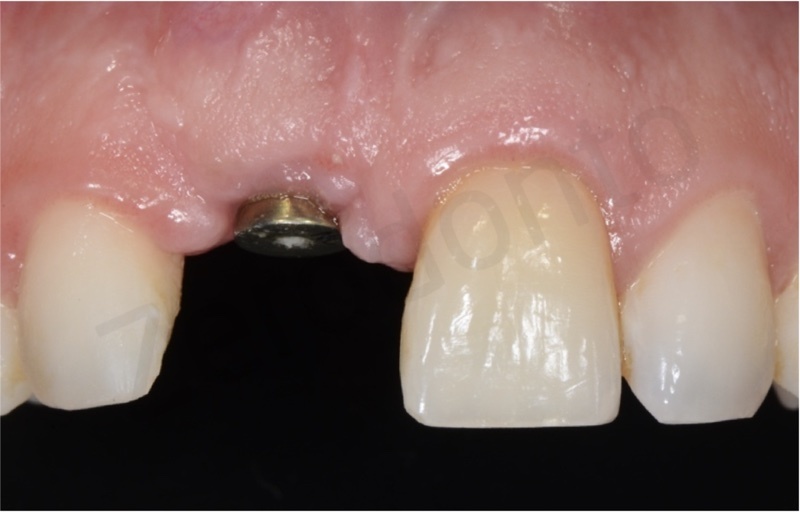
A 42-year old male patient with good general health presented with a severe gingival recession on tooth 11 causing a significative asymmetry of the smile.

Although he was interested by several minor problems (incongruous previous restorations, slight gingival recessions in other areas), the patient explicitly asked for the substitution of the right maxillary central incisor and the treatment of the maxillary anterior teeth crowding.

At the visual and radiographic inspections, tooth 11 was affected by a serious apical migration of the gingival margin and by internal and external root resorption caused by a previous wrong root canal treatment and placement of a preformed metal post.
The tooth was considered hopeless and it was planned an implant-supported prosthetic rehabilitation; in order to optimize the management of soft and hard tissues, an orthodontic preparation was requested to perform a slow extrusion of the jeopardized tooth, so as to recover mucosal and bone tissues as well as to solve the anterior crowding.
ORTHODONTIC TREATMENT
The patient desired to recover an acceptable aesthetic condition, requiring an orthodontic treatment solution both invisible and very comfortable, without phonetic disorders. For this reasons, a bracketless fixed lingual orthodontic treatment was proposed.
The appliance was made by a 0.0175 inches multistranded stainless steel wire, commonly used to model passive fixed retentions.


To obtain an extrusive movement, such retainer was modeled according to teeth anatomy with two vertical bends, particularly two U-loops. These vertical bends, just like bends on the horizontal plane, increase the elasticity of the wire. The wire was modeled intraorally but the authors suggest to beginners to perform this procedure on casts.

The bonding procedure is conventional and needs cleaning of dental surfaces, etching of dental areas to be bonded and bonding agent application. Then, after light curing, pre-activated retainers are applied by means of flowable composite resins. It is paramount to follow a precise bonding sequence to obtain a correct force transmission. In particular, in the present case it was very simple as the only rule to be respected was to bond the tooth to be extruded at last. The extrusion was activated modifying the vertical position of the wire, moving it in a more apical position with the use of a utility tool. The elastic return of the wire in the original coronal position will move the tooth in the desired direction.

Proper biomechanical principles have to be strictly followed during retainer activation, considering not only the device to be used but also the point of force application in respect to the center of resistance.

When buccal braces are used, the extrusion movement is almost always accompanied by a moment moving the crown in buccal direction, as the force is applied in a more buccal point then the center of resistance. Conversely, when lingual braces are applied, the force will almost always pass through the center of resistance and it will be easier to have a bodily tooth extrusion. Moreover, when the orthodontic device is on the lingual aspect but it is bracketless, its position may change in respect to the center of resistance and could be more lingual or buccal. Furthermore, in order to activate the extrusion, the wire has to be displaced from a more coronal to a more apical point but also from a more buccal to a more lingual point. Therefore, the elastic return will produce the extrusion of the tooth accompanied by a buccal moment.
Finally, during retainer activation, the expansive force generated by the loops should also be considered. If such buccal moment is not desired, it must be controlled with opposite forces.
In the present case, both extrusion and lingualization were activated to obtain a bodily extrusion of the tooth, first moving lingually the wire with a Weingart plier and then moving it apically with a utility tool.


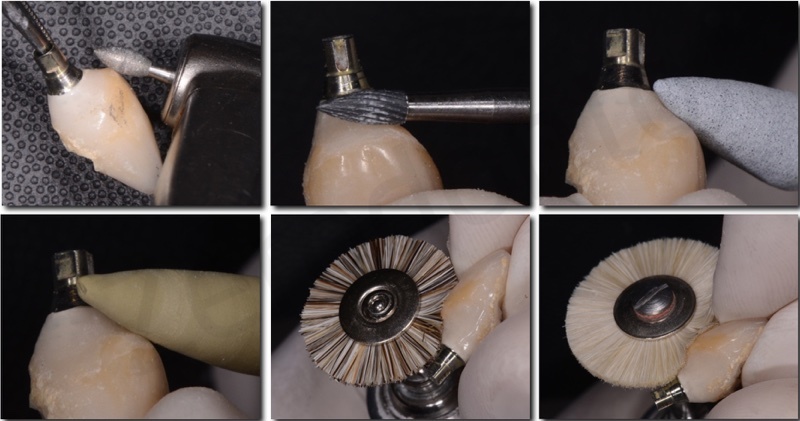
The device was checked every 4 weeks and reactivated. The reactivation was performed by detaching the wire from tooth 11 and consuming almost the entire composite layer covering it by means of a diamond bur at low speed under water irrigation, taking care not to damage it; to do this, the authors suggest cylindrical or ball-shaped burs. The last layer of composite was detached using a dental explorer as a lever under the wire, to detach it without any damage deriving from the bur. After detachment, it is possible to change wire position and shape, in order to obtain the desired displacement (in the present case always in lingual and apical directions) and then to bond the retainer again as previously described.


During reactivations, the etching procedures are always performed on surfaces already covered by a thin composite layer; therefore, the enamel is not repeatedly etched. If the identification of the composite area on teeth is difficult, a Wood’s light can be used to highlight it. Simultaneously to extrusion, the incisal margin reduction was performed, in order to level the margin with the contralateral central incisor.


