COMPLETE MAXILLARY AND MANDIBULAR EDENTULISM TREATED WITH IMMEDIATELY-LOADED DENTAL IMPLANTS AND SCREWED FULL-ARCH TEMPORARY PROSTHESES
INITIAL SITUATION
The patient referred a clinical history of severe adult chronic periodontitis.
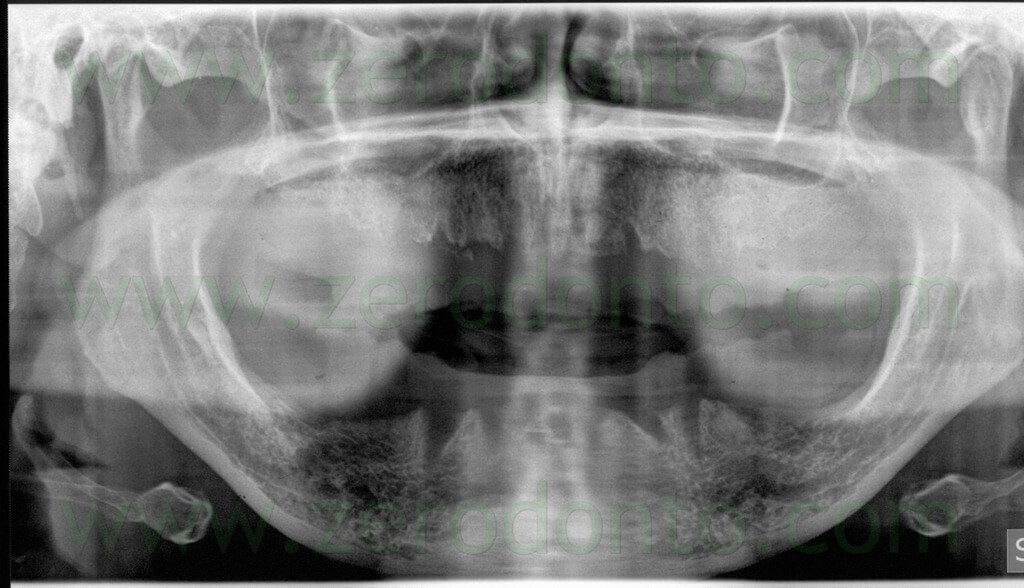
She has been edentulous at the maxillary arch for about 3 years while the latest extractions at the mandibular arch had been made about 6 months before the clinical examination. The patient presented with good general health and oral hygiene. She wore two removable complete dentures unsatisfactory for both function and esthetics.



After explaining the different prosthetic solutions and the possible complications, the patient specifically required a fixed implant prosthesis and signed a consent form. It was planned to perform an implant guided-surgery intervention with immediately loaded temporary prosthesis in each arch.
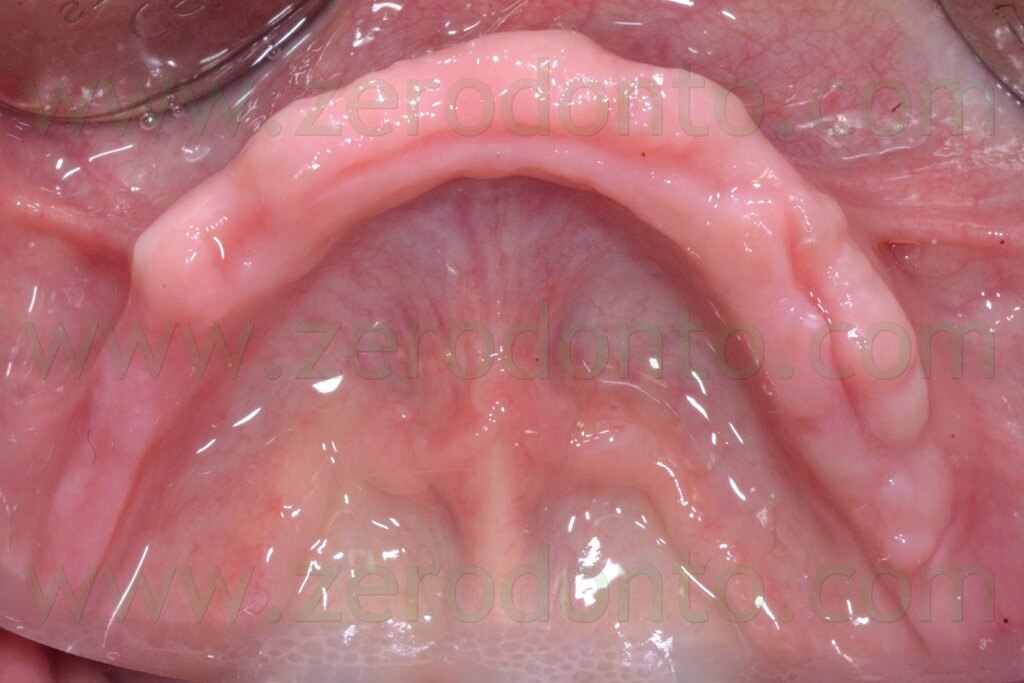
From a skeletal viewpoint, the patient presented with an edge-to-edge relationship with tendency to III Class. The edentulous ridges were interested by moderate atrophy but with the distal mandibular areas where such atrophy was severe. Furthermore, a severe lack of adherent mucosa was evidenced in quadrant 4.



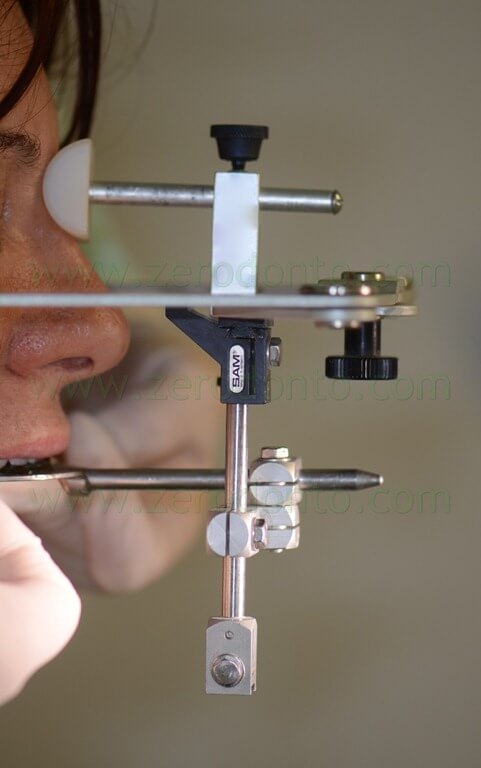
A facebow was used to transfer the intermaxillary registrations in an articulator and study the case.
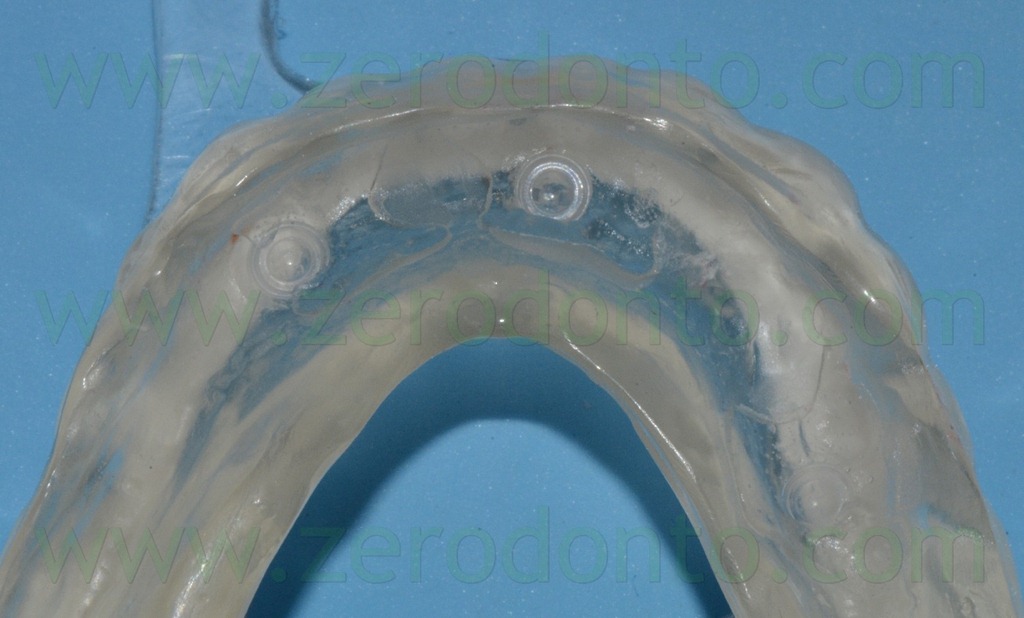
Two new complete dentures were made, according to Passamonti’s technique. Because of the severe bone atrophy, three Straumann temporary mini-implants with ball-attachments were inserted in the mandibular arch to stabilize the denture. Three plastic matrixes for ball-attachments were blocked in the removable prosthesis by means of direct relining.
The matrixes were placed over the relative attachments intraorally and three holes were drilled in the denture matching the positions of the mini-implants. Such holes were filled with self-polymerizing relining resin and the patient kept the denture in occlusion until the resin completely set. Finally, the relined denture was finished and polished, transforming it from a removable complete denture to a temporary overdenture.
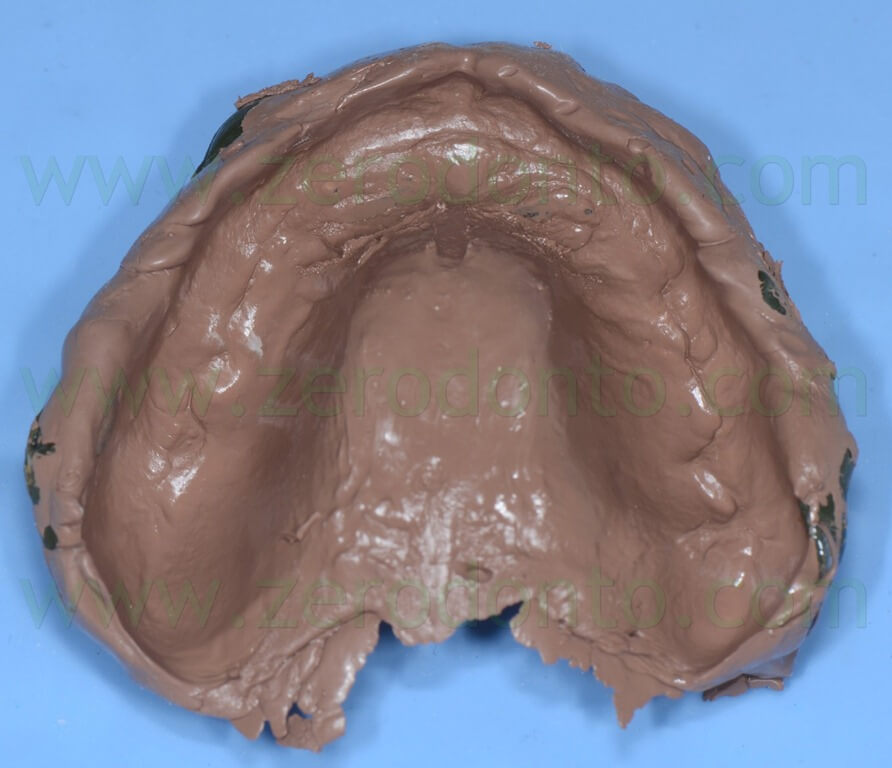
After two weeks of mucosal tissue conditioning, a polysulfide impression of each arch was made, in order to fabricate the master casts.




