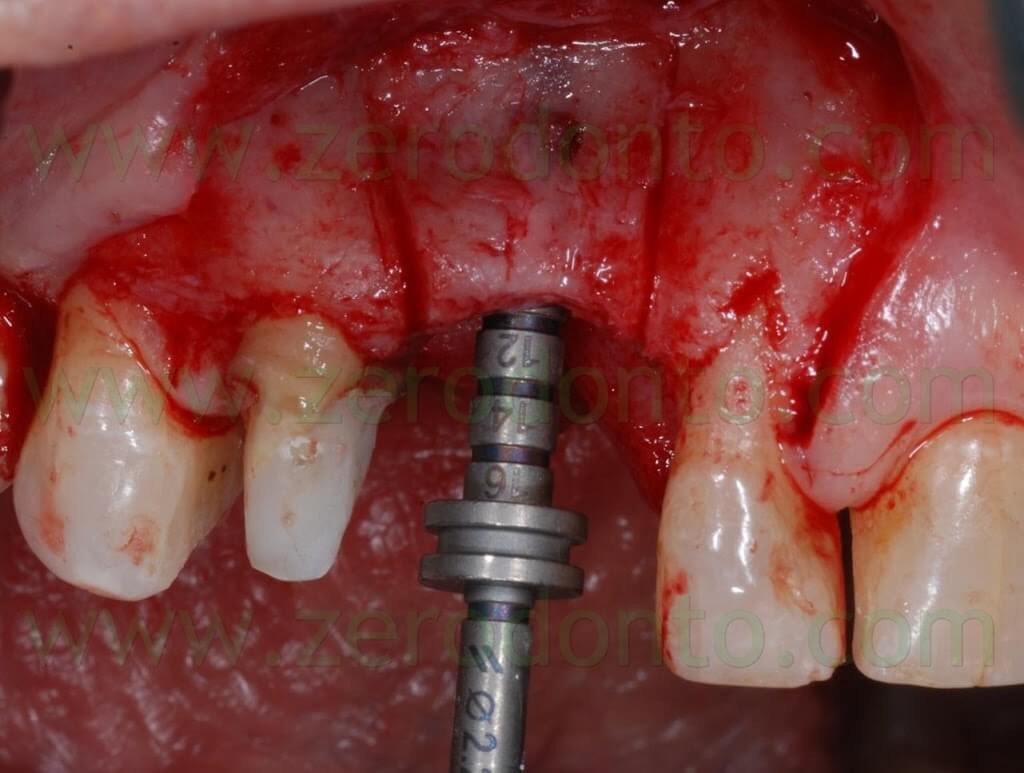
A 10 mm deep cut was made in the center of the ridge using a flat blade.
Then, an orthogonal blade was used to perform two vertical cuts on the buccal aspect of the ridge, reaching the primary horizontal cut. In this way, a piece of bone was cut and moved buccally, maintaining an anatomical and functional continuity with the apical part of the ridge.
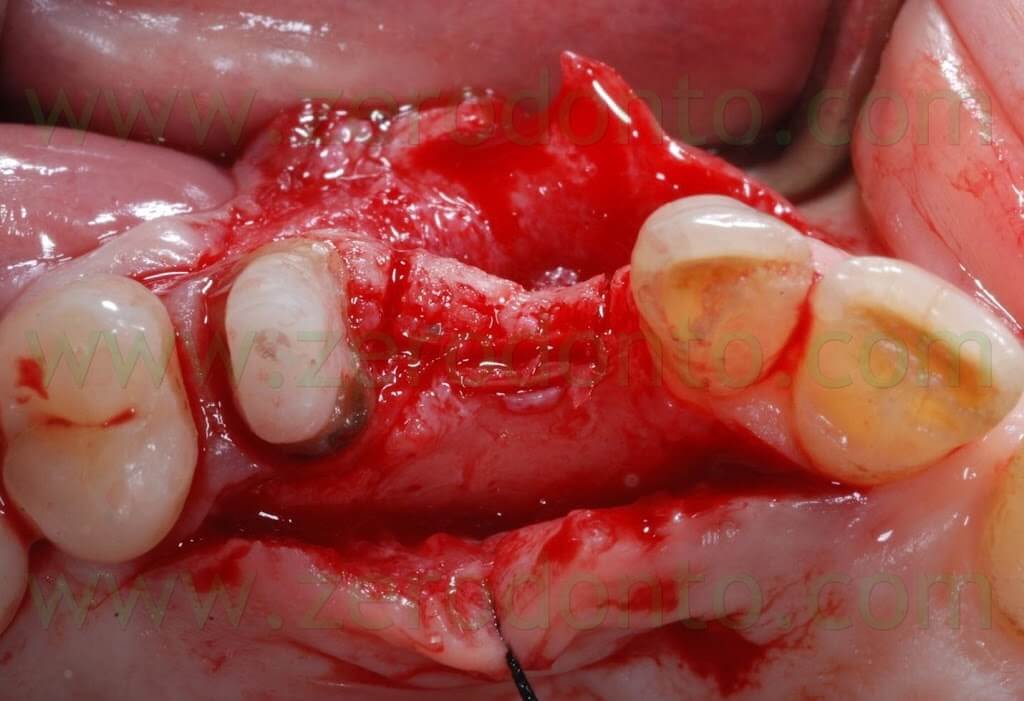