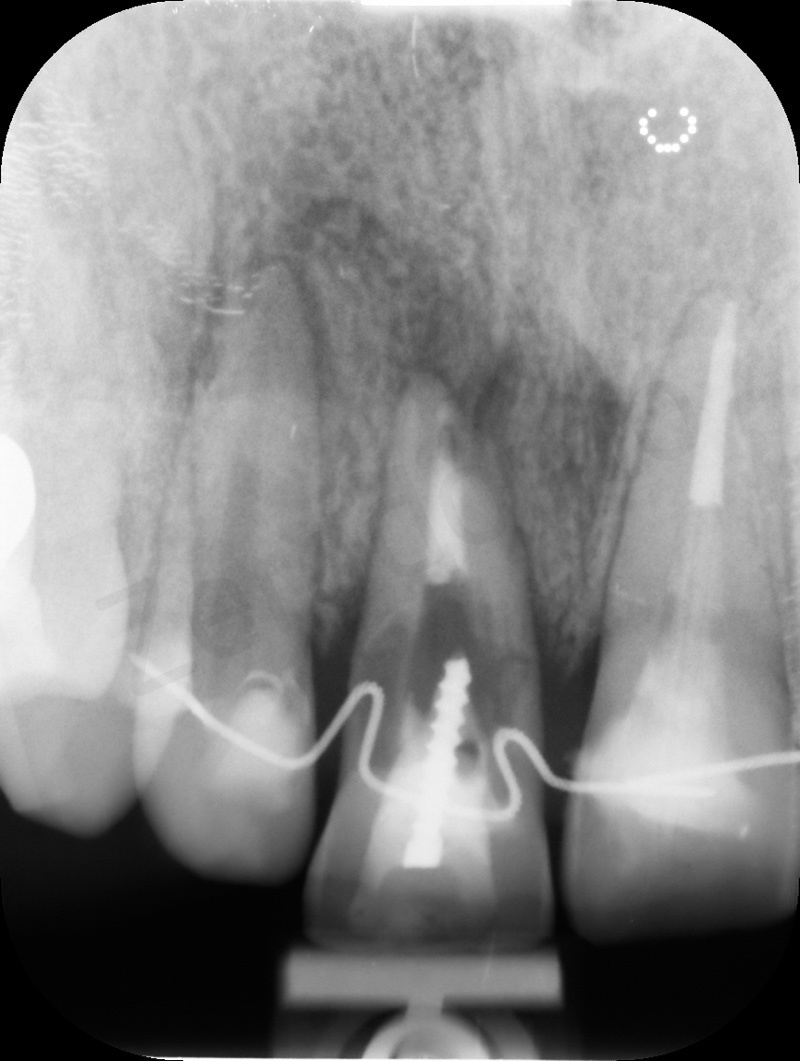
The intraoral x-rays show the coronal displacement of the root apex of tooth 11. The extrusion was obtained with approximately 5 activations and was performed in excess, in order to provide more hard and soft tissues for the subsequent periodontal and prosthodontics procedures.
IMPLANT-SURGERY TREATMENT
As regards multidisciplinary treatments, both surgery and orthodontics have to be finalized for prosthodontics, so implant placement and teeth movements, hard and soft tissues management have to be prosthetically guided in order to achieve functional and esthetical success.
As reported before, in the present case a resorption of the root of tooth 11 due to a previous internal bleaching caused the loss of the buccal and palatal cortical bone. Consequently, if the tooth was removed immediately, it would result in a vertical defect very difficult to be faced.

By means of a slow orthodontic extrusion, in a first stage it will be observed the reduction of the pocket depth and then the bone and soft tissues will move coronally.
The extrusion movement determines a progressive reduction of the radicular diameter; consequently, on one side it will contribute in solving the vertical bone defect whereas on the other it will cause an horizontal bone minus that will be easier to be managed.




In order to limit as much as possible the bone loss subsequent to tooth extraction, a socket preservation technique was performed. To date, no clinical study proved this technique to keep completely the post-extraction alveolus; however, the systematic review by Vignoletti et al. (2012) showed that post-extraction sites not treated by means of preservation techniques usually collapse 1.47 mm vertically and 1.84 mm horizontally more than socket preserved areas. Furthermore, the horizontal component is the one that takes more advantage from such approach.
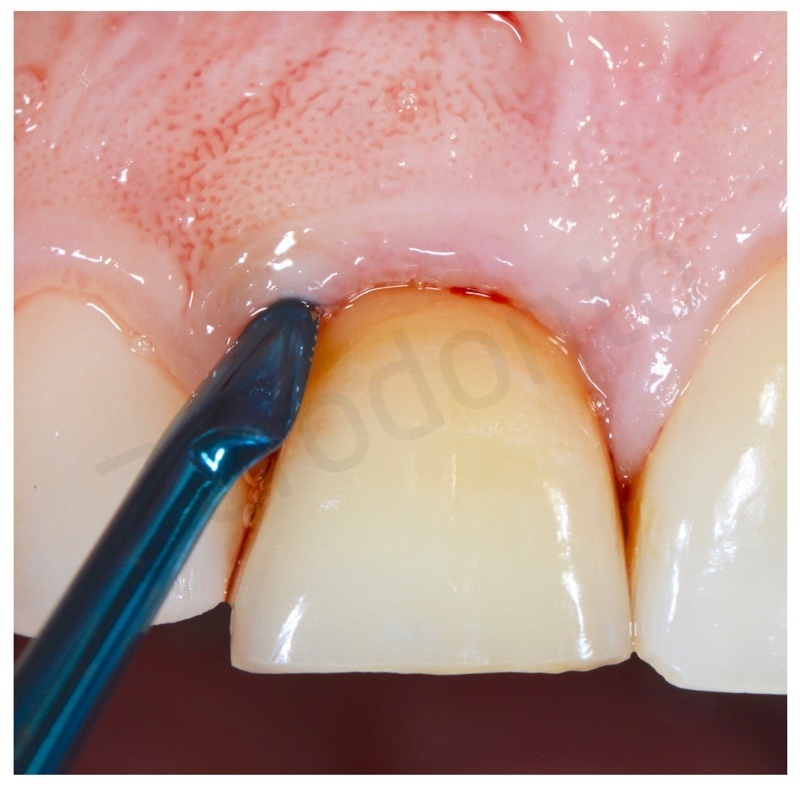
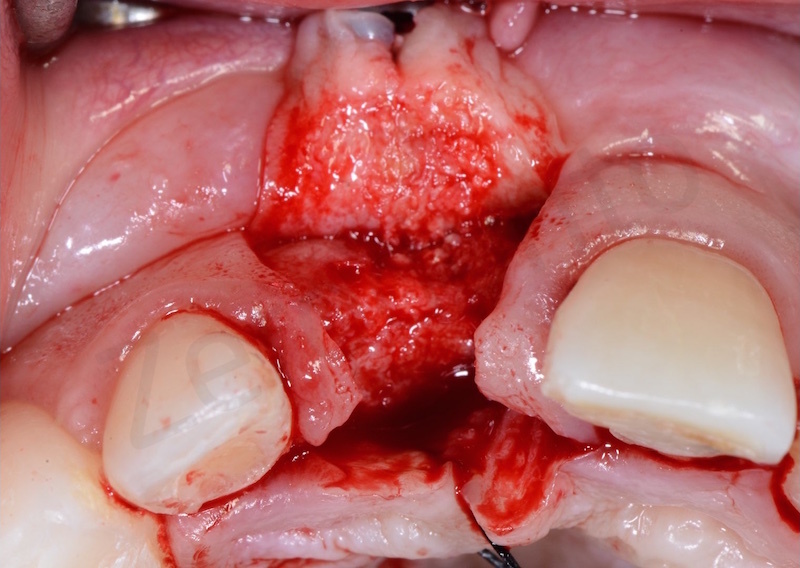
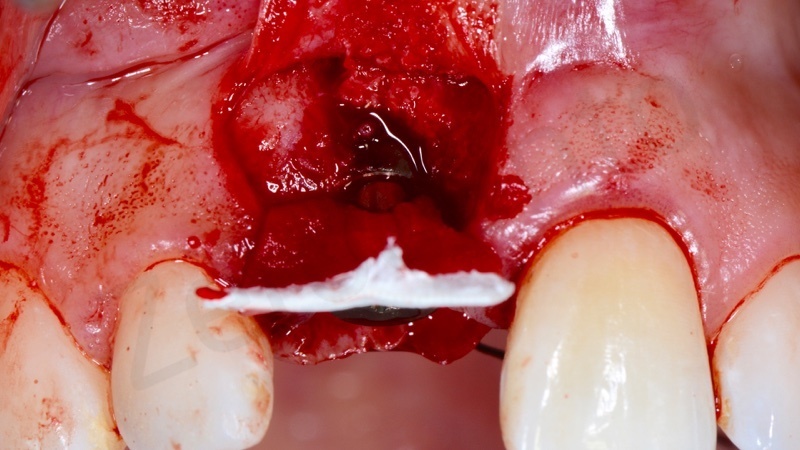
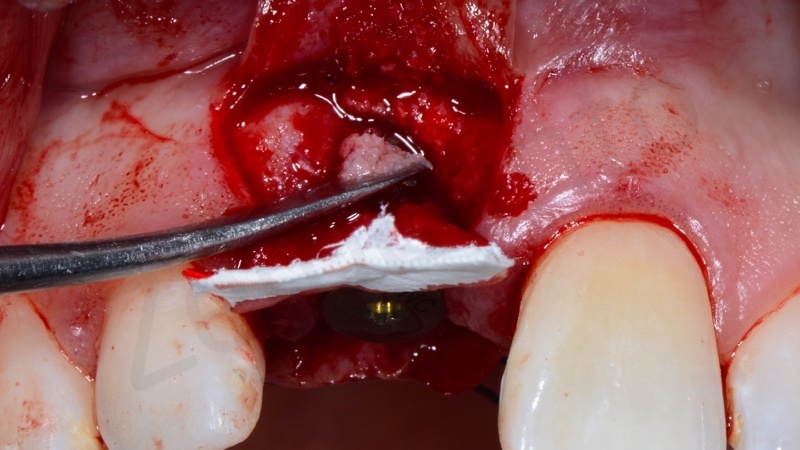
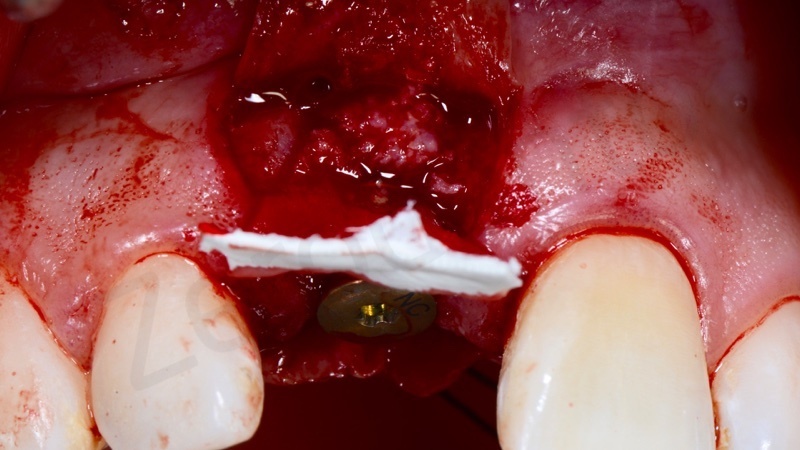
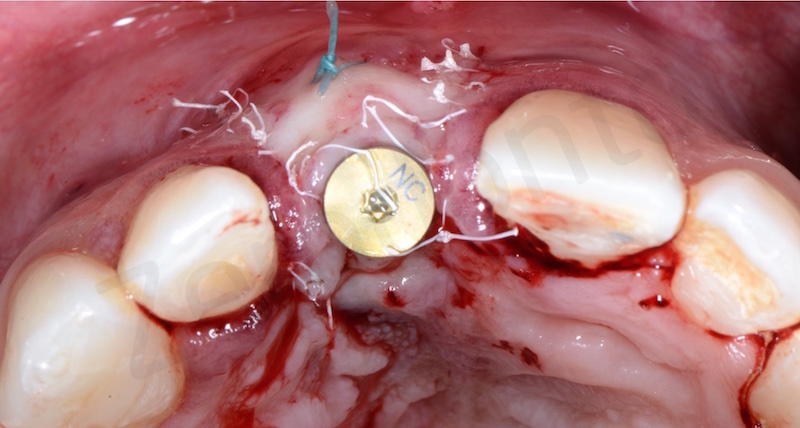
After performing an atraumatic extraction, a careful debridement of the bone defect was made; then, the sulcular epithelium was removed by means of a surgical blade and slow diamond burs.