A careful facial esthetic analysis was made as well as the conventional functional, phonetical and esthetic try-in procedures, using denture teeth mounted in wax on transparent acrylic registration bases, so as to highlight any compression area of the edentulous ridges.






The left maxillary emiarch resulted to be too coronal because of a moderate asimmetry of the lower lip. Consequently, the length of the incisal margins of 22 and 23 was reduced, highlighting the areas to be shortened intraorally by means of a marker pen. The stability of the registration bases was improved using a denture adhesive paste. The rest and smile positions were evaluated both in the frontal view and on the sides. Once the desired esthetic result was achieved, the phonetic tests were repeated and two new polysulfide impressions were made to mount the registration bases in the articulator more precisely.







Further esthetic try-in procedures were made until the patient’s requests were accomplished. Then, two impressions were made using a zinc oxide-eugenol paste. A new maxillary denture was fabricated and its occlusal scheme was studied to properly match the occlusion of the mandibular temporary fixed prosthesis.





The maxillary denture and the final mandibular registration base were used as individual impression trays to make two medium-consistency polyether impressions, in order to verify the correct position of the master casts before fabricating the radiological templates. Moreover, an occlusal wax was made to transfer the centric occlusion position. Careful attention was dedicated to the occlusal analysis, in order to optimize the occlusion of the implant-supported temporary fixed prostheses.



FABRICATION OF THE RADIOLOGICAL TEMPLATES AND CONE-BEAM COMPUTED TOMOGRAPHY SCANNING
The prostheses were duplicated with transparent acrylic resin and barium-painted teeth were used to fabricate a radiological index per arch, in order to perform Cone-Beam Computed Tomography (CT) scannings and prosthetically-guided virtual implant surgery.









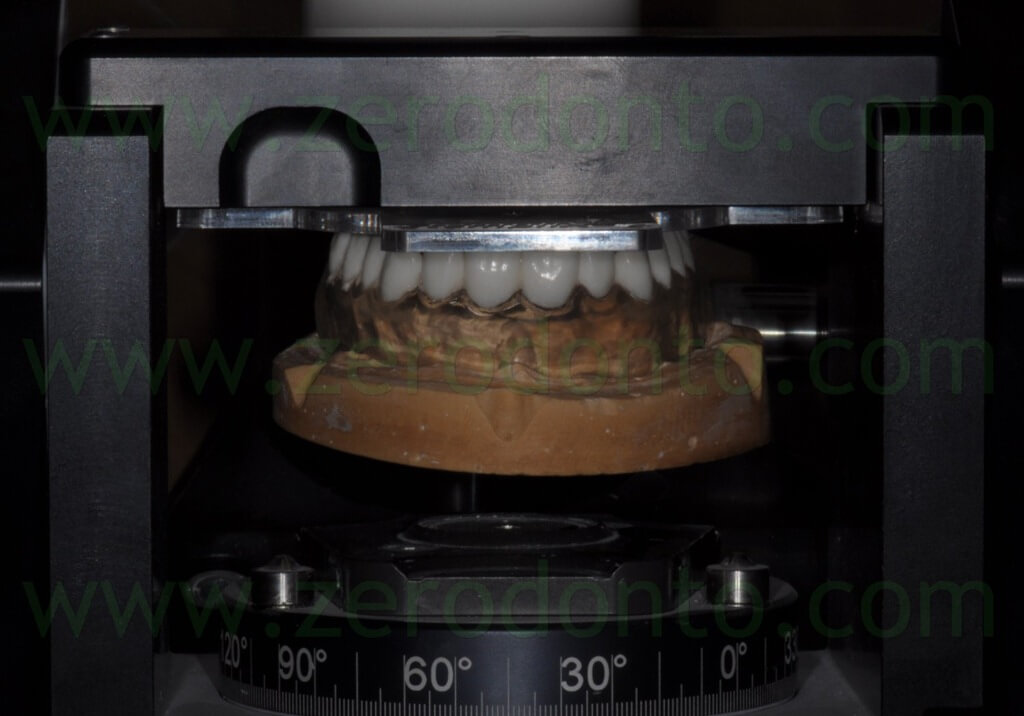
The radiological indexes were blocked on a specific template (Templix) using a transparent acrylic resin on the incisal margins of the barium-painted teeth. Then, the master casts assembled on the Templix were mounted in a device (Gonyx) dedicated to implant guided-surgery, in order to position 3 radiological metal reference points on the basis of specific coordinates due to the morphology of each dental arch.
Each Templix was shaped and refined so as to limit its intraoral room.





The mandibular radiological index was stabilized on the temporary mini-implants by means of the ball attachments. Two occlusal silicon indexes were fabricated to make each radiological template stable in occlusion with the relative opponent prosthesis.