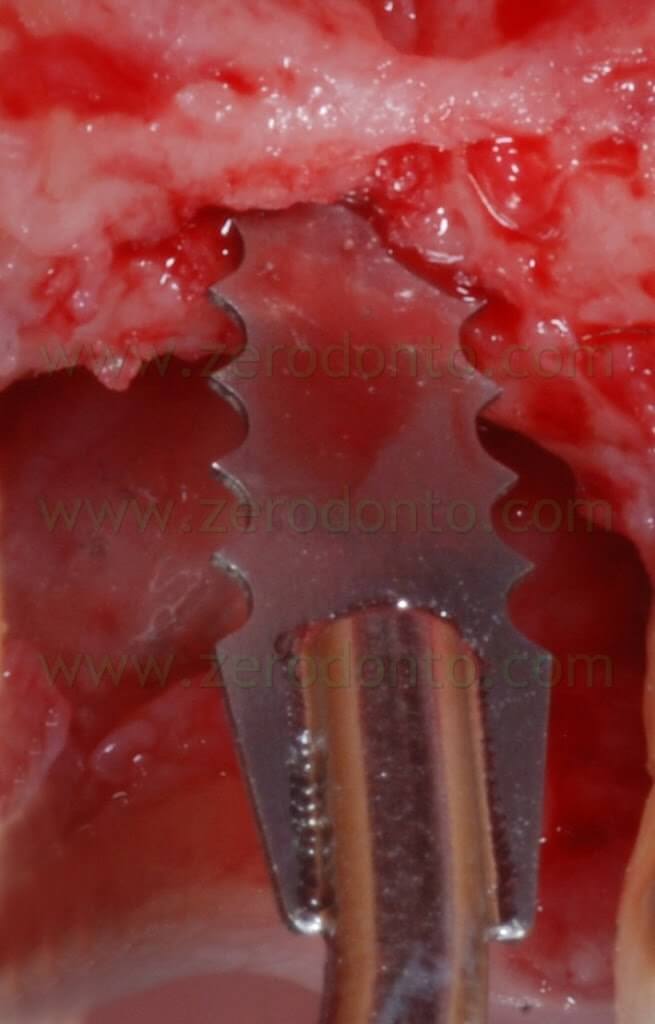

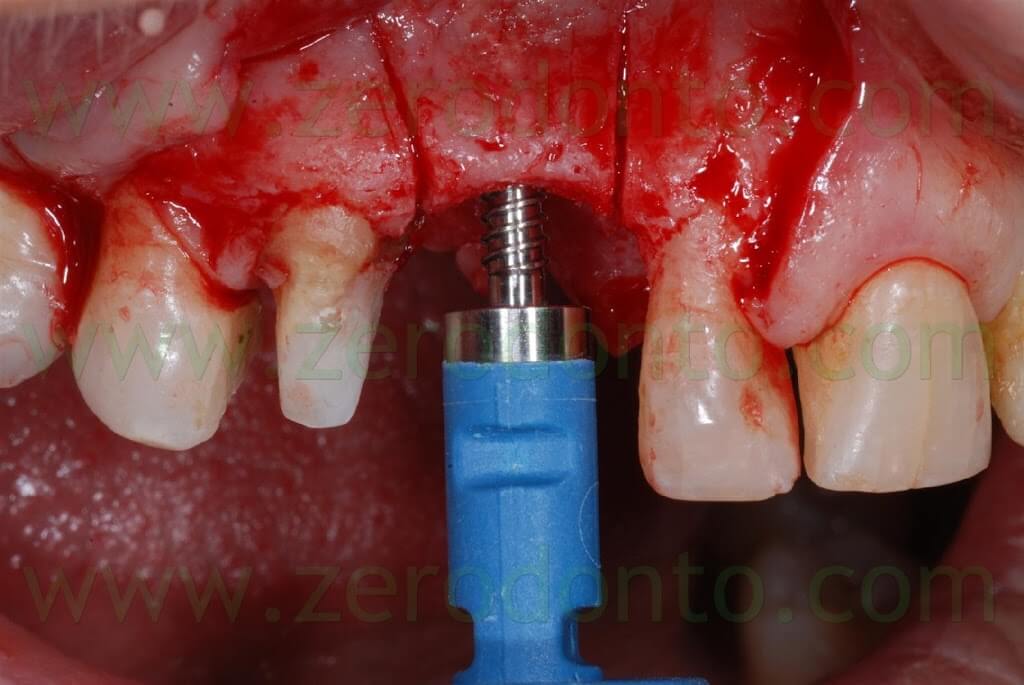
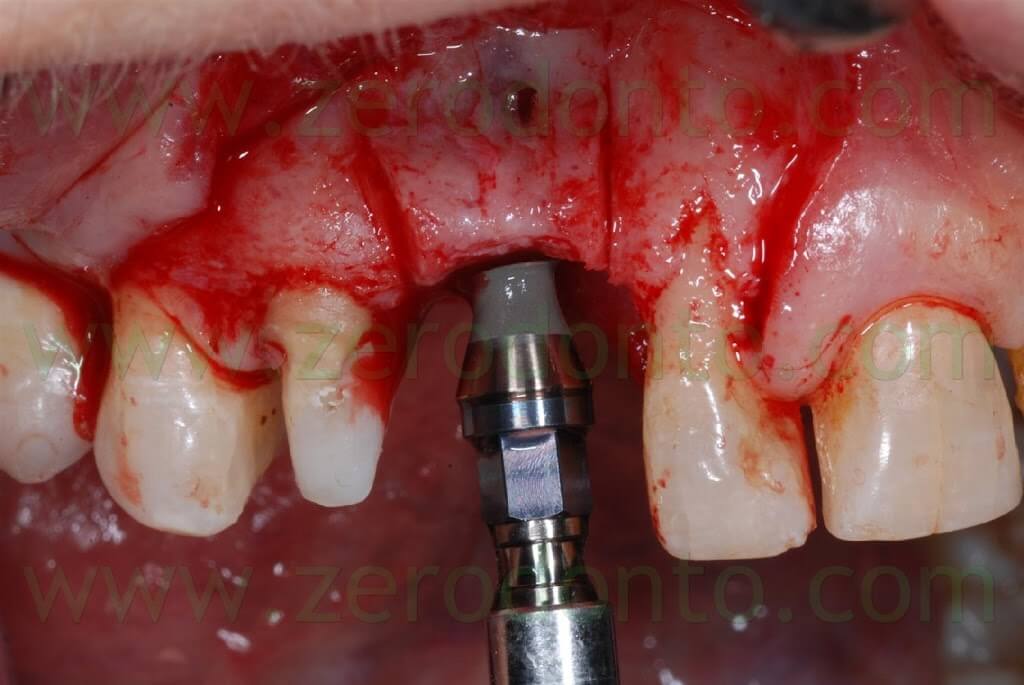
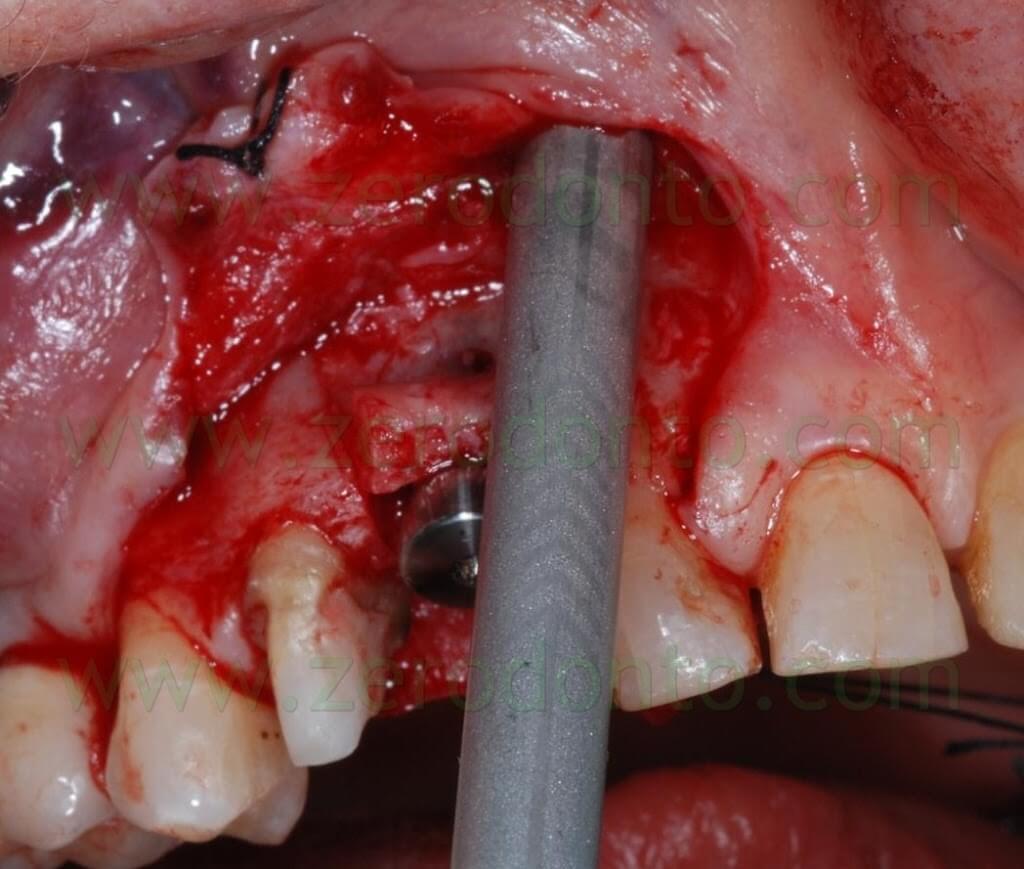
A first guiding hole to place the implant was created using a rounded bur and a 1.2 mm bur; then, further space was created by means of Ostwill bone expanders (Meta).

