Maxillary functional orthopedics (MFO), officially introduced in 1936th in the orthodontic world by Andresen and Haulp as valid alternative in the treatment of malocclusions, has always been subject to profound passion by both followers and opponents.
In the middle of last century the idea of being able to intervene positively or negatively influencing the growth of the jaw was strongly denied in the light of the belief that there was a growth program exclusively determined by genetics and virtually no influenced by the environment and function.
But Moss’s matrix theory, Petrovic’s growth theory, and Woodside’s studies at the University of Ontario in Canada have demonstrated the true consistency of this therapy in a rational, and not just intuitive manner. Mandibular condylar cartilage has a type of growth characterized by different morphology and function compared to epiphyseal cartilage of long bones.
This reality provides an explanation of the type of response of this anatomical structure to the motivation exercised by the functional orthopedic device. At same way, the results of experimental animal studies on glenoid remodeling after functional orthopedic therapy provided further evidence that could provide an explanation for the stability of the corrections, particularly Class II Division 1 malocclusions.
Direct descendant of maxillary functional orthopedics, the Neuro-occlusal rehabilitation (NRO), founded by Prof. Pedro Planas in the 1950s, is part of the medicine that studies the etiology and genesis of functional and morphological alterations of the stomatognathic system.
The procedure proposed by Planas aims to research the causes of these alterations, eliminate them and, if possible, rehabilitate the organ or reduce the severity of the lesions. It is therefore proposed to ensure freedom of movement to the jaw, to provide balance and stability to dental occlusion and the TMJ (Temporomandibular joint).
It differs from the MFO only because it is addressed not only to patients in active growth but to all age category.
Therefore it found hight space application not just in the correction of bone growth vectors, but also in the correction of mandibular-cranial and cranio-cervical relationships on dysfunctional patients, as well as in the treatment of acute and muscular disorders, but also and especially in prosthetic finalization and stabilization over time of the correct mandibular-cranial relationship.
Clinical Case
An 8-year-old girl comes to our observation for a gnathological visit. The anamnesis reports that she was born with caesarean section and was artificially fed. She performs artistic gymnastics and suffered direct trauma on 21 at the age of three, resulting in necrosis of the tooth and displacement of the germ of 21.



Static stomatognatic inspection shows a normally postured upper jaw and no signs of reduction of the transverse diameter of the arch. Notice the lack of 21 (in bone retention) and the slight mesio version of 22, resulting in initial tendency to a class 2 relationship on the 2nd quadrant. The mandibular arch appears well-shaped and free from crowding signs. The medians are slightly decentralized due to a millimeter shift of the upper median to the left.



The incisive head-head shows a margin incisal contact with no posterior balances and the presence of a black hole slightly more evident on the left side.



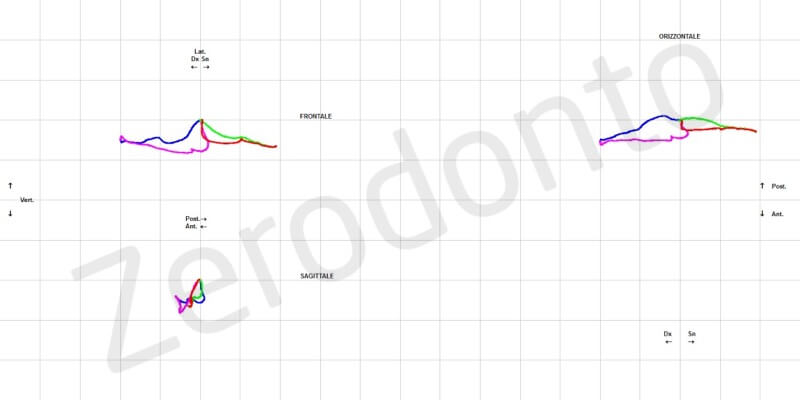
The protrusive appears long enough and is characterized by a slight front overhang. However, there are no deflections in lateralities and posterior balancing contacts, as evidenced by the kinesiographic plot.
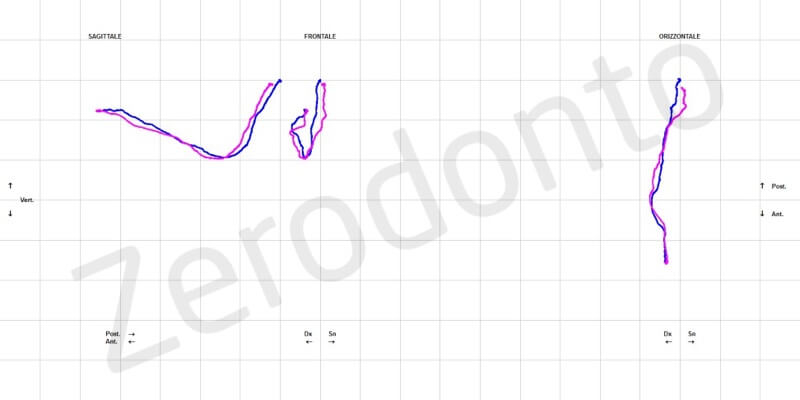