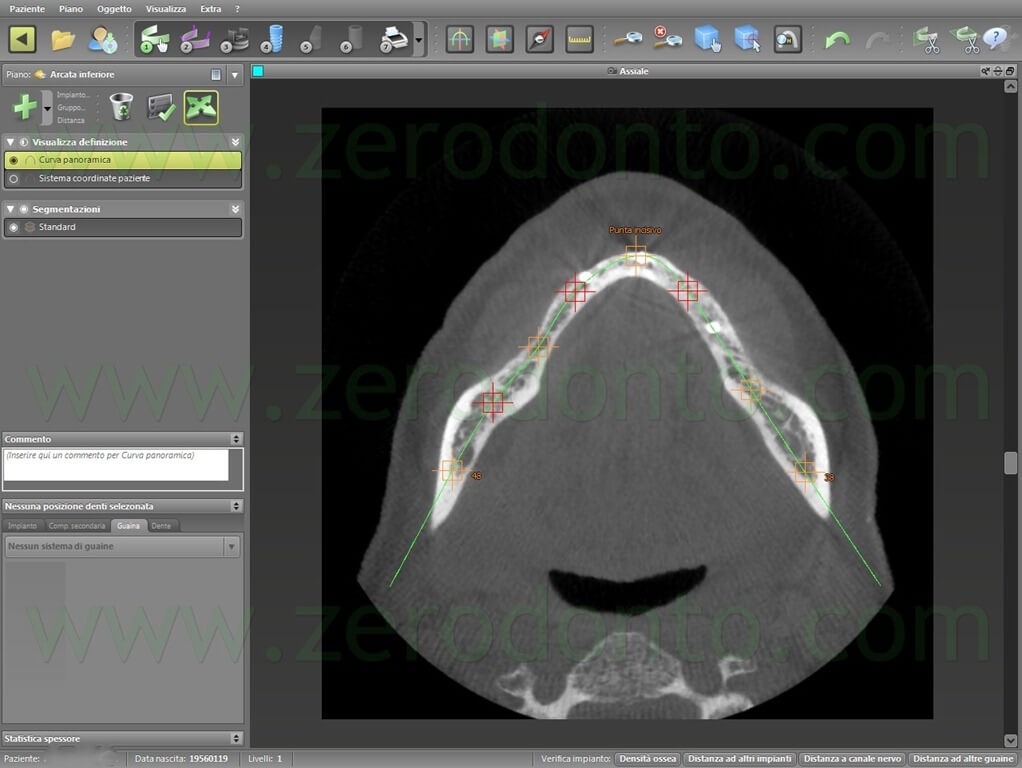
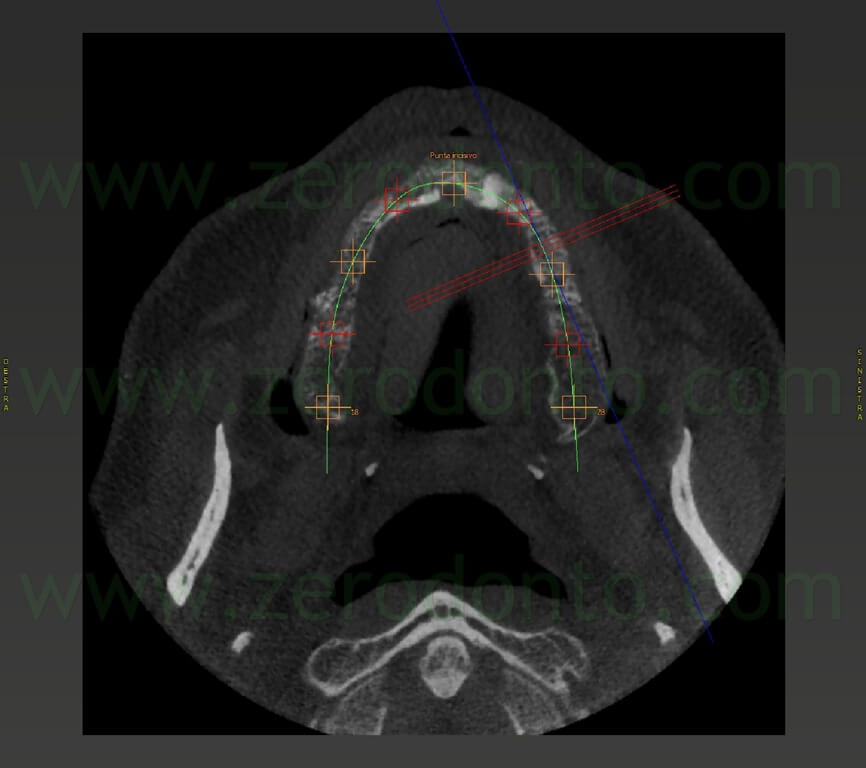
Both dental arches were subjected to low dose Cone-Beam CT scanning. Although there was enough intraoral room to set both the radiological indexes at the same time, due to the limited dimensions of the radiological sensor, it was decided to make two different scannings in order to achieve optimal scanning resolution and width.
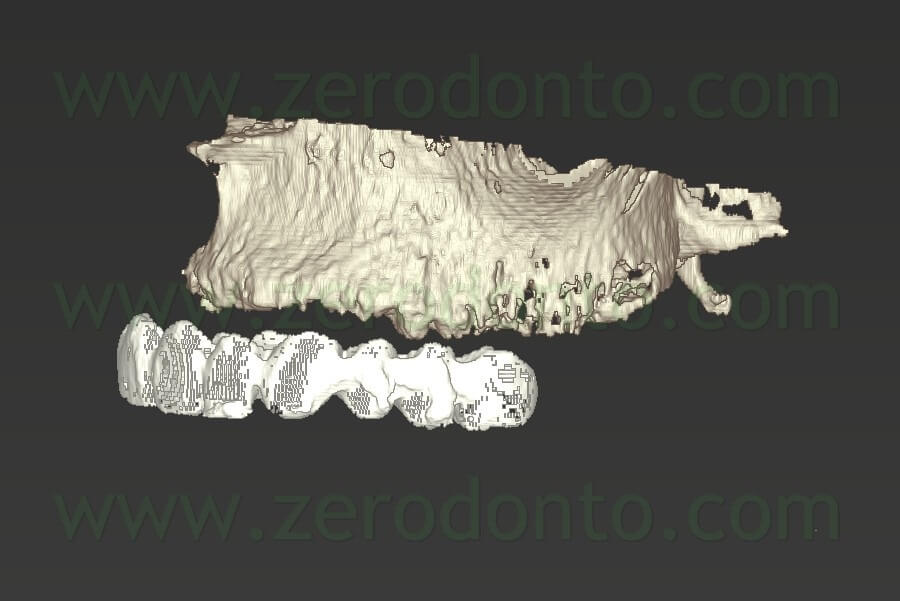
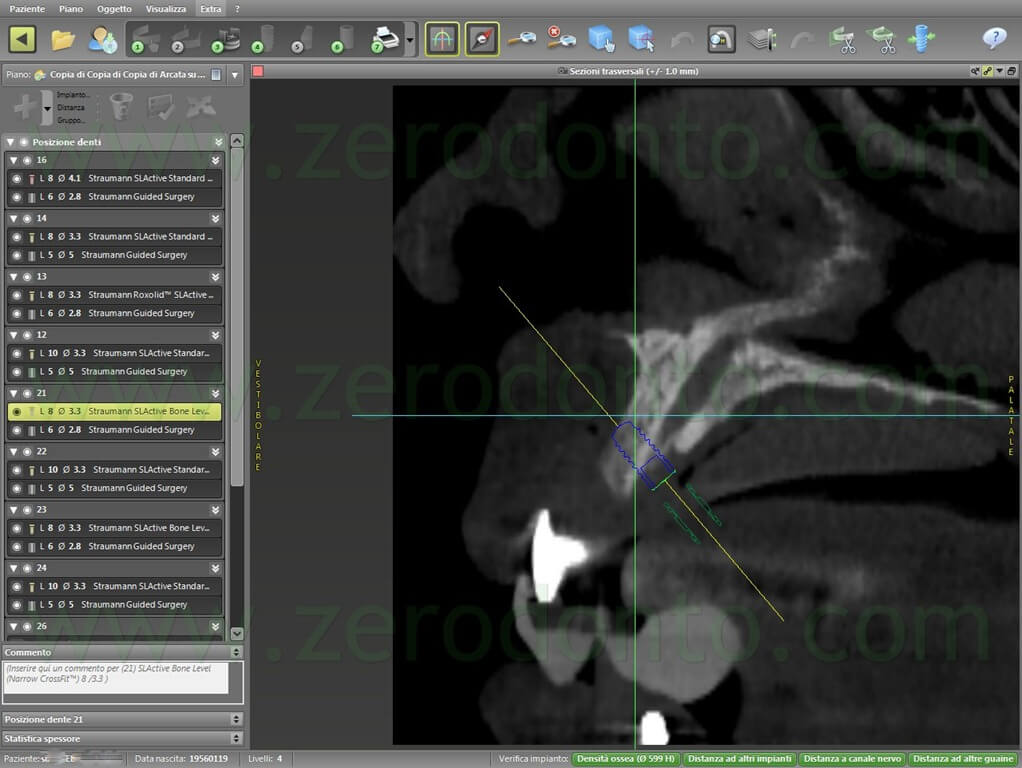
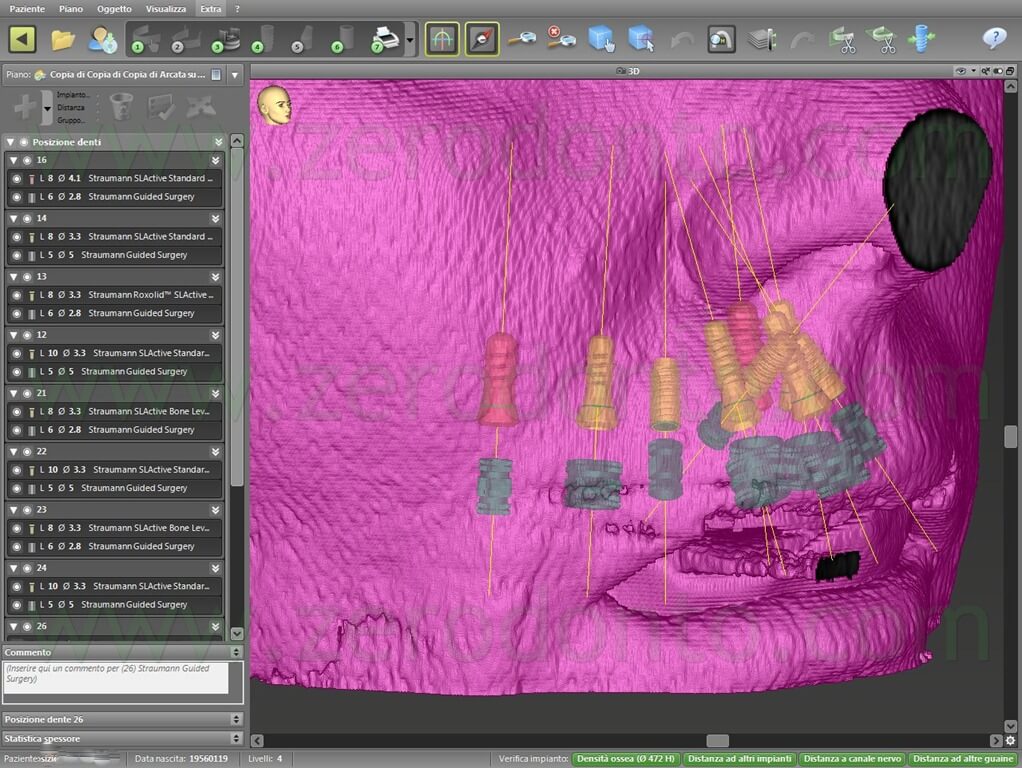
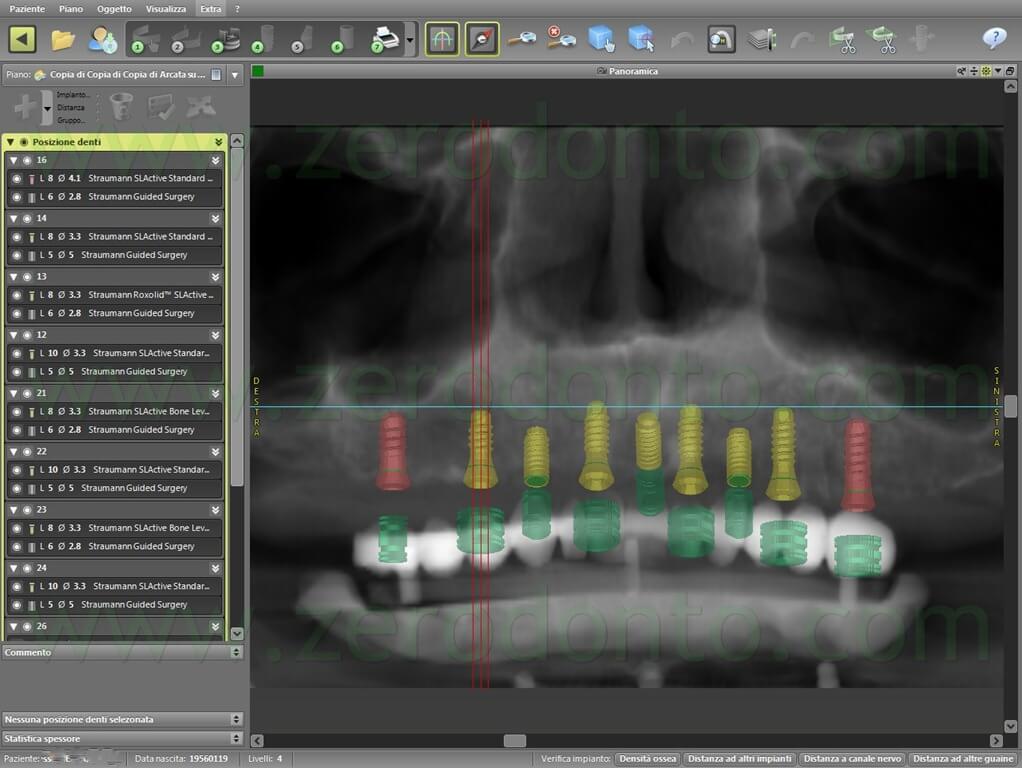
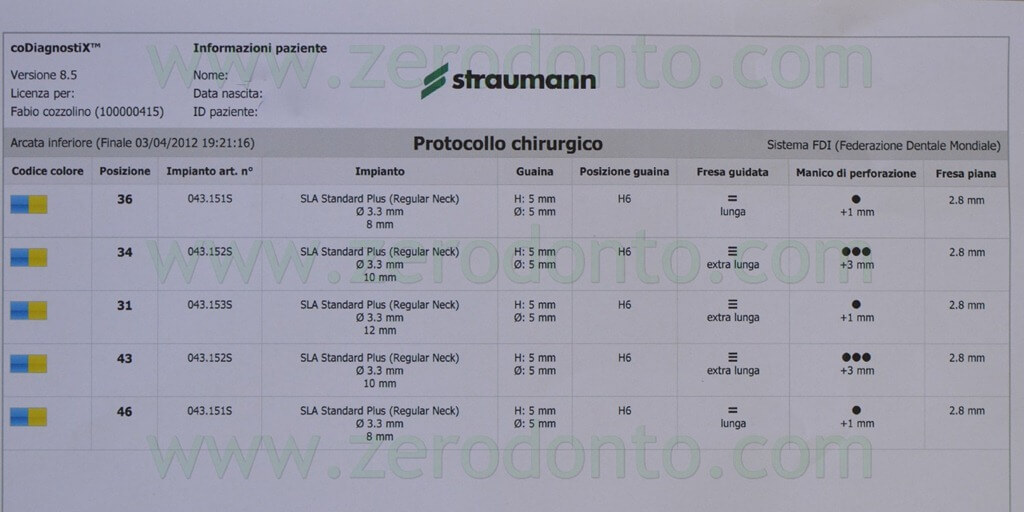
GUIDED-SURGERY PLANNING USING CODIAGNOSTIX SOFTWARE
The radiological scannings were uploaded in the Codiagnostix software for guided-surgery planning. The software allows clinicians to visualize not only bone tissues but also extraoral soft tissues.
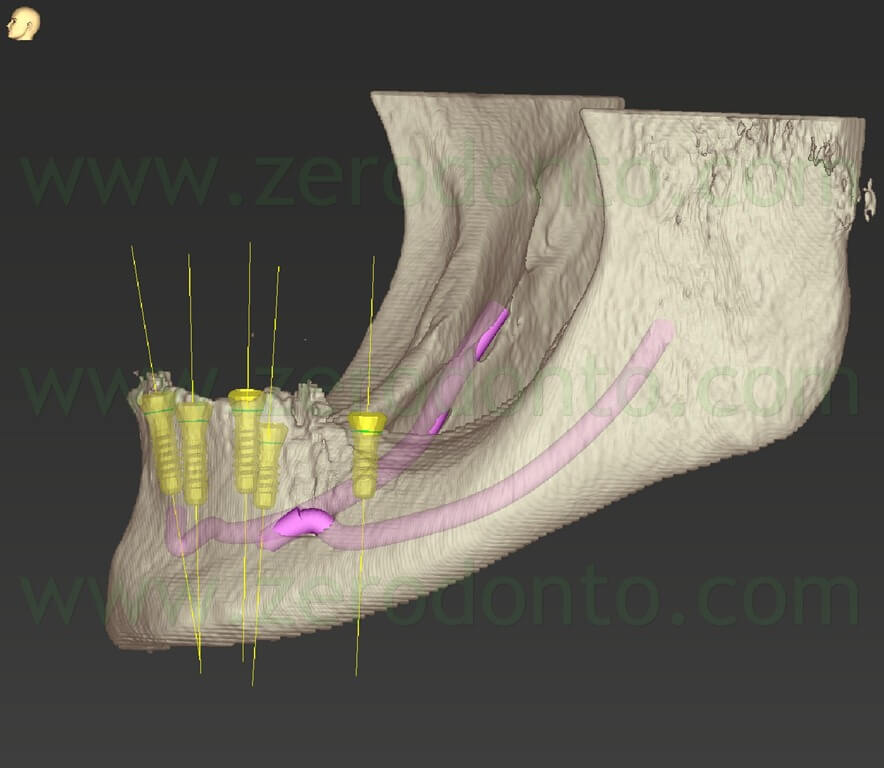
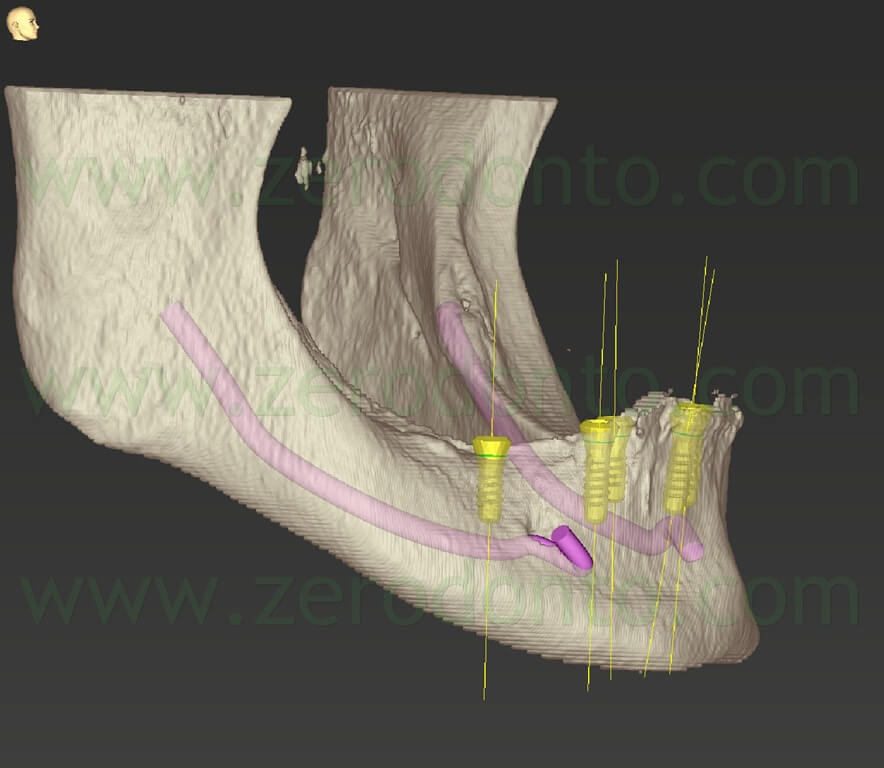
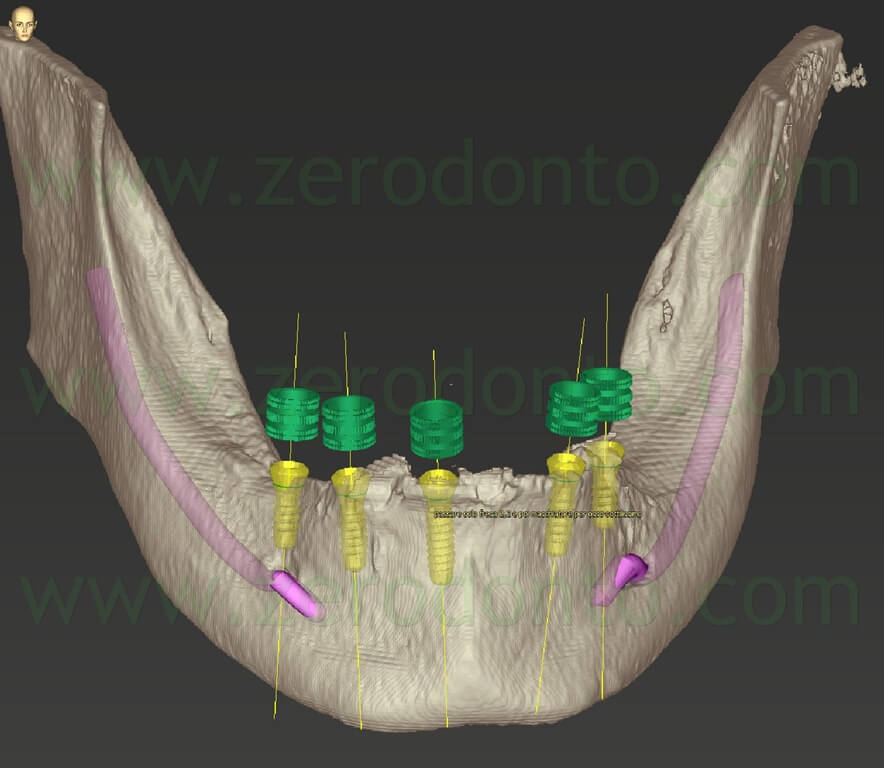
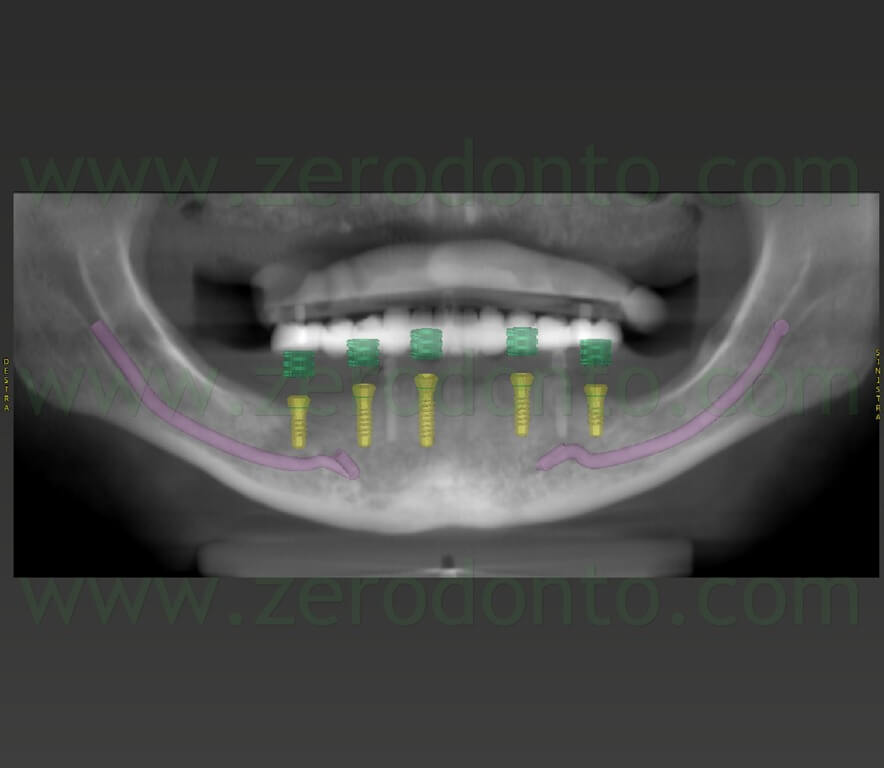
First, the mandibular surgery was planned. The anatomical structures not to be damaged (such as the mandibular nerves) were highlighted. Then, the arch line was evidenced and each slice of the scanning was carefully evaluated.
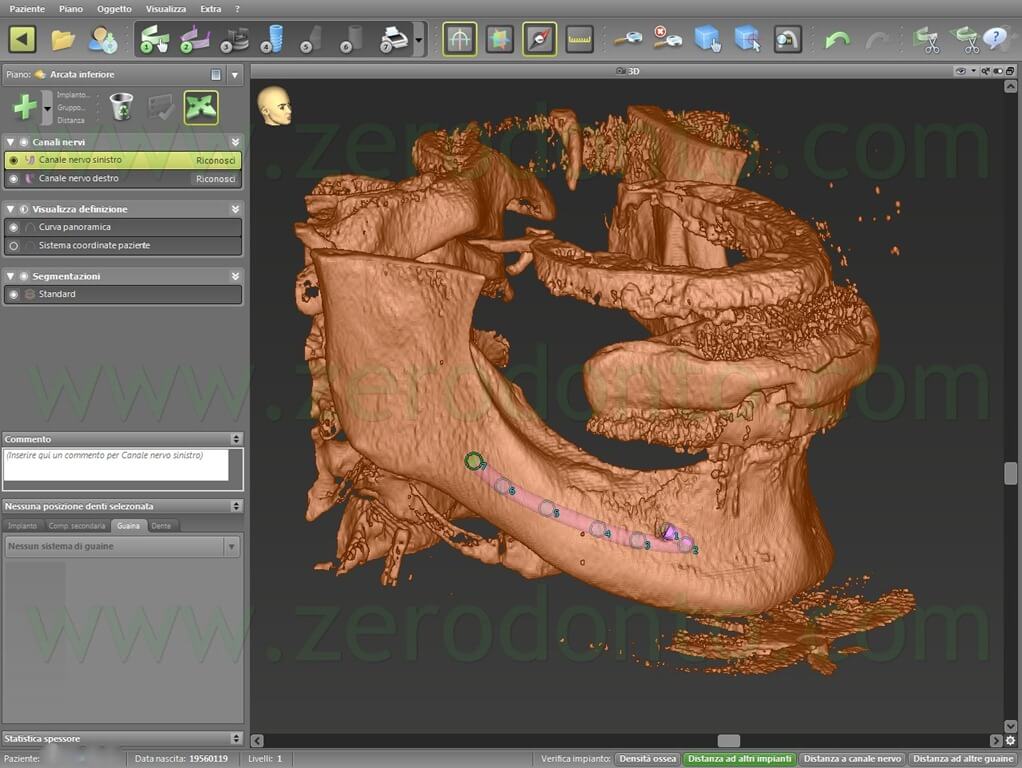