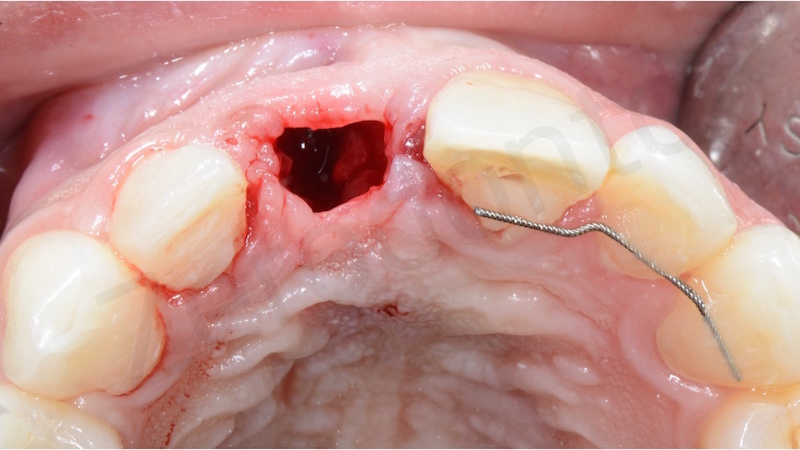
Once the inflammatory remnants were thoroughly cleaned, a block of bovine spongy bone and 10% porcine collagen was inserted into the socket. The bone graft was condensed up to the cortical level.
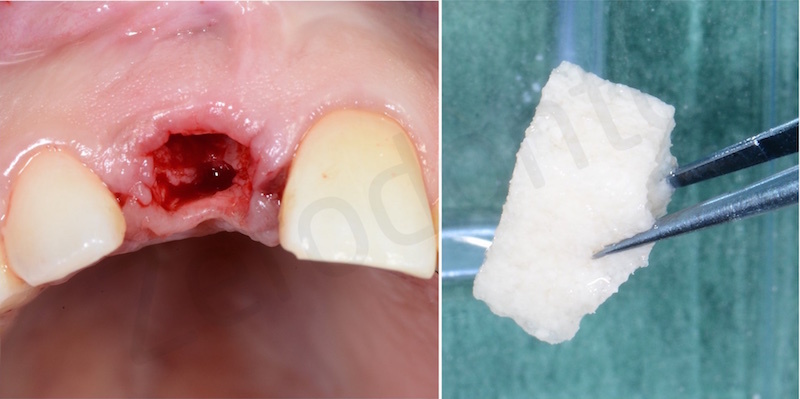





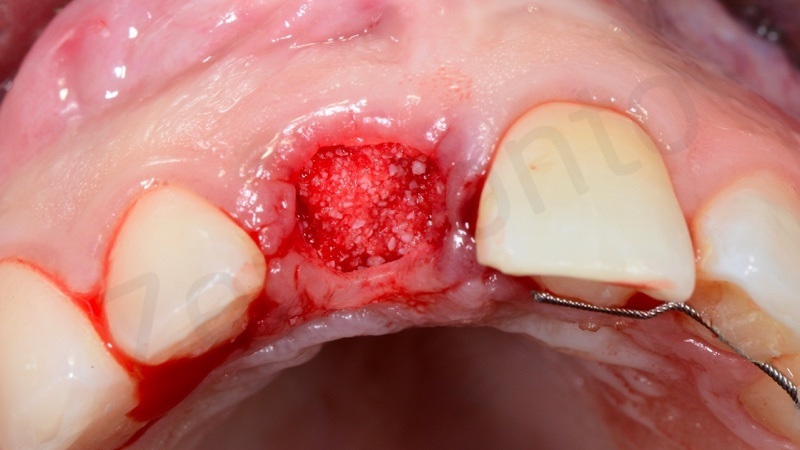
Then, a liquid resorbable membrane was used (Membragel, Straumann) to protect the graft; once it solidifies, such membrane stabilizes the bone substitute and offers a barrier effect lasting for 4-6 months.