In right lateral movements, there is evidence of a pure canine disclusion contact that occurs in the absence of back balances. In left lateral movements, there is evidence of several dental elements contacts in the presence of posterior balances. The right AFMP, slightly above the controlateral, devotes a tendency to a prevalent left chewing.



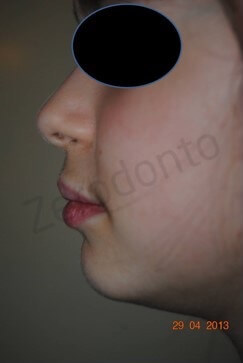
The tongue is free of torsion and signs of ankyloglossia. It’s not festooned but rather narrow and long. The interincisors frenums do not coincide due to a slight left upper mandibular laterodeviation associated with the lack of 21 in the arch. The soft tissues analysis of the profile show an accentuated mentolabial fold and signs of slight bi-protrusion, while the upper lip is not short and lips are competent.

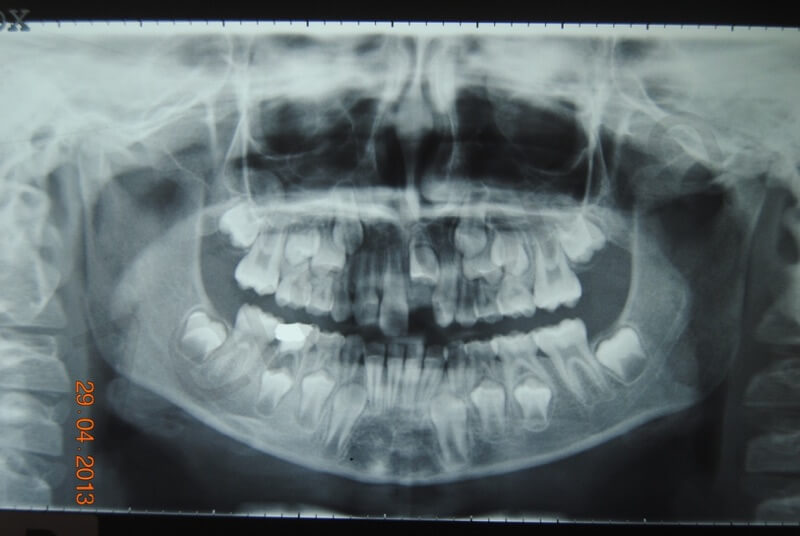
In the OPT note the inclusion and the buccal version of 21, as a result of the traumatic event at age 3.
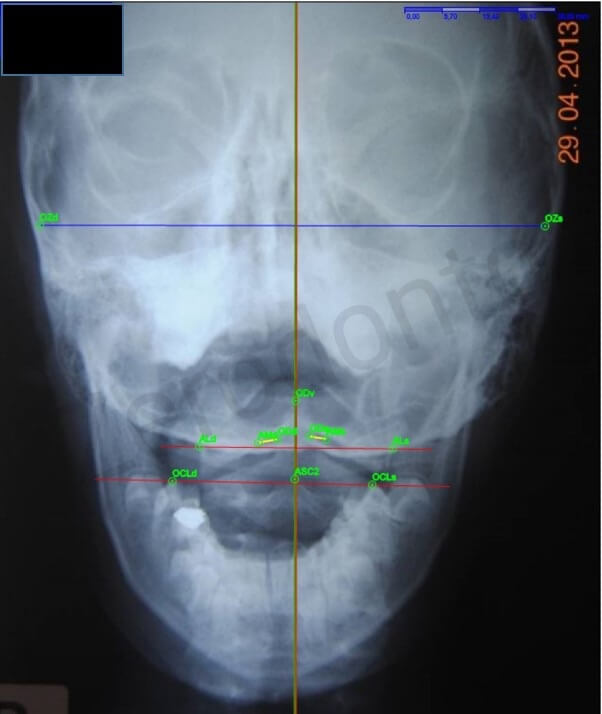
C1 and C2 do not show any particular signs of rotation, despite the incipient tendency to left chewing.