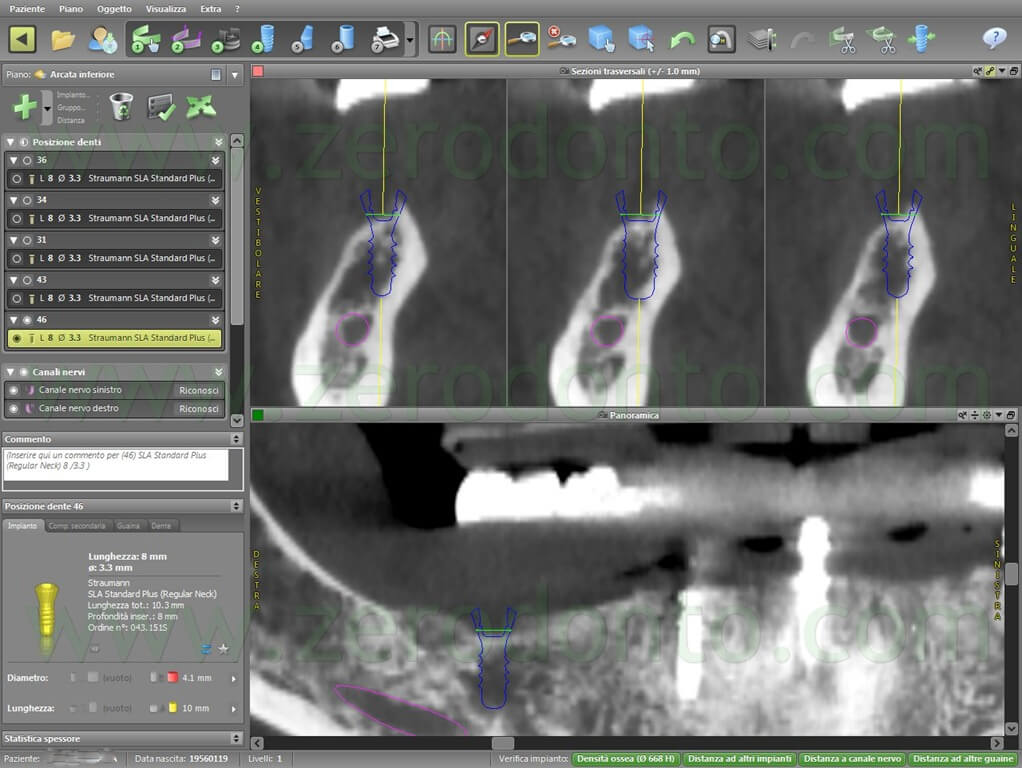
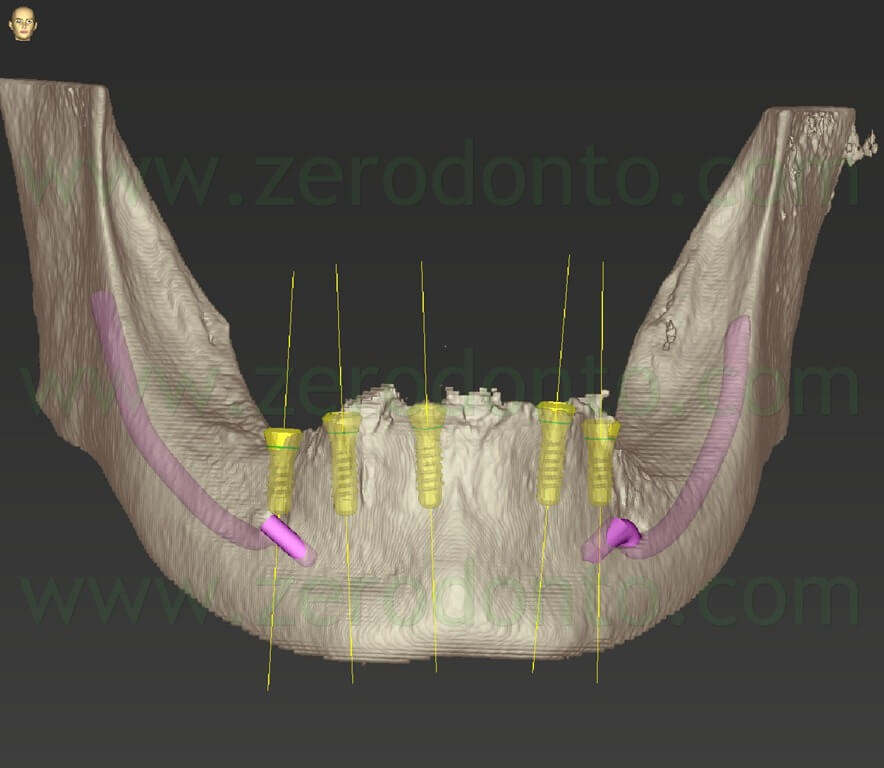
A prosthetically-guided criterion was used to plan the insertion of the implants, on the basis of the position of the barium-painted teeth. In the mandible, 5 Roxolid SLActive Straumann implants with a diameter of 3.3 mm were planned.
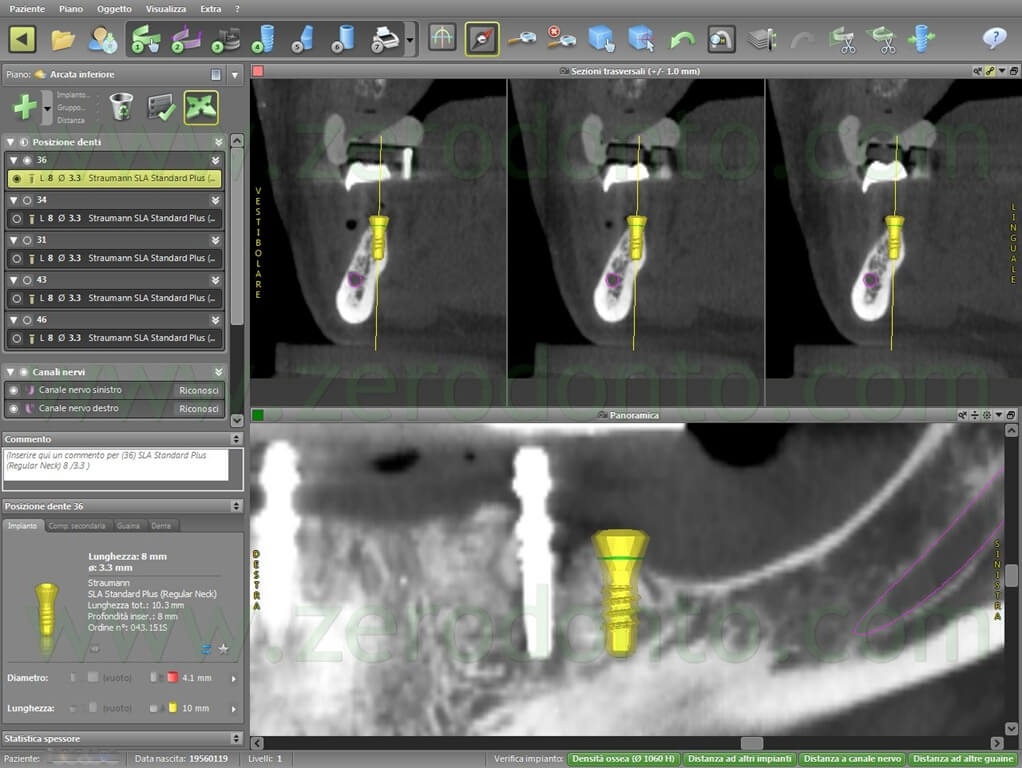