Finally, a double stabilization suture was made.
Later on, the site was ready to receive the implant.


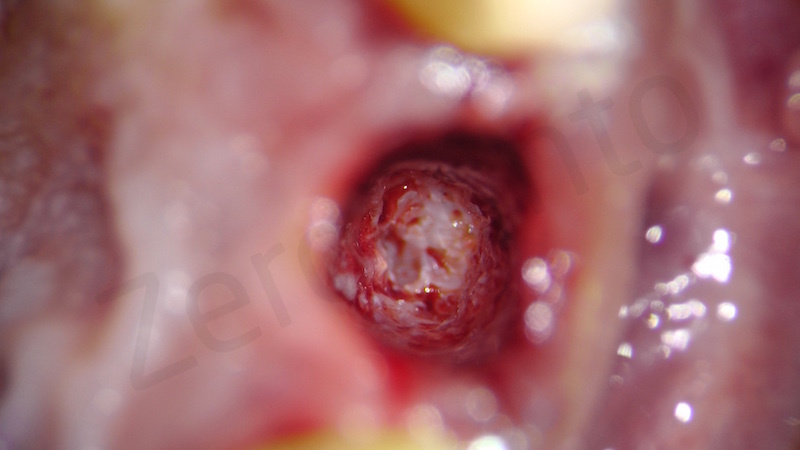
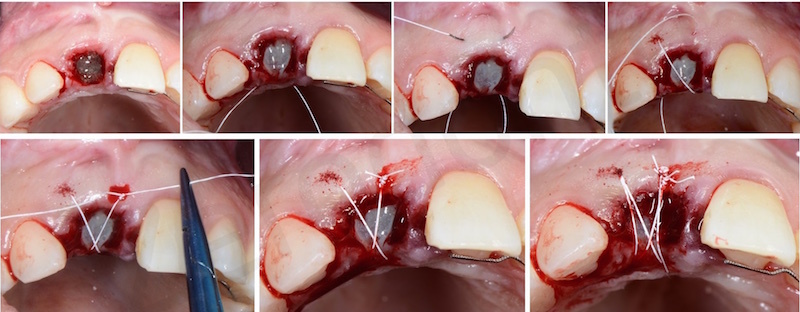
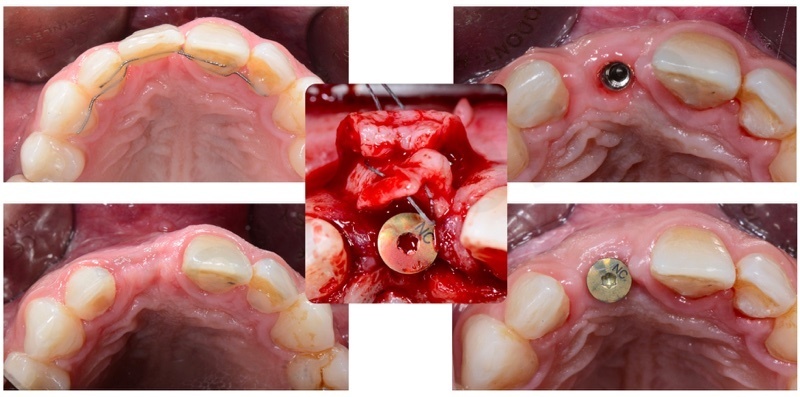
An incision with release cuts was executed, so as not to raise the interdental papillae and avoid any attachment loss on the adjacent teeth.

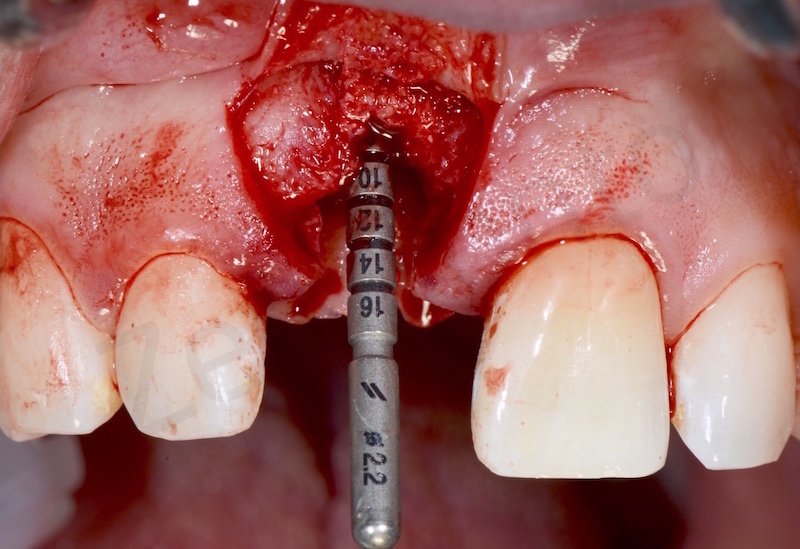
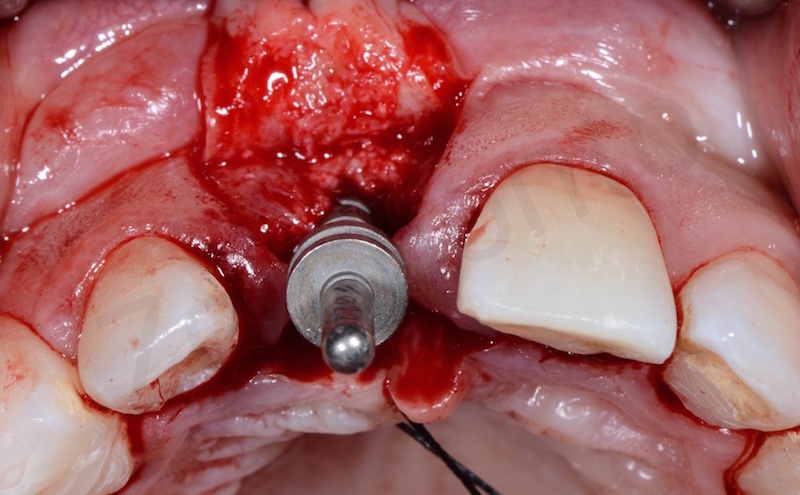
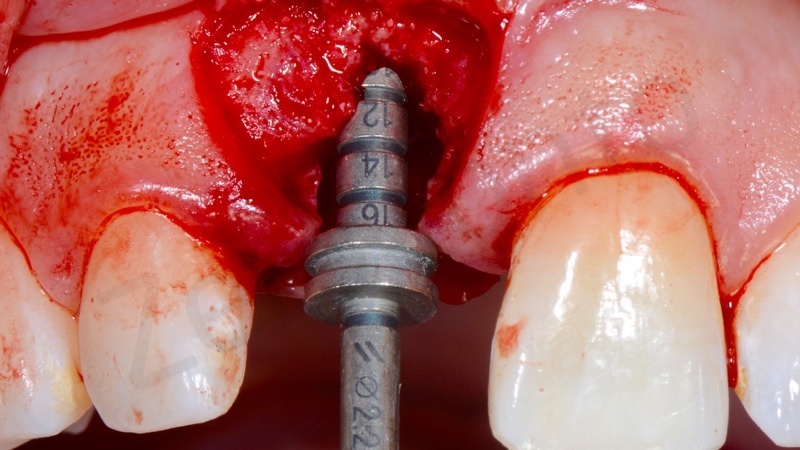
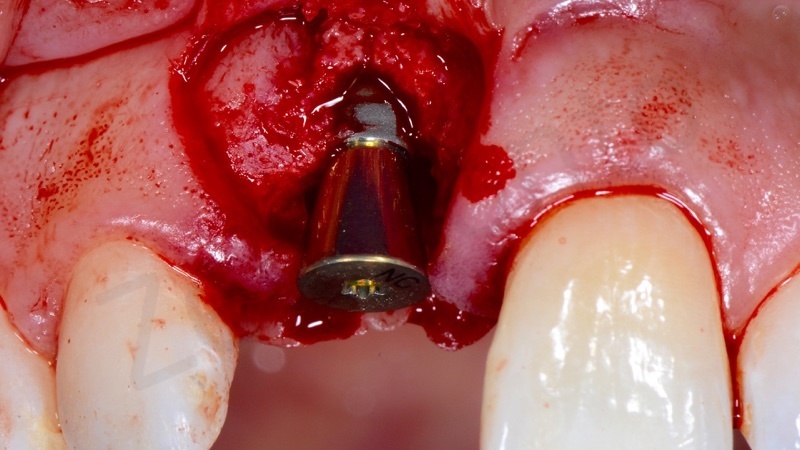
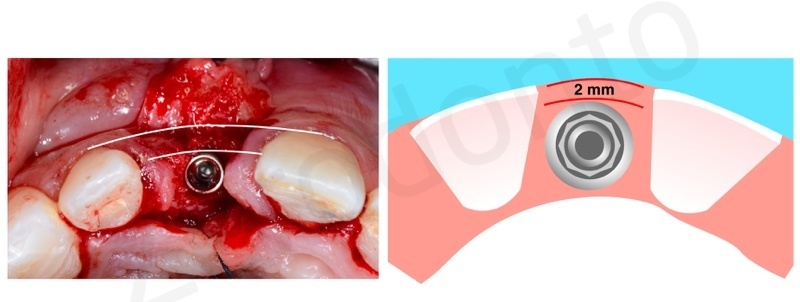
A 3.3 mm Bone Level Straumann implant was used with a transmucosal healing abutment in order to manage a non-submerged healing phase. Nowadays, thanks to very resistant alloys just like the Roxolid (titanium-zirconia), there is no indication to use wider implants in esthetic areas.
It is paramount to place the implant with a prosthetically-guided approach, in order to achieve both functional and esthetic success.
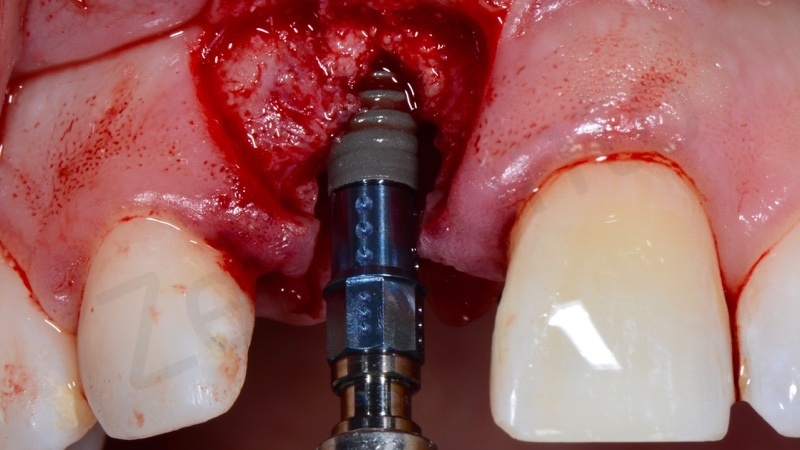