Such bone expanders are conical screw-shaped instruments with increasing diameters. They are slowly activated manually rotating the screw under constant irrigation of physiological solution until bone resistance is met: this results in a controlled bone expansion, avoiding the risk of fracture the bone piece.
After 20-30 seconds, a new activation is performed. Regular pauses are paramount, since the described surgical procedure is performed respecting the viscoelasticity of the bone. During such pauses, in fact, trabecular liquids are redistributed in intratrabecular spaces, reducing the risk of buccal bone fracture.
Each screw rotation corresponds to a bone expansion of about 0.2 mm.
A dynamometric device allows to control bone resistance and applied force, in order to decide when to pause before any further activation.

Sometimes, a few minutes could be necessary to allow intratrabecular fluids to redistribute, reducing bone resistance.
If the described technique is used, it is advisable to elevate a full thickness flap in order to control the occurrence of bone dehiscences or fenestrations; in these cases, bone augmentation procedures are necessary to prevent the fracture of the buccal bone.

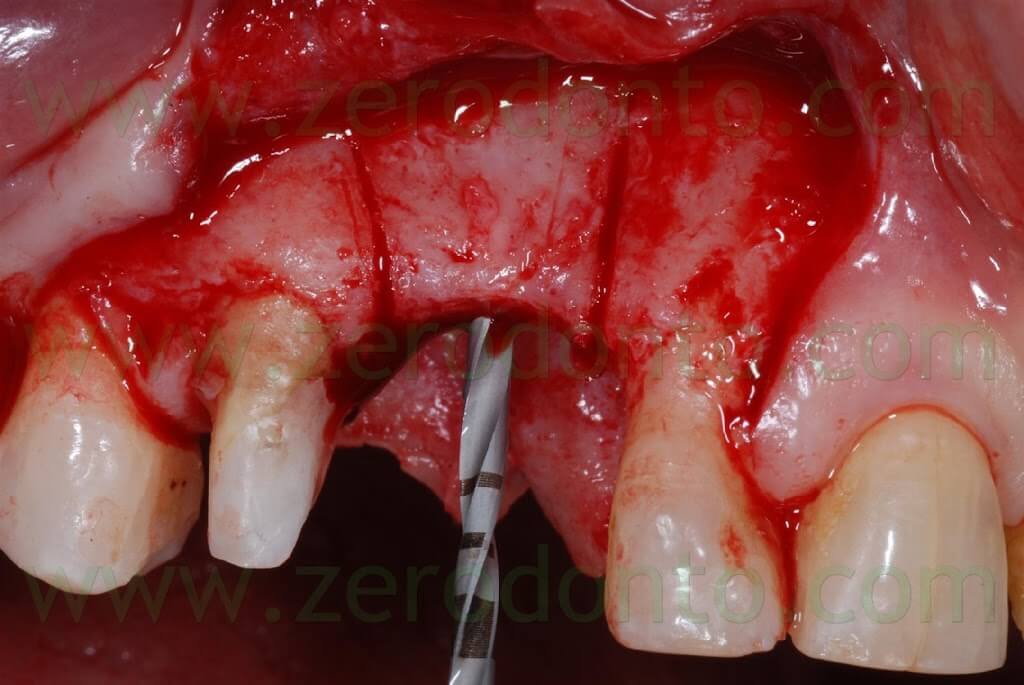
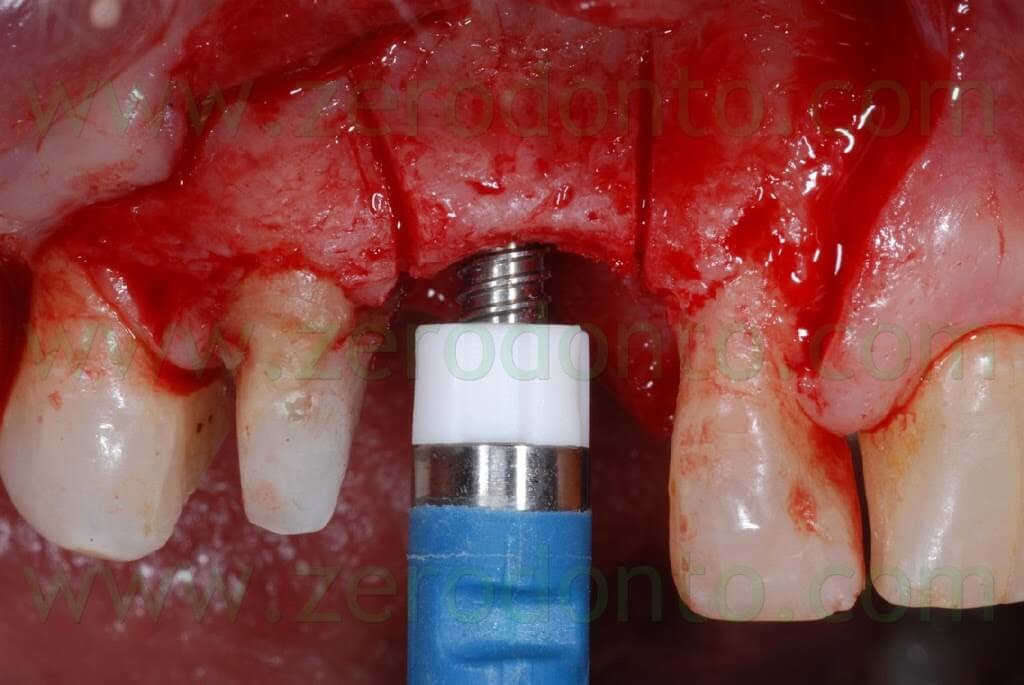
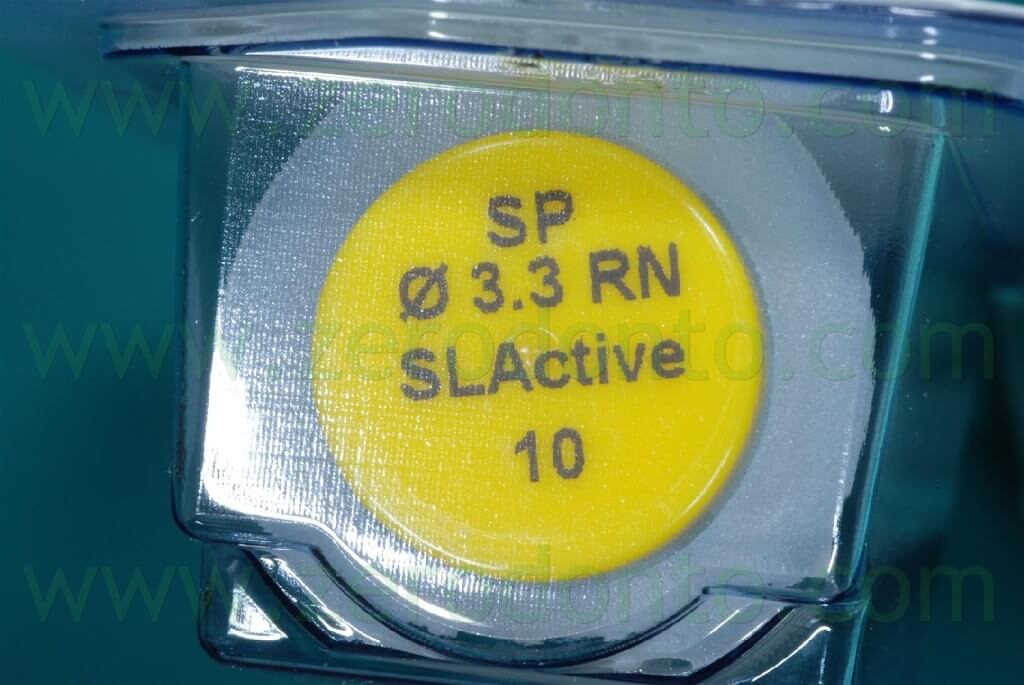
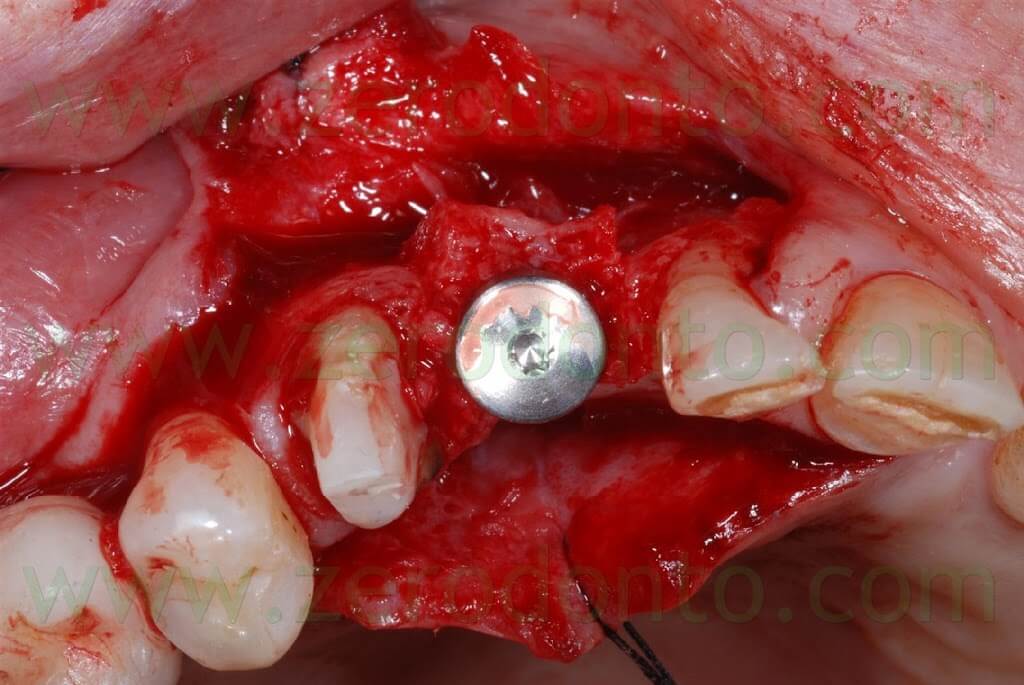
A SLActive Standard Plus (with smooth neck) Straumann implant 3.3 mm in diameter and 10 mm in length was used and placed 2 mm more apically because of esthetic reasons.
The SLActive surface makes osseointegration faster, allowing to load the fixture in the upper arch 6 weeks after surgery.