After checking the congruence of the prosthetic planning, the sleeves for the guided surgical drills were virtually placed.
A similar approach was used in the planning of the maxillary arch. Careful attention was dedicated to the planning in the anterior maxilla, because of the high esthetic value of this area. Consequently, the Codiagnostix was asked to remove the extraoral soft tissues, so as to visualize the prosthesis in relation to the bone.
In the maxillary arch, 6 Roxolid SLActive Straumann implants were planned, 4 with a diameter of 3.3 mm in the anterior area and 2 with a diameter of 4.1 mm in the posterior regions.
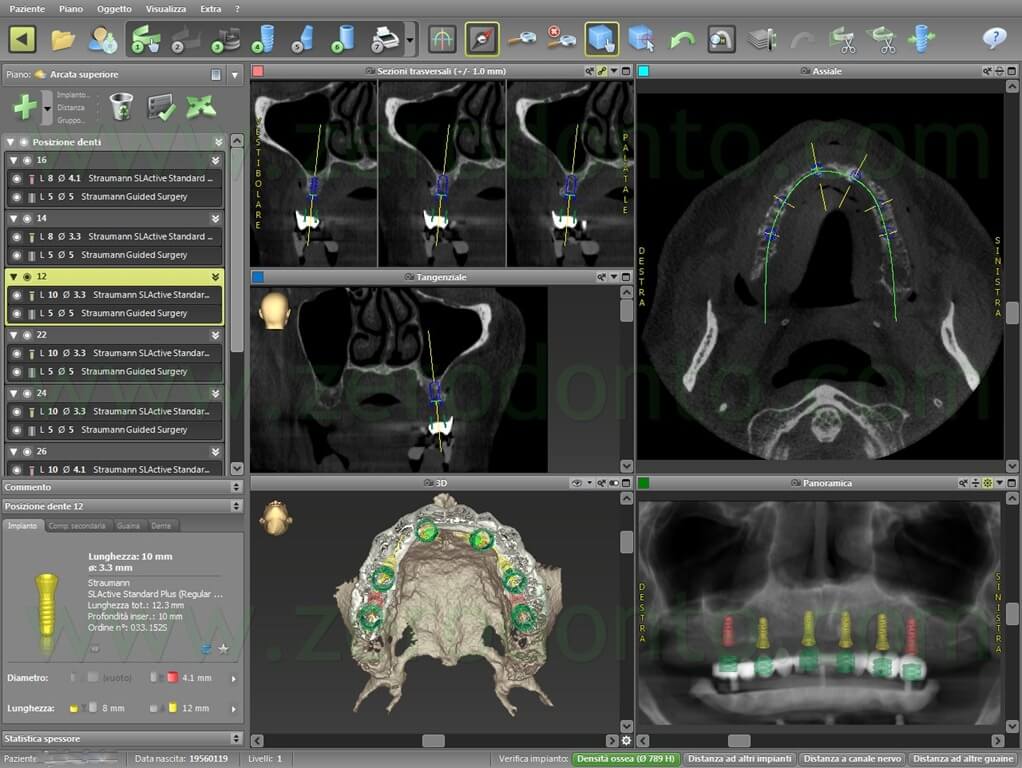