The fixture has to be inserted 2 mm palatally to the buccal tangent passing through the cervical margins of the adjacent teeth, its emergence profile has to be placed at 3 mm from the CEJ of the neighboring teeth and its interproximal surfaces has to be set at 1.5 mm from the adjacent teeth.
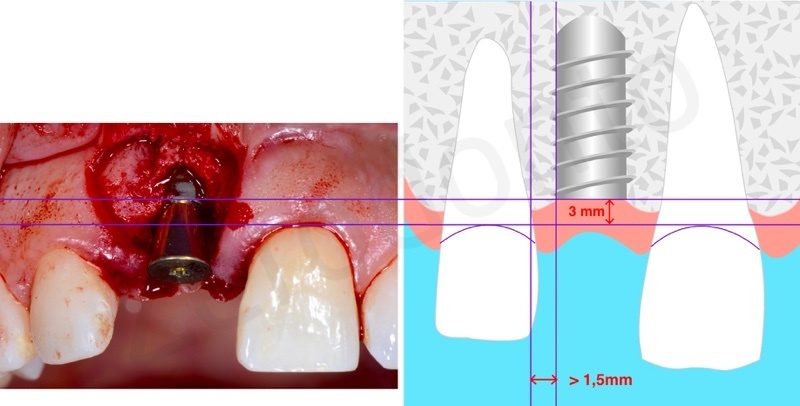
Then, the hard tissues were managed by means of a GBR technique using a collagen membrane and a bone graft made up of a mixture of bovine and autologous bone taken from the implant site itself.
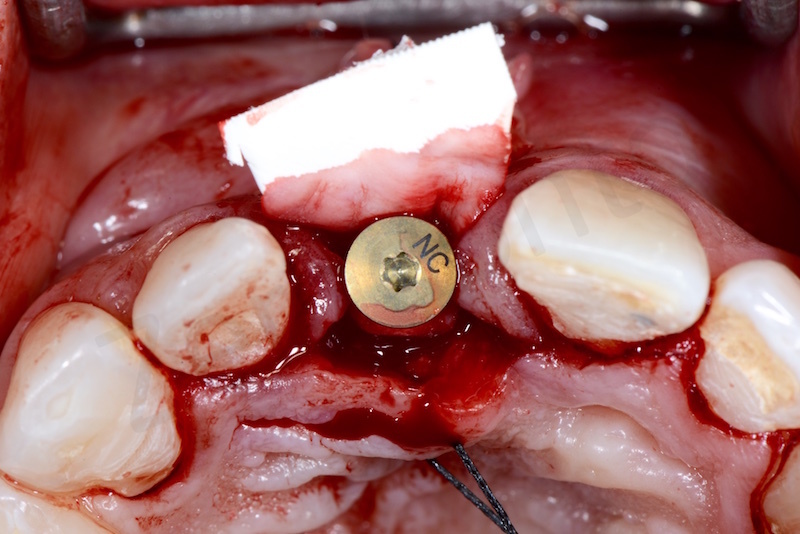
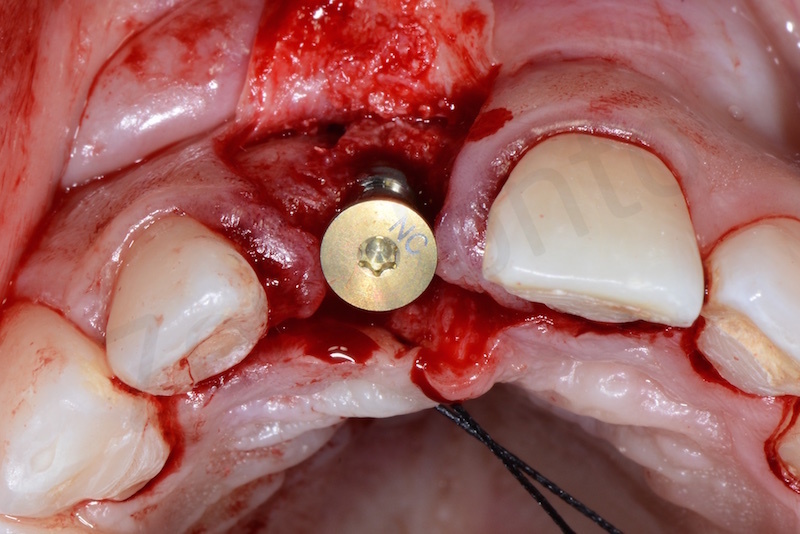