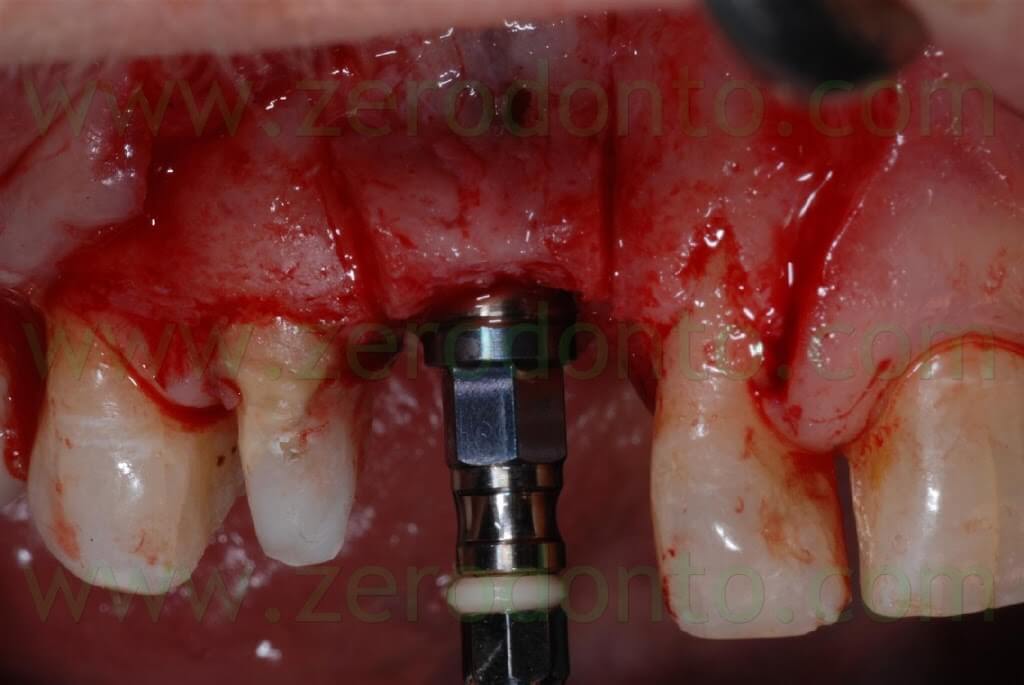
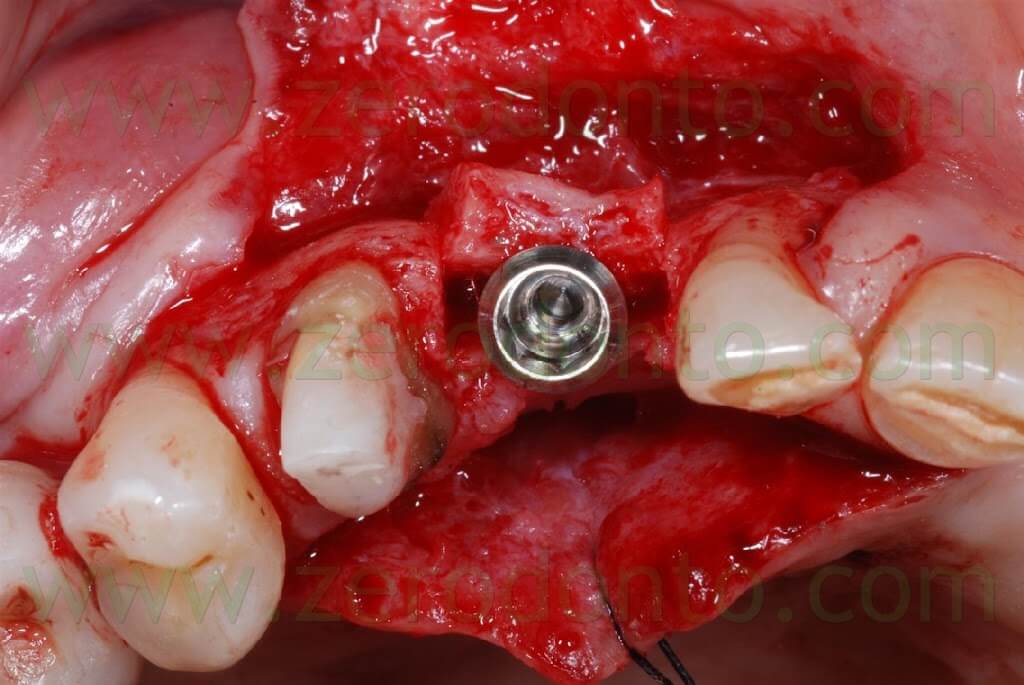
A covering screw with a diameter of 3 mm was used to shape the transmucosal region.
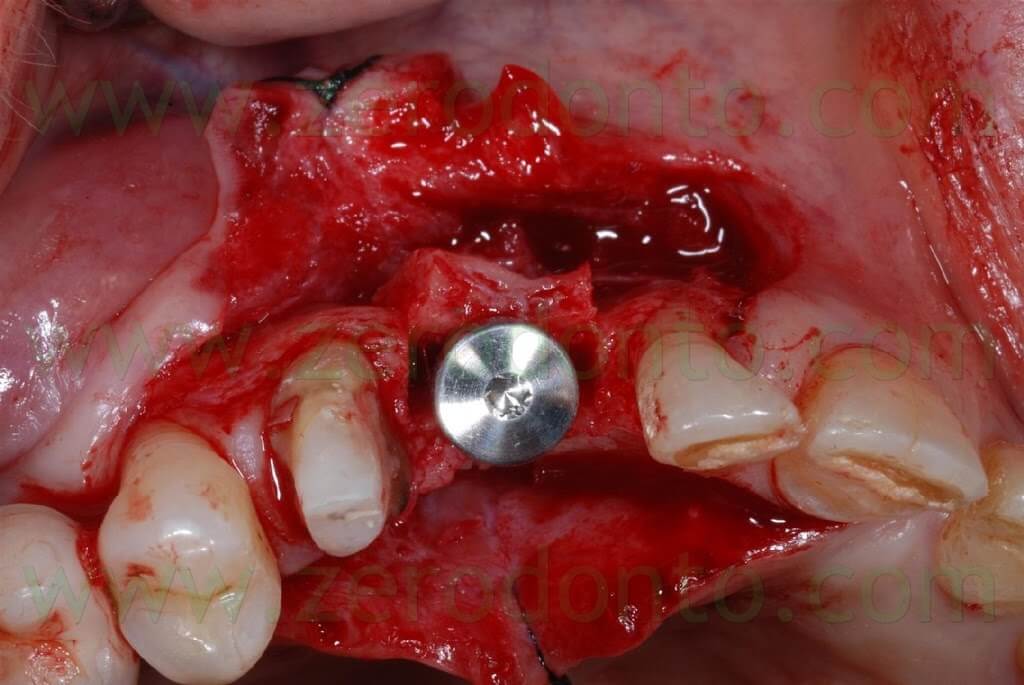