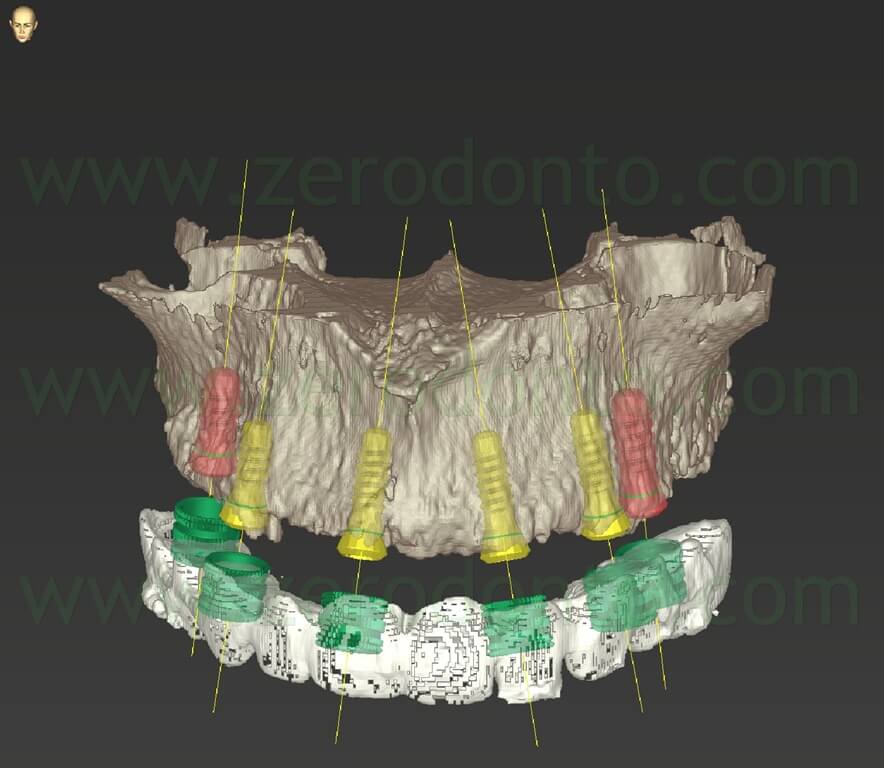
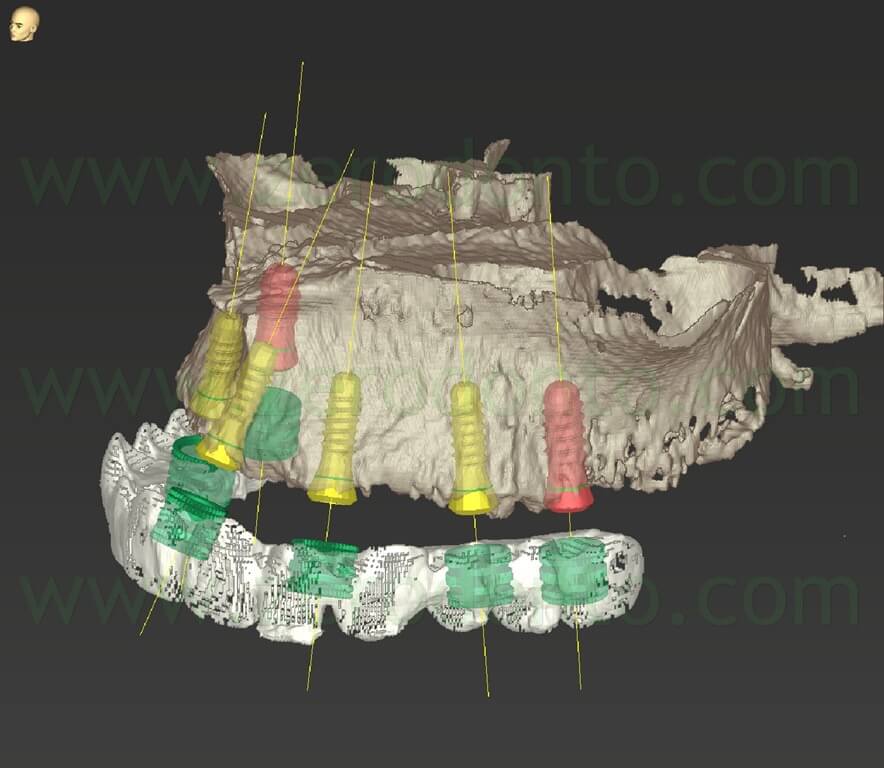
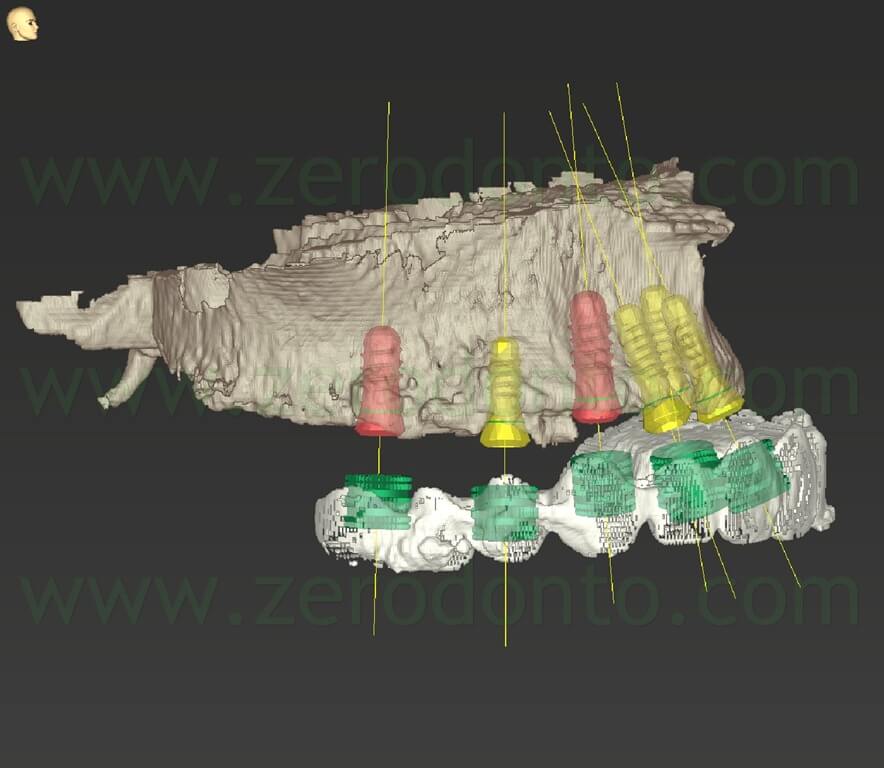


According to the Straumann protocol, the mandibular surgical template was stabilized using the temporary mini-implants. Conversely, since to date the guided-surgery protocol allows to fabricate only bone/mucosal-supported surgical templates, it was decided to improve the stability of the maxillary surgical templates modifying the standard protocol and planning 3 non-axial stabilization pins.
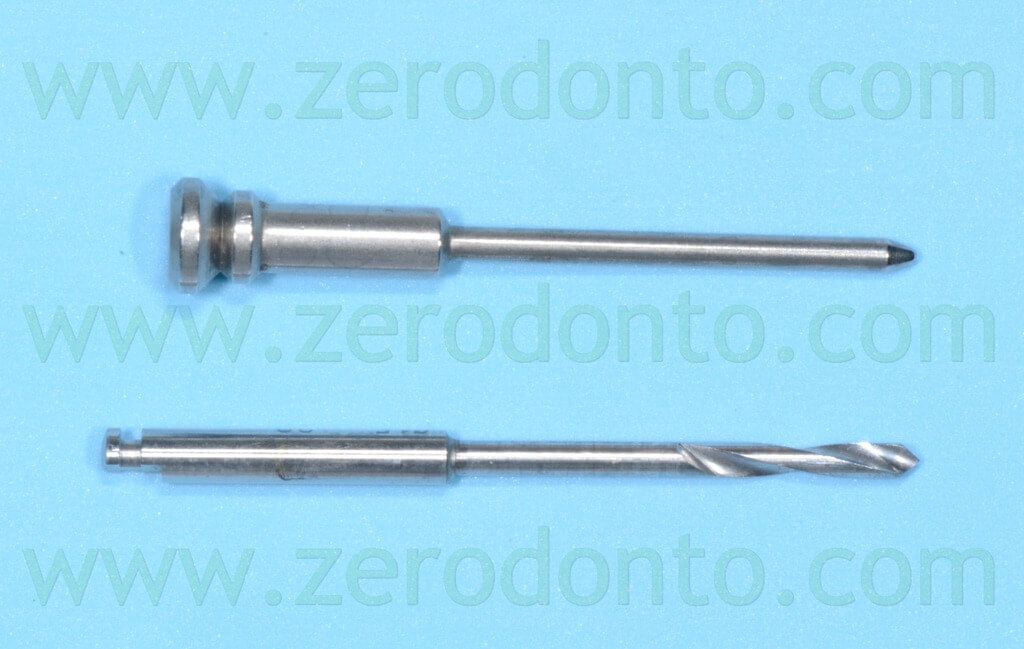
On the basis of previous clinical experiences (Nobel Guide Implant-Guided Surgery With Nobel Clinician Software) as well as to simplify the surgical procedures, it was decided to use 3 guided stabilization pins by NobelBiocare.
In order to perform a guided planning of the position of the stabilization pins, 3 Straumann Bone Level implants with the relative sleeves were virtually positioned in the maxilla; such a choice was made since the NobelBiocare sleeves fit with light friction into the Straumann sleeves of the 3.3 mm-diameter implants.
Although the Codiagnostix allows for the placement of custom made implants, pins and sleeves, it would not have been possible to insert such sleeves in the surgical templates using the Gonyx, since the device only uses Straumann components.
As a consequence, Straumann sleeves overdimensioned to NobelBiocare stabilization pins were chosen. The fitting procedure will be described in the laboratory procedures.
The Bone Level implant was planned so as that the sum of its length, the sleeve and the sleeve/implant distance would be equal to the length of the NobelBiocare pin.
Due to the limitations of the coordinate system of the Gonyx, it was possible to plan the pins with a maximum angulation of 45° to the sagittal plane; consequently, the three-dimensional placement of the pins was not optimal (e.g. perpendicular to the longitudinal axis of the maxilla).
In order to overcome such a problem and maximally stabilize the surgical template, 2 buccal and 1 palatal pins were planned; finally it was carefully checked that their position did not interfere with either any anatomical structure or the guided implants.
FABRICATION OF THE MASTER CASTS
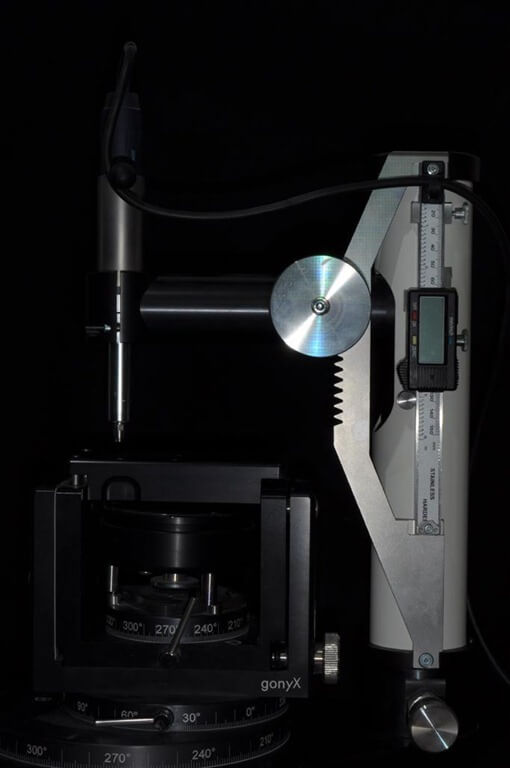
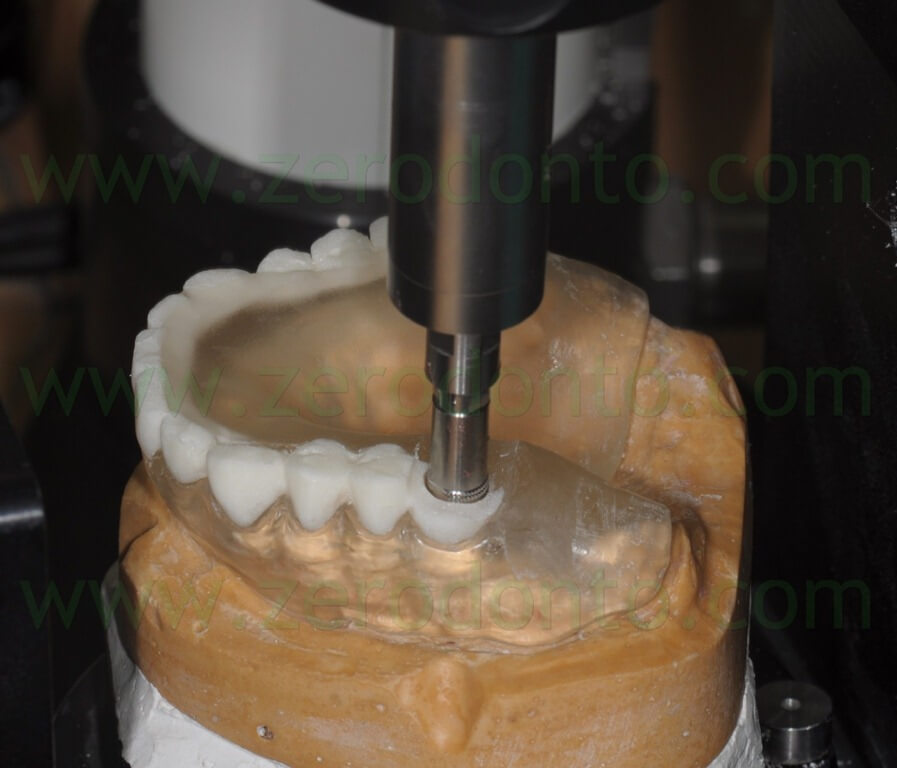
The Gonyx is a mechanical precision device created to transform the radiological indexes in surgical templates. It is made up of a rotating and angulating (with defined limitations) platform to mount the master cast; moreover, the Gonyx is provided with a digital caliper mounted on a vertical arm used to drill the templates and insert the sleeves.
Once the guided planning is completed, the Codiagnostix prints a paper verification template using a calibrated printer; the verification template has to be mounted on the platform of the Gonyx.
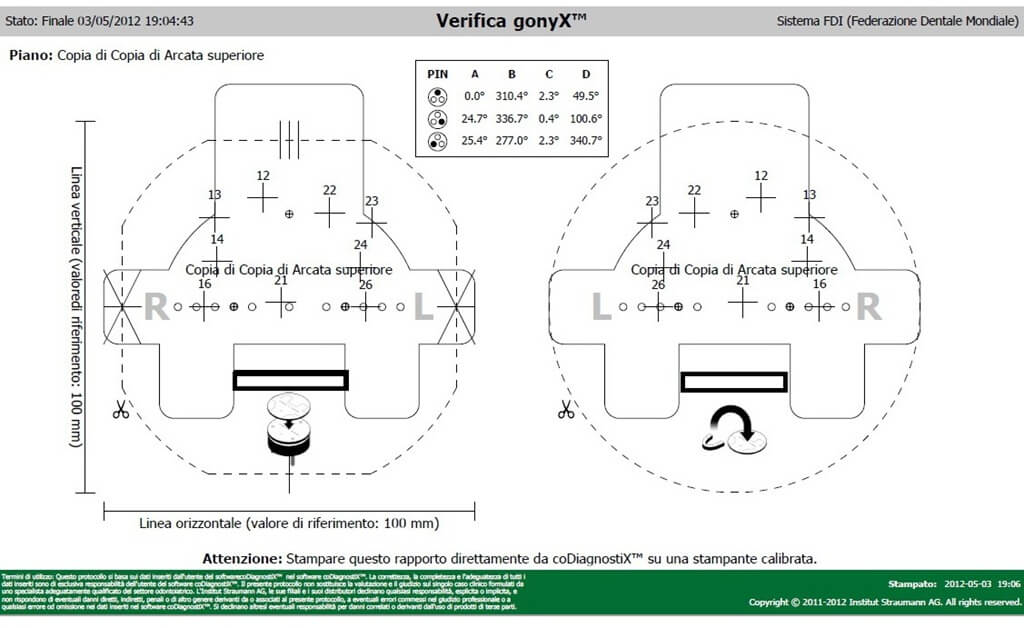
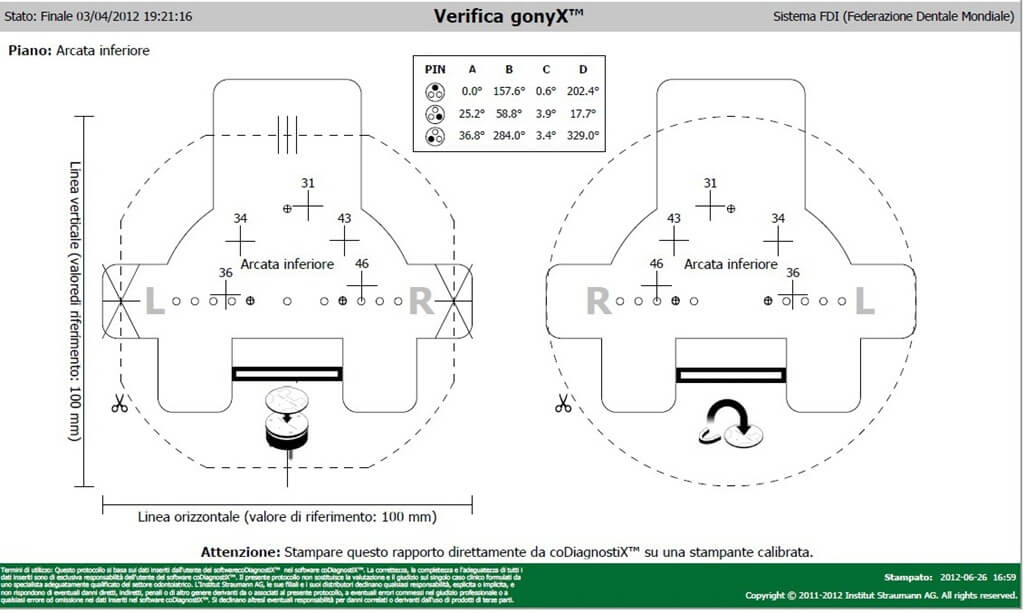
The verification template has to be manually aligned with some reference lines and is stabilized on the platform using 3 little magnetic spheres. The verification procedure starts with the identification of a reference point called “zero point”; this point allows to match the center of a cross printed on the verification template for each guided implant with the vertical arm of the Gonix.