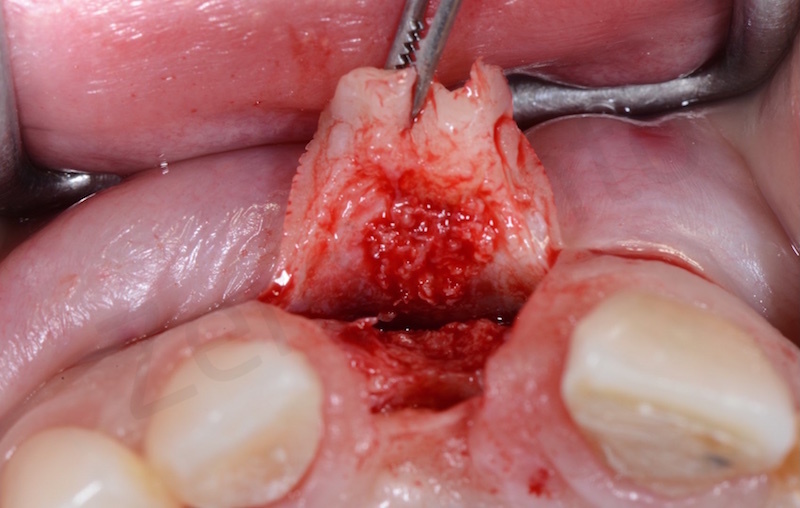
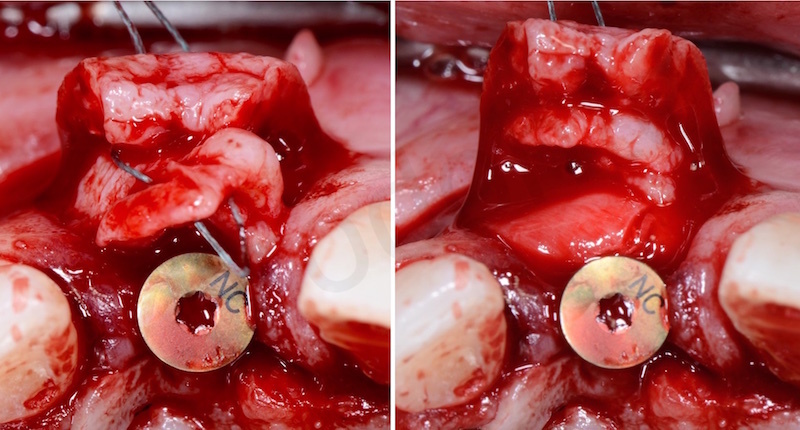
Subsequently, the soft tissues were handled through a connective graft in order to thicken the periimplant soft tissues, allowing the prosthodontist to manage a proper amount of mucosa during the prosthetic steps.
The connective graft was taken from the palatal flap itself and stabilized with a polyester suture.
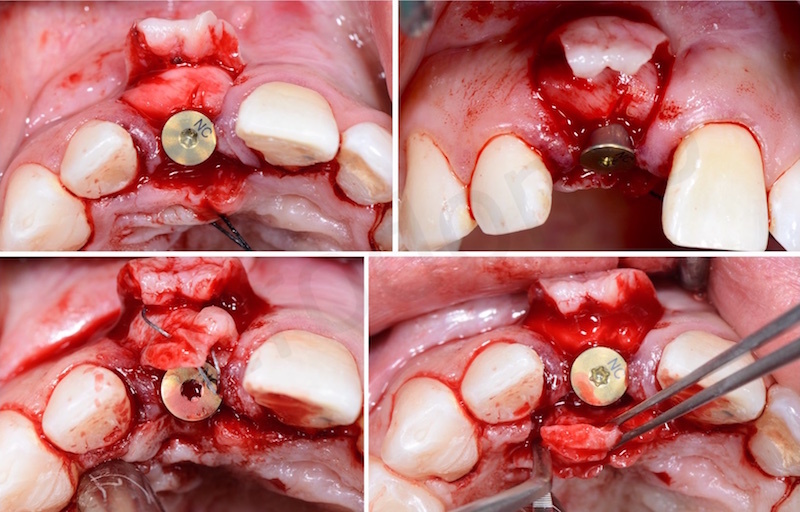
Finally, the flap was closed with Gore-Tex sutures.
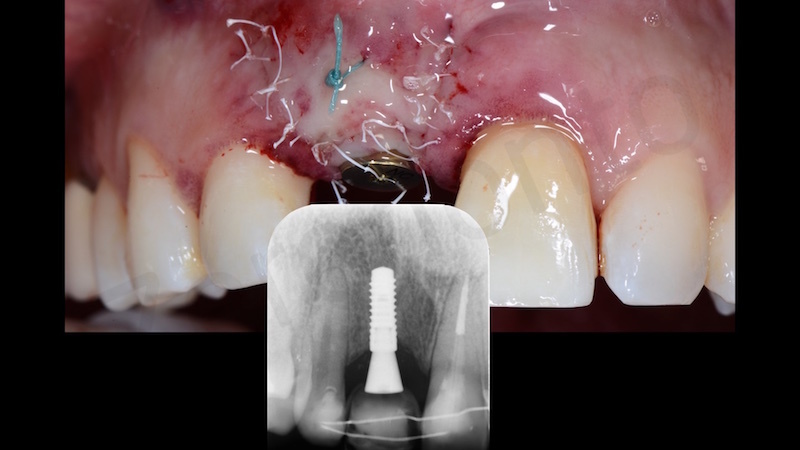
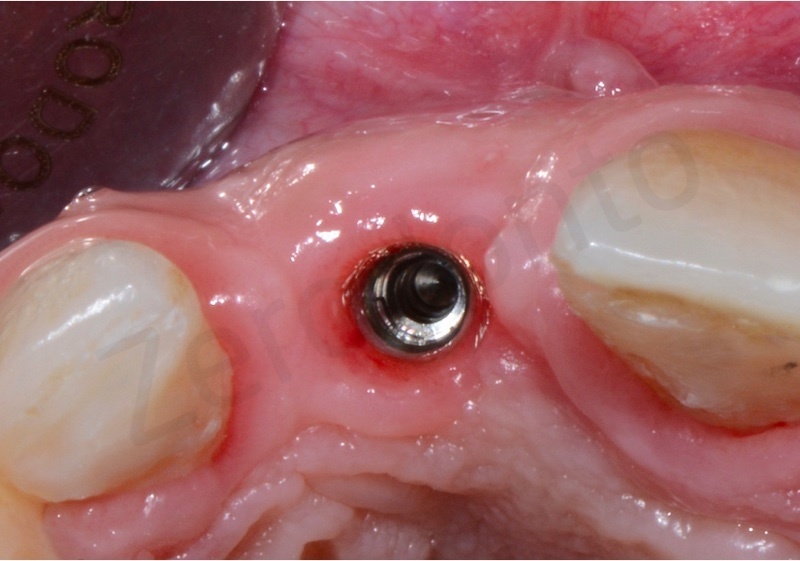
When the sutures were removed, the healing was satisfactory.

Consequently, only through the integration of different clinical factors (i.e. implant positioning, prosthetically-guided hard and soft tissues management) it is possible to allow the prosthodontist to achieve the functional and esthetic success.
In fact, the biotype thickening and the GBR modified the buccal concavity into a convexity permitting to properly shape the periimplant soft tissues during the prosthetic steps.
In the first surgical healing phase, a fixed ortho-pontic temporary restoration was applied by means of an active retainer bonded onto the palatal surfaces of the maxillary front teeth.