Intervertebral spaces between C0-C1-C2 are symmetrical. Also note the slight reduction of C2-C3 apophyseal joint space, resulting in cervical articular fulcrum and possible tendency to swallowing dysfunction.
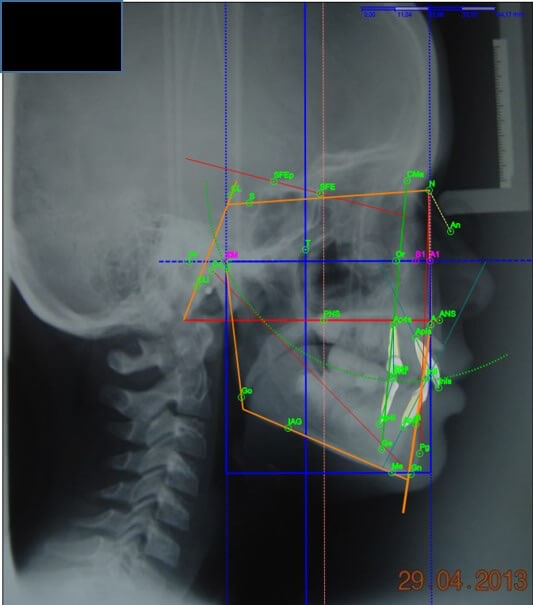