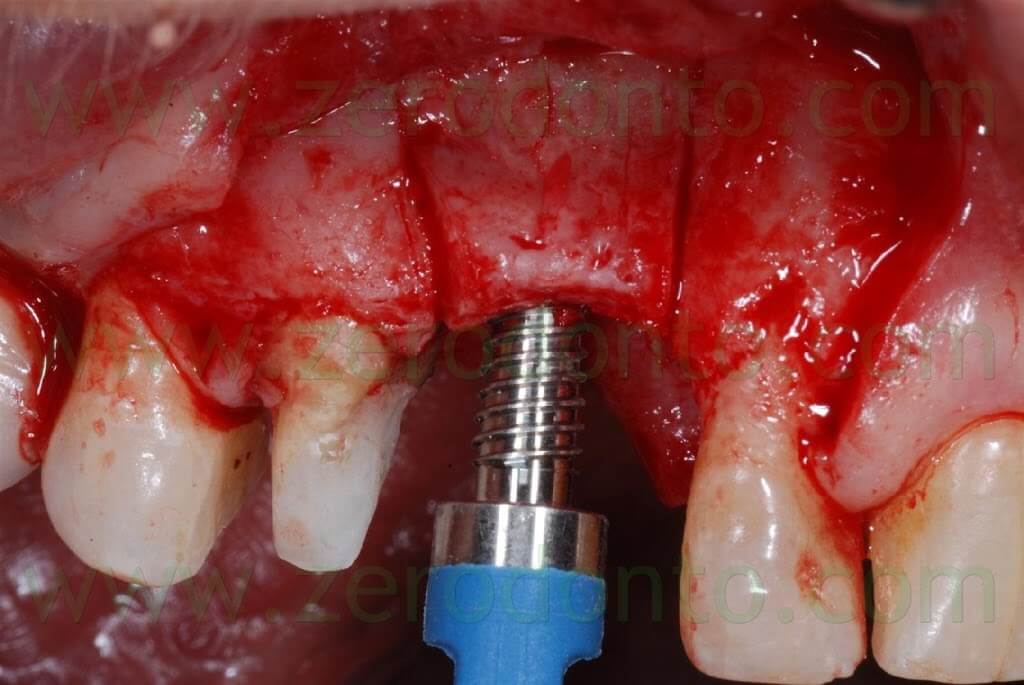
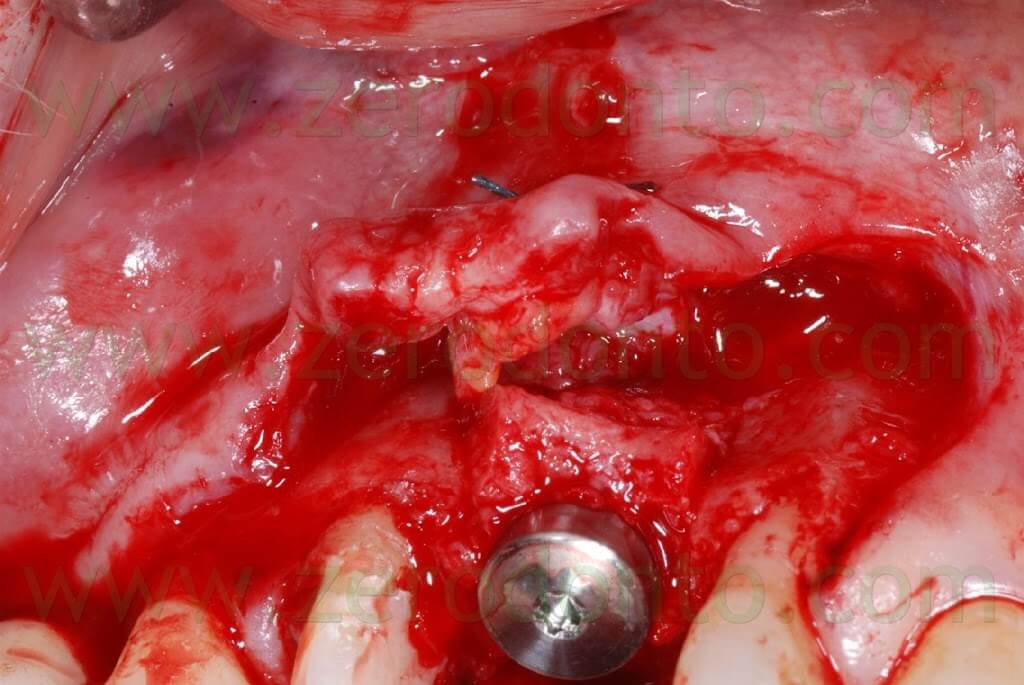
The 2-3 mm gap created between the buccal and palatal bone after the split crest was filled using bone chips taken by means of a Micross bone scraper (Meta) from the same implant site, apically to the fixture.