PROSTHETIC TREATMENT
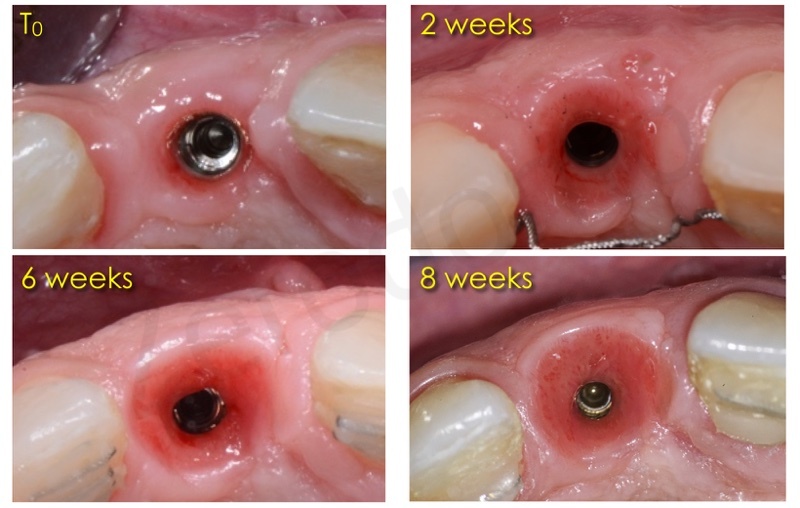
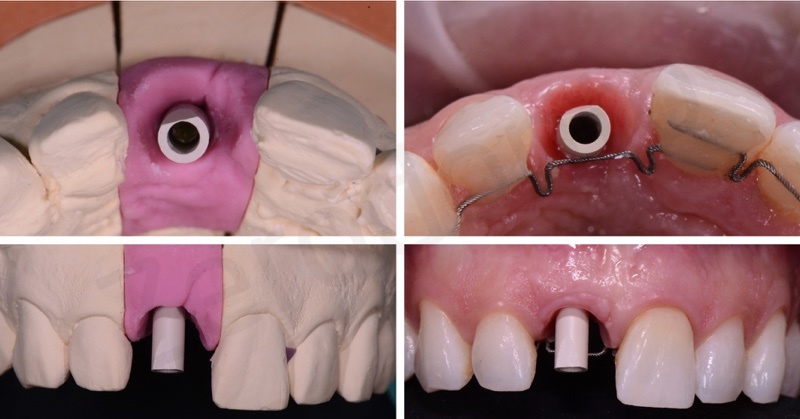
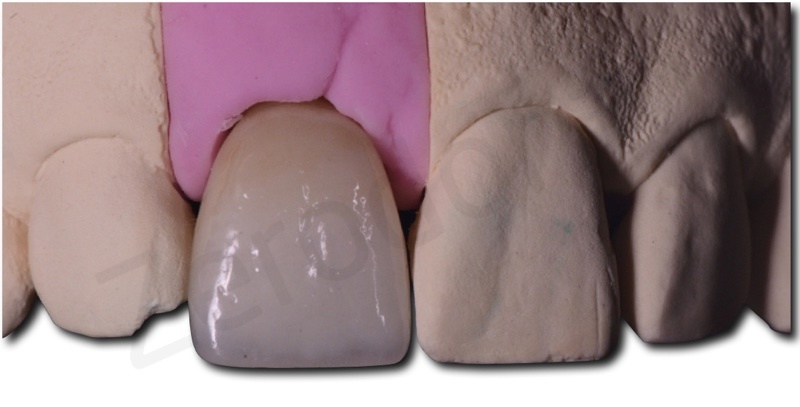
Six months after implant placement, once surgical healing and oseointegration were obtained, a precision impression using a screw-retained transfer coping was kept to fabricate a screwed temporary restoration. A careful esthetic analysis led to the planning of an interim prosthesis symmetrical to the adjacent maxillary central incisor, so as to facilitate the orthodontic finishing during the dynamic compression of the periimplant soft tissues.
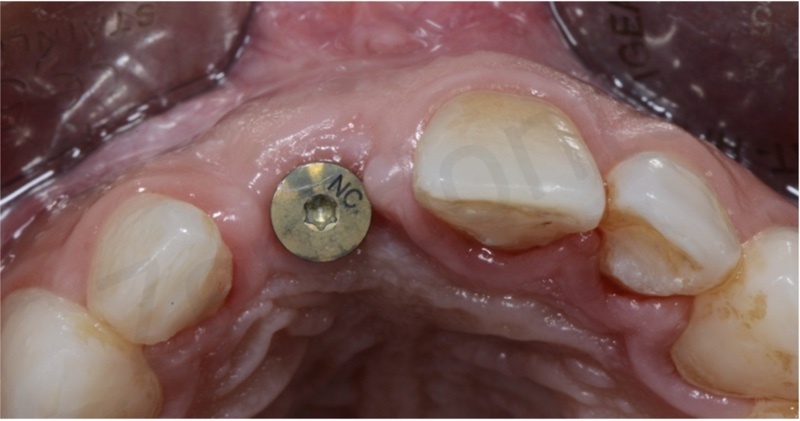


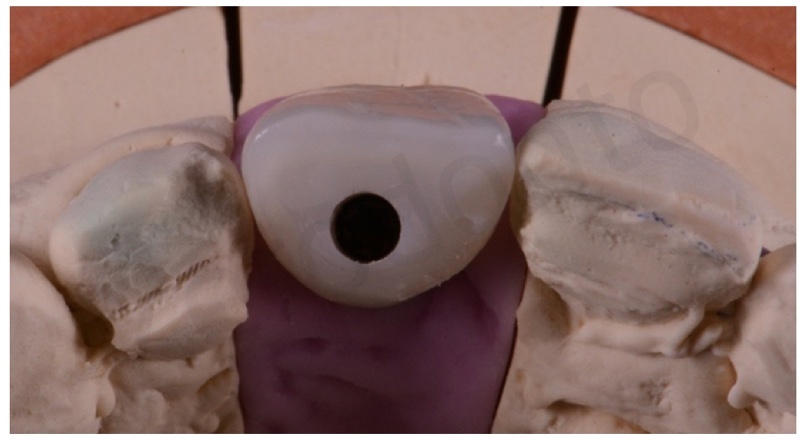
The screw-retained temporary restoration was periodically modified every week using a flowable composite resin, in order optimize the emergence profile. The dynamic compression technique was adopted, first determining a slight mucosal compression, then creating a small concavity on the cervical aspect of the prosthesis (so as to allow a thickening of the marginal tissues) and finally smoothening the emergence profile. After about 3 weeks of conditioning, the profile and volume of the temporary restoration were considered satisfactory to finalize the clinical case.