Bimler’s cephalometric analysis shows a growth trend in mesodivergent class 1.
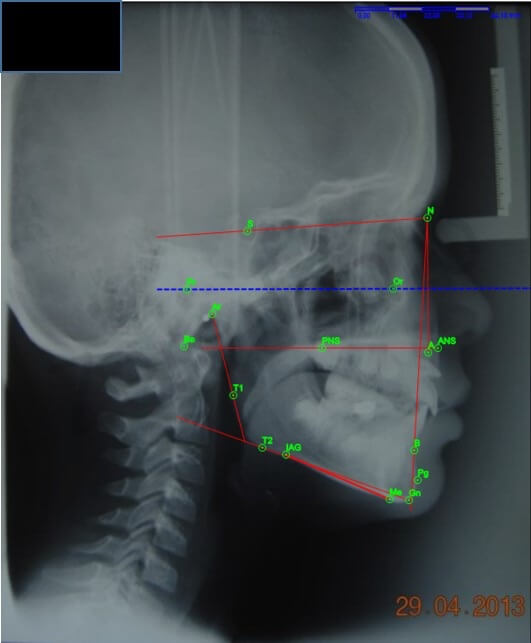
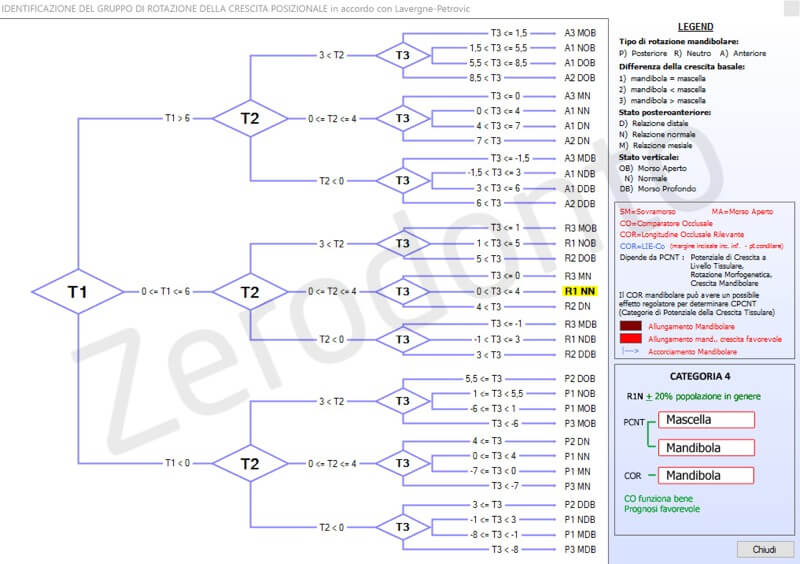
Lavergne-Petrovic’s cephalometric analysis identifies his membership in a category 4 rotational growth group, belonging to the R1NN type, typical of a Class 1 with a mandibular neutral type rotation, and with a standard postero-anterior and vertical relationship.
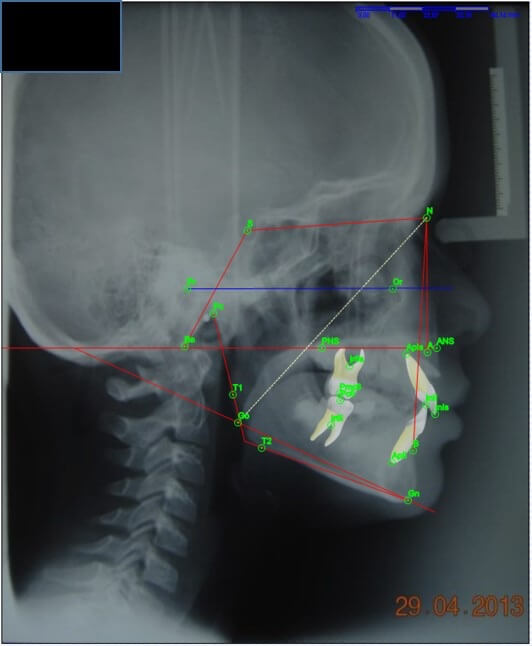
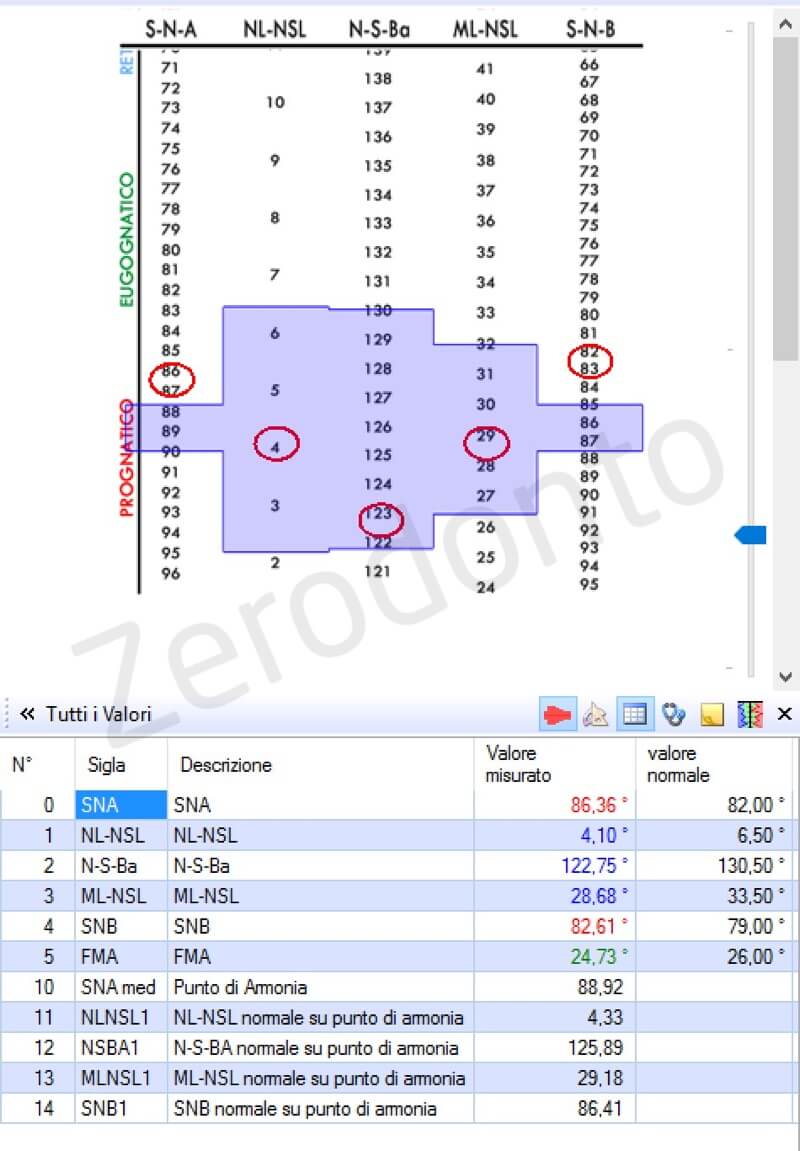
The analysis of the “floating norm” according to Tollaro – Baccetti confirms growth with a sagittal relationship of 1 ° class with a normally rotated bispinal plane.