Connective tissue was taken from the palatal aspect of the flap and grafted buccally to make the soft tissues thicker, changing the biotype and making such tissues stable in the long-term.

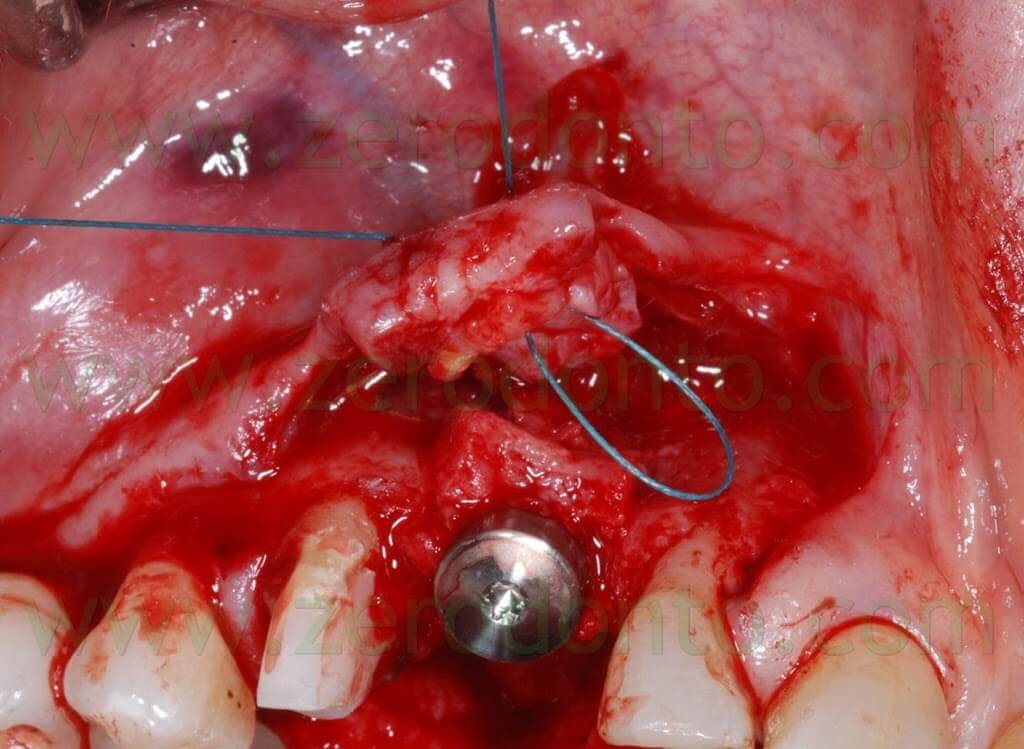
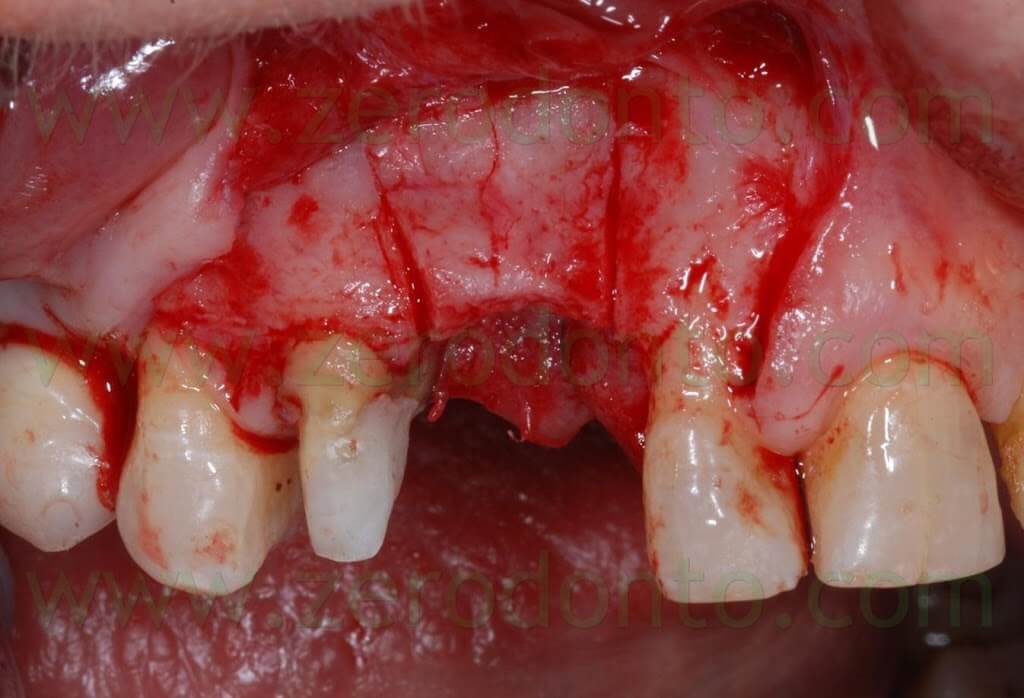
A 4.0 Tevdek multithread polyester wire covered with ePTFE was used to suture the surgical site.