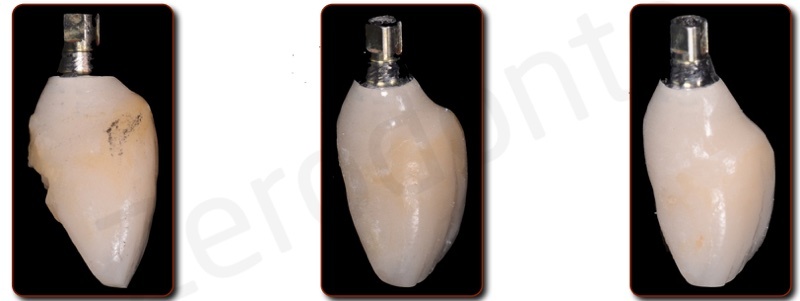

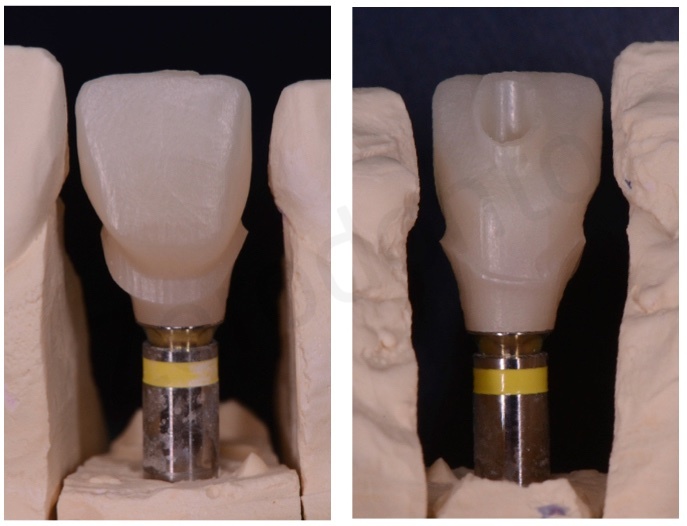
An optical impression was taken using a dedicated scan body. A triple scansion was performed, in order to register the shape of the interim prosthesis intraoraly and extra orally and the position of the scan body. The merging of these scans permitted to store all the obtained information in the CAD software and proceed to the designing of the final prosthesis.




A screw-retained single crown made up of monolithic translucent zirconia layered on the buccal surface with fluorescent esthetic ceramic was produced. The crown was cemented onto an implant abutment for screwing using a dedicated resin cement.

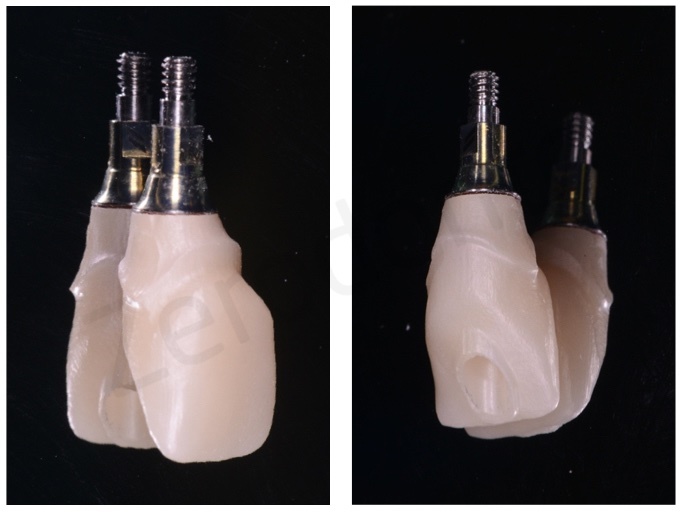
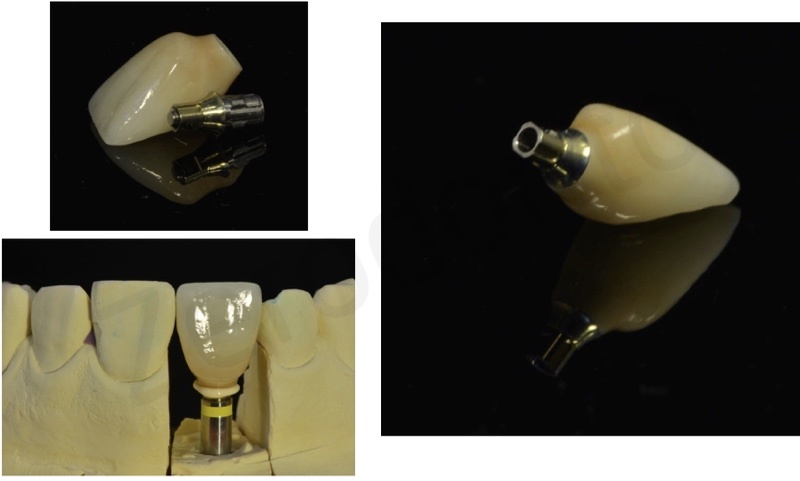
Then, the crown was intraorally seated onto the fixture using a torque controlling device at 32 Ncm. The access hole was covered with PTFE and filled with a composite resin slightly darker than the restoration in order to simplify the identification of the access area for periodical retrievability.
The correct seating of the mechanical components was checked radiographically.
One week after the finalization, the crown was screwed again with the torque controlling device in order to compensate for possible preload loss due to the settling of the prosthetic screw.
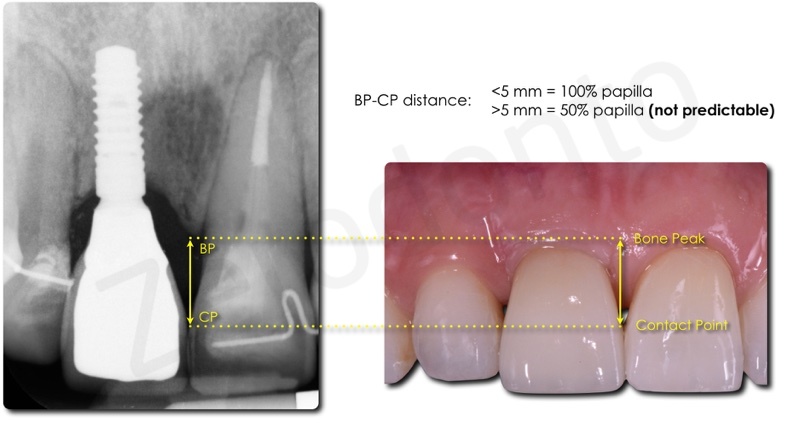
The interproximal contact areas were placed at a distance inferior to 5 mm from the bone peaks so as to favor the filling of the interdental spaces with pseudopapillas.

The crown was designed to guarantee proper oral hygienic maintenance with floss and interproximal brushes.
The good optical properties of translucent zirconia allowed for a natural appearance of the implant crown.

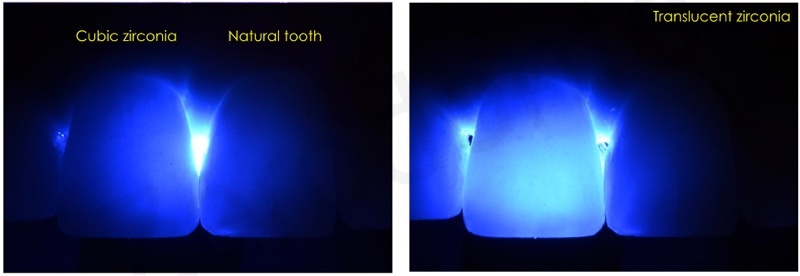
Both the functional and esthetic integration were considered fully satisfactory.




REFERENCES
Camposilvan E, Leone R, Gremillard L, Sorrentino R, Zarone F, Ferrari M, Chevalier J.
Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications.
Dent Mater. 2018 Jun;34(6):879-890. doi: 10.1016/j.dental.2018.03.006. Epub 2018 Mar 26.
Wittneben JG1, Buser D, Belser UC, Brägger U.
Peri-implant soft tissue conditioning with provisional restorations in the esthetic zone: the dynamic compression technique.
Int J Periodontics Restorative Dent. 2013 Jul-Aug;33(4):447-55.
Joda T, Lenherr P, Dedem P, Kovaltschuk I, Bragger U, Zitzmann NU.
Time efficiency, difficulty, and operator’s preference comparing digital and conventional implant impressions: a randomized controlled trial.
Clin Oral Implants Res. 2016 Sep 5. doi: 10.1111/clr.12982.
Tarnow DP, Magner AW, Fletcher P.
The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla.
J Periodontol. 1992 Dec;63(12):995-6.