Finally, kinesiographic analysis shows that pathological angle and deviation on the frontal plane of the habitual centric and swallowing do not fully confirm the characteristics of the dental traces, with wide extremes, with slight slicing of lateral joints and long enough protrusive, characterized by a modest overhang and a good climb. Trace divergences present on both large opening and lateral paths confirm that the framework could be justified by a largely postural causal component, to which the occlusion is adapting. It is therefore necessary to intervene on occlusion while the prognosis appears to be quite favorable, although osteopathic collaboration (especially in the cervical-scapular area) is not excluded if no substantial improvement in the cranio-cervical relationship can be found with the resolution of malocclusion.
The treatment goal of this patient should therefore be to slightly expand the upper jaw, opening the 21 eruption corridor and allowing the disimpaction, and re-balancing chewing so that it can make it perfectly alternate bilateral and reduce the risk of future relapses. Therefore a orthopedic-functional treatment plan with a PIPS (Planas indirect Simple tracks) class 1 ^ and a possible repositioning orthodontic treatment of 21 in the arcade is expected.

We choose to apply Class 1 Planas indirect simple tracks, with the aim of obtaining an initial maturation of the occlusal plane and make the perimeters of the arches compatible to accommodate permanent dentition by stimulating the expansion of the bone bases, in absence of significative mandibular bone growth boost in the sagittal direction, since the cephalometric characteristics of the growth trend are in class 1. The final aim is to correct bone bases and stimulate muscle-articular exercise to allow self-regulation of the system. The vertical anchorage of the device transfers the forces of the jaw muscles to horizontal forces for the frontal springs with mesio-distal action of the teeth 12 and 21. The modified vestibular arch supports the lip and releases the 12 eruption curve.

The intermittent stimulation action exercised on the maxillary basal bone any time the swelling acts occurs, due to the vertical anchor, produces an increase in the turnover in the included tooth area and its subsequent partial eruption under the mucous membrane. This because of the neurovegetative activation effect of the Basic Adjustment System, that produces a stimulation of the microcirculation and all bone metabolism and the expansion of the basal bones.

The next application of a spring capable of exerting a “presence effect” on the vestibular surface of the same progressively and slowly guide the eruption of 21 with a correct arch orientation.




The eruption occurred in the alveolar mucosa, and the lack of adherent gum is evident, but this last progressively and inexorably has grown over time because the tooth movement occurred as a result of a physiological (if guided) process of eruption, and not for a surgically induced disimpaction.
The contact that occurs at each swallowing between the acrylic slopes located on the upper and lower plaques creates an “intermittent” growth stimulus effect on the entire basal bone of the jaws, well different from the traditional orthodontic, since it does not being continued over time, does not cause hyaline degeneration of the alveolar bone with subsequent bone remodeling. There is not resorption at the periodontal compression zones, nor new bone apposition in traction areas. The “intermittent” stimulus acts rather with a “proprioceptive” afferent effect capable of modulating the neurovegetative control of the arterial tone and venular at the level of the Basic Adjustment System, thus allowing a greater inflow of metabolites and oxygen into the bone baseline, also facilitating the drainage of catabolites at the venular level. Metabolic and gaseous exchanges between the circulatory system and the tissues will be more efficient. Since these are best sprayed and fed, they will have a greater “growth stimulus”, induced by the optimization of intermediate metabolism at the local site. For this reason, a “physiological” eruption of the teeth can be seen, resulting in the regeneration of the adherent gum.



From the last photos we can highlight the correct positioning of the dental element to complete the clinical case. Occlusal planes, which are not yet, completely matured, will allow optimal intercuspidation between the antagonistic arches, following completion of the dental eruption, guided by a proper function.
Conclusions
The use of maxillary orthopedics principles, working with mild and intermittent forces, not only modifies the growth of bone bases, but also, where necessary, the realization of dental movements during eruption and maturation of the roots . This is enough in many cases to achieve an easy conquest of the necessary spaces, preserving periodontal health and alveolar remodeling.
Bibliography
- SIMOES, W.A. – Ortopedia Funcional dos Maxilares. San Paulo, Artes Mèdicas, 2003
- VINOD, K.; DAVIDOCH, Z – Cellular, molecular, and tissue-level reaction to orthodontic forces. Am. J. Orthd. And Dentofacial Orthop. 129:461-469, 2006
- LINDEN, FRANS P.G.M. van der Desenvolvimento da denticao. Ed. Santos, 1986
- PLANAS, P. – Riabilitazione Neuro-Occlusale RNO. L. Rubini – Muzzolini