Once the surgery was completed, the preexisting temporary restoration was modified in order not to be in contact with the implant, avoiding micromovements interfering with osseointegration. The provisional restoration was relined with acrylic resin to shape a proper mesial contact area. Both centric and non-centric occlusal contacts were checked, in order to avoid overload of the restoration.
The suture was removed two weeks after surgery. A new metal-reinforced acrylic temporary restoration with a mesial wing was made after 2 more weeks.


As received by the dental laboratory, such provisional restoration was in contact with the covering screw; consequently, its cervical shape was modified as previously described, in order not to interfere with the healing process. At level of the 14, the tooth preparation was modified and corrected, placing the finishing line iuxtagingivally. The temporary crown was relined using autopolymerizing acrylic resin and polished. One month after surgery, optimal healing of soft tissues was noticed with an evident creeping over the prosthetic margin.




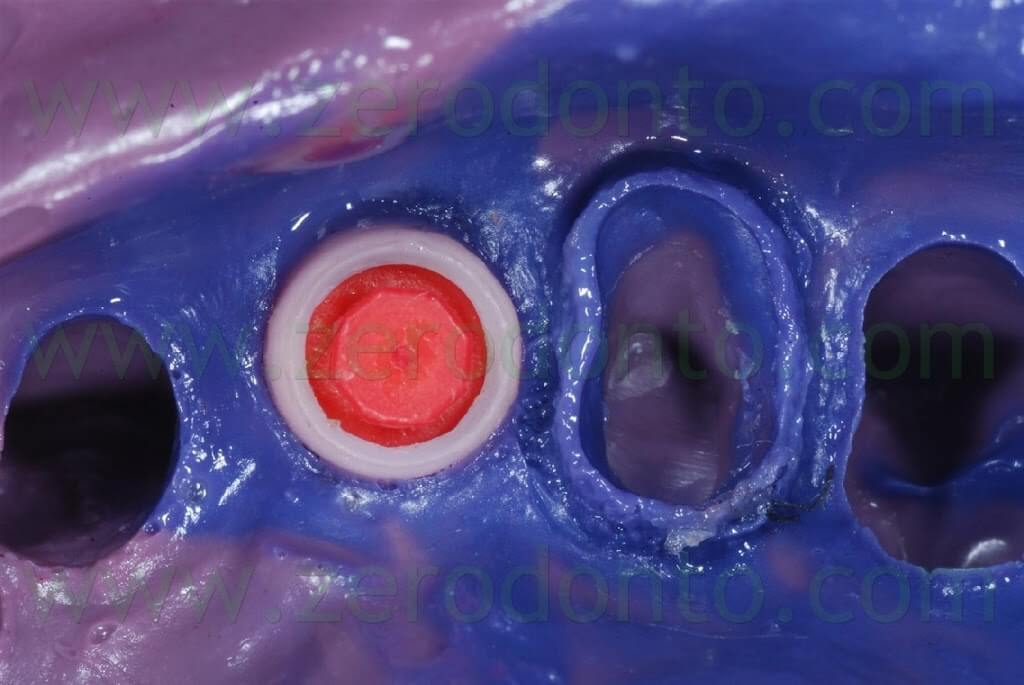
After 3 months, the final impression was made on both tooth and implant by means of light and medium consistency polyether impression materials. On tooth in position 14 two retraction chords were placed to make the impression whereas a snap-on transfer coping was used on implant in position 13.





After the conventional prosthetic try-in procedures, the case was completed. A 15° angled titanium implant abutment was used to make the emergence profile consistent with that of the tooth supported restoration. Two single-unit metal frameworks were made and tried intraorally.




Similarly, a try-in of the ceramic was performed to check both esthetics and function. The color resulted too light, consequently darker areas at the cervical margin of both crowns were realized.


The tooth-supported single crown on the 14 was luted using a glass-ionomer cement whereas the implant-supported single crown in region 13 was luted by means of a resin temporary cement, because of the optimal retention guaranteed by the industrially machined implant abutment.
Soon after the cementation, no papilla filled the space between the restorations.


After 3 weeks, good emergence profiles and an evident creeping of the soft tissues were noticed and the interproximal space resulted partially filled. At the 1 year follow-up recall, such space was almost completely filled, although the patient presented soft tissue abrasions due to wrong brushing procedures.

Once the trauma was eliminated motivating the patient to a correct oral hygiene, complete healing of the soft tissues was observed after 3 weeks.




Bibliography
Scipioni A, Bruschi GB, Calesini G.
The edentulous ridge expansion technique: a five-year study.
Int J Periodontics Restorative Dent. 1994 Oct;14(5):451-9.
Scipioni A, Bruschi GB, Giargia M, Berglundh T, Lindhe J.
Healing at implants with and without primary bone contact. An experimental study in dogs.
Clin Oral Implants Res. 1997 Feb;8(1):39-47.
Jensen OT, Cullum DR, Baer D.
Marginal bone stability using 3 different flap approaches for alveolar split expansion for dental implants: a 1-year clinical study.
J Oral Maxillofac Surg. 2009 Sep;67(9):1921-30.
Chiapasco M, Ferrini F, Casentini P, Accardi S, Zaniboni M.
Dental implants placed in expanded narrow edentulous ridges with the Extension Crest device. A 1-3-year multicenter follow-up study.
Clin Oral Implants Res. 2006 Jun;17(3):265-72.
Blus C, Szmukler-Moncler S.
Split-crest and immediate implant placement with ultra-sonic bone surgery: a 3-year life-table analysis with 230 treated sites.
Clin Oral Implants Res. 2006 Dec;17(6):700-7.
Demarosi F, Leghissa GC, Sardella A, Lodi G, Carrassi A.
Localised maxillary ridge expansion with simultaneous implant placement: a case series.
Br J Oral Maxillofac Surg. 2009 Oct;47(7):535-40. Epub 2009 Jan 15.
For information:
zerodonto@gmail.com
tel. 0039 081 2451805