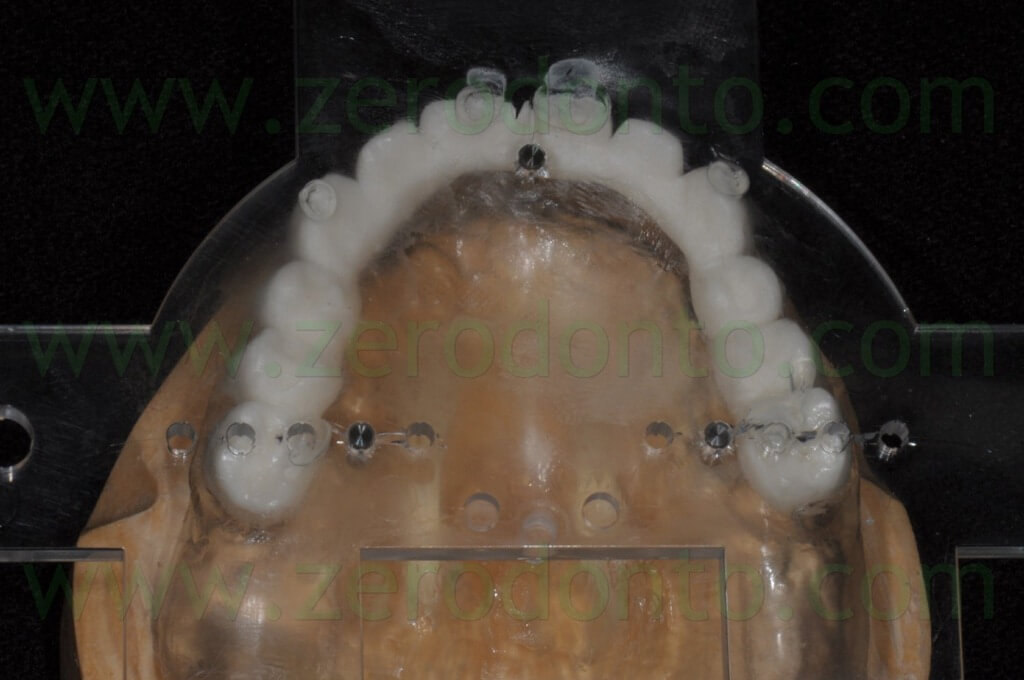
The barium-painted teeth were properly cut so as not to interfere with the components used to place the sleeves.


Then, the holes for the sleeves were drilled on the basis of the three-dimensional coordinate system achieved at the end of the virtual planning. The sleeves were blocked in the surgical template using acrylic resin.

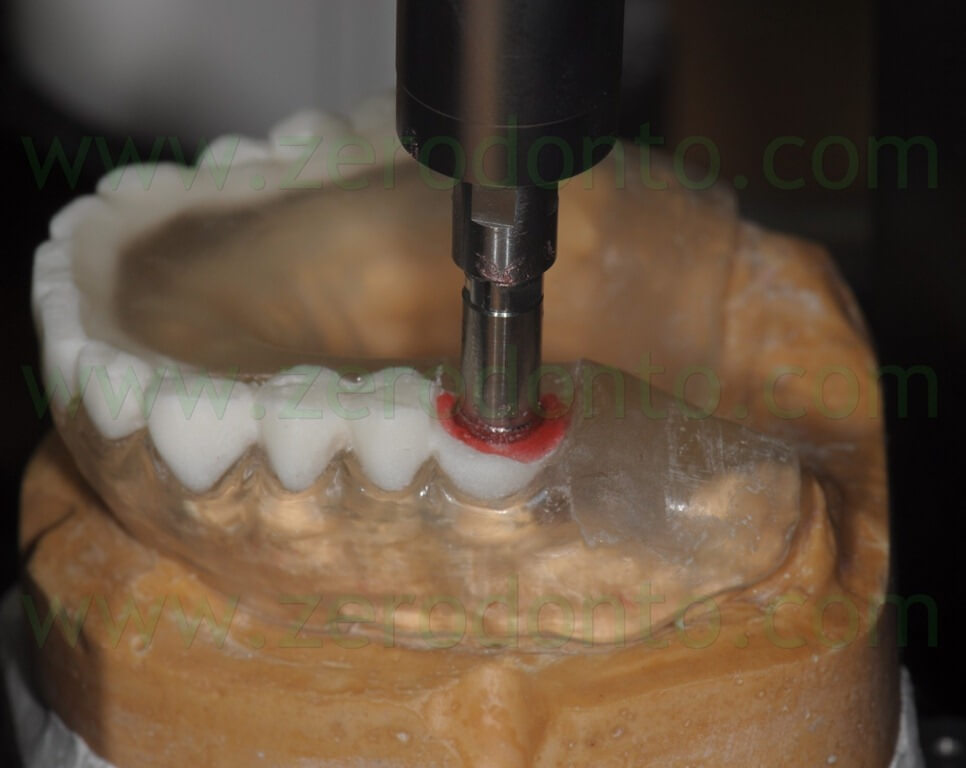

Il corretto posizionamento in altezza di ciascuna boccola è stato verificato per mezzo di un apposito puntale che frizionava su un cartoncino di verifica senza deformarlo.


The correct heigth and placement of each sleeve was verified by means of a specific pin frictioning on a verification paper with no deformations.
Once all the sleeves were placed, the stabilization pins were inserted in the maxillary surgical template; 3 pins with an angulation of 45° to the sagittal plane were placed.
In order to correctly use the Gonyx components, 3 Straumann sleeves were inserted in the surgical template; then, 3 smaller NobelBiocare sleeves slightly frictioning in the Straumann ones were bonded into the latter using cyanoacrylate. Such a procedure allowed to use the calibrated guided drills and pins (not available for the Straumann guided system at the moment of the described surgical procedures).







In order to guarantee a proper intraoperatory stability of the surgical template, it was decided to insert 8-9 mm deep the stabilization pins in the maxilla.




The congruence between the sleeves and the implants on the master casts was checked using a stereomicroscope.


PREPARATION OF THE IMMEDTAELY-LOADED SCREWED TEMPORARY PROSTHESES
Once the surgical templates were completed, they were used to fabricate the immediately-loaded screwed temporary prostheses. To date, the Straumann guided system does not allow to plan immediately-loaded impants with a standard protocol; as a consequence, a modified procedure was set up by the authors. A guided mounter per implant (suitably taken from new guided implants) was screwed onto each implant analog on the master casts, using the guided stop keys to assemble them at the correct heigth indicated by the virtual planning.






Once all the mounters were fixed, the dental technician blocked the implant analogs in newly produced master casts to fabricate the temporary prostheses.



A removable complete denture was made on the maxillary model; such a denture was to be used as temporary removable prosthesis soon after the mandibular surgery. The occlusion of the denture was optimized to match with the mandibular fixed temporary prosthesis.



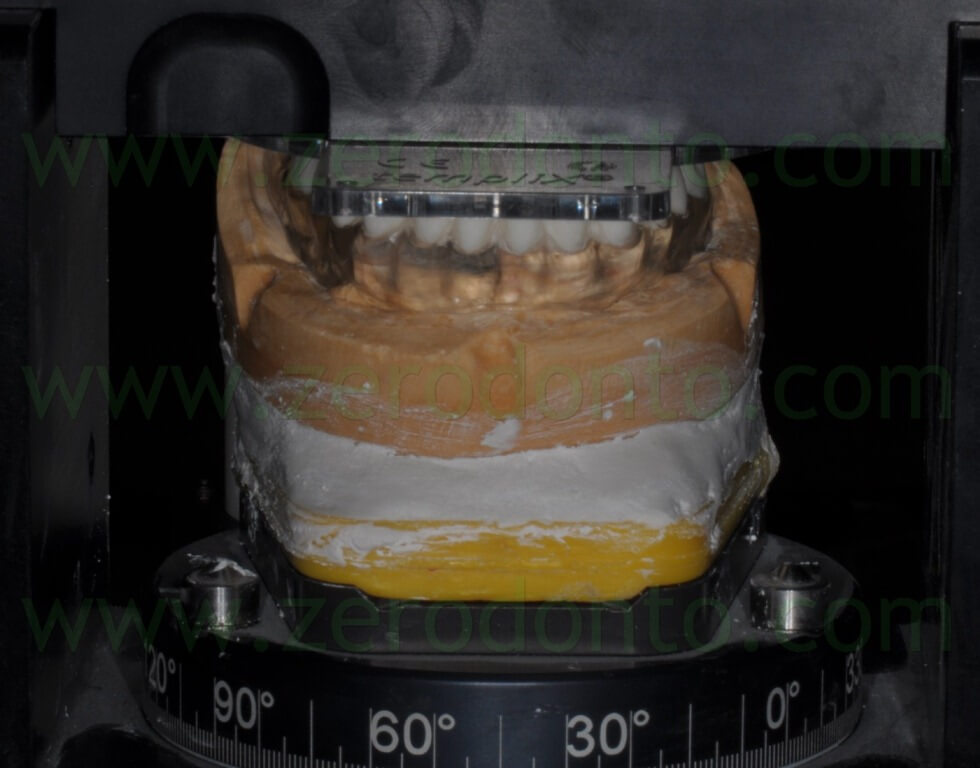
The screwed temporary full-arch restorations were fabricated by means of casted metal frameworks blocking all the temporary cylinders of each arch. The morphology of the buccal surfaces of teeth was duplicated using silicon indexes recorded during the study stage of the clinical case.
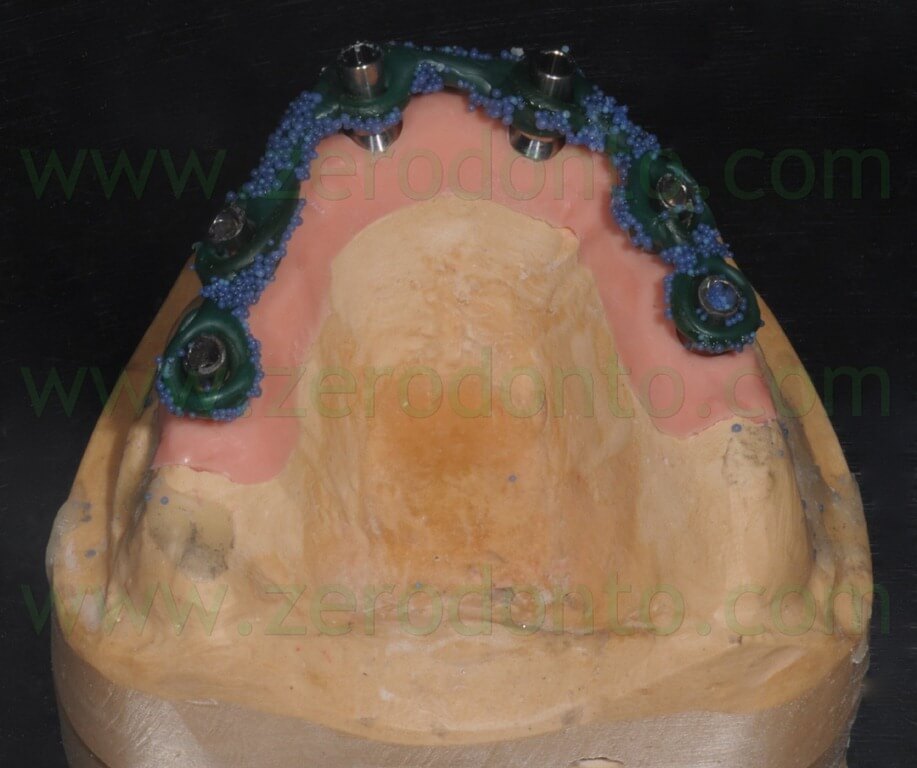


Once the screwed temporary prostheses were completed, the prosthetic cylinders were blocked to the superstructure with an indirect-direct technique, using a little amount of flowable composite resin; consequently, although the position obtained on the master casts was kept, it would have been possible to easily detach and block again each cylinder during the intraoral relining procedures.
In fact, although the virtual planning is very precise, the more implants have to be placed the higher risk of misfit can occur, due to radiological distortions or procedural variations.













Finally, the temporary prostheses were finished and polished. Particular care was dedicated to the access to implant necks, so as to ease and optimize the hygienic home maintenance.
MANDIBULAR ARCH: SURGICAL PROCEDURES
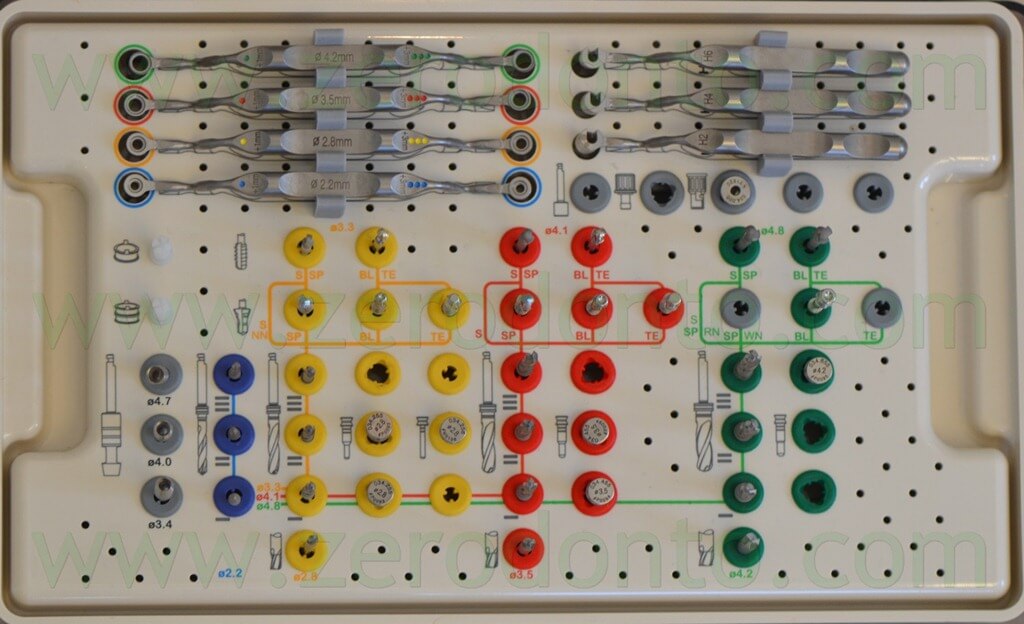
The guided surgical procedures were made on the basis of the virtual planning, using a kit dedicated to guided-surgery.
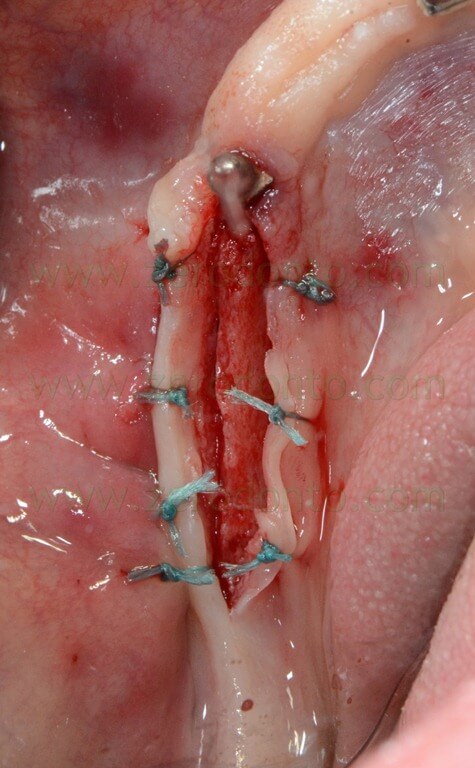
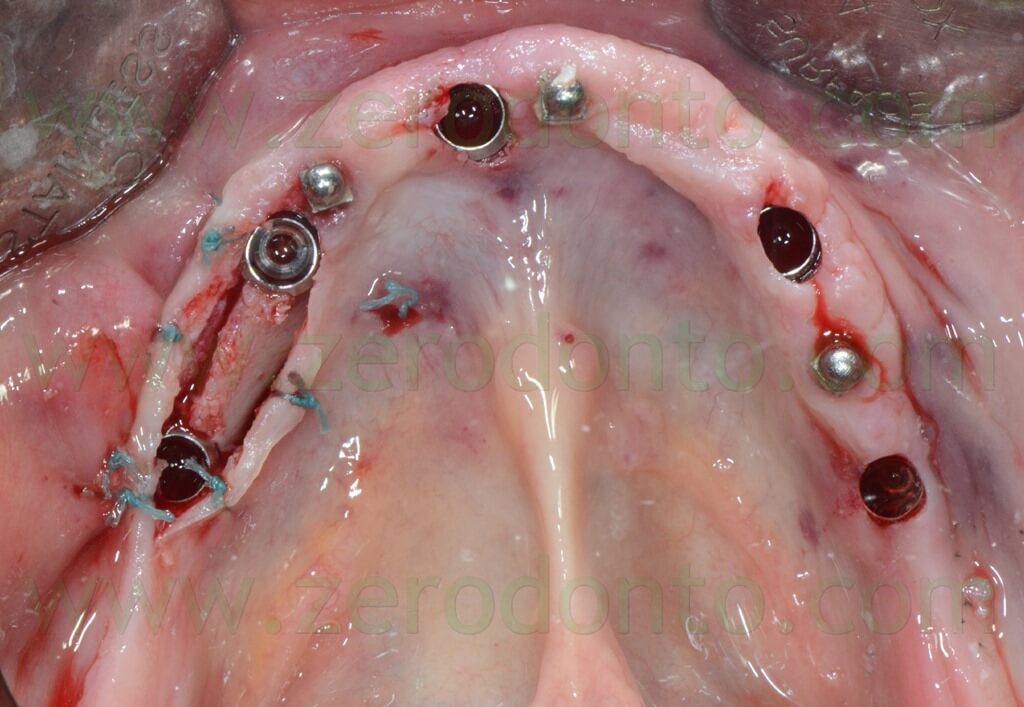
First, the mandibular surgery was performed, since a lack of keratinized tissue was evidenced in the right posterior emiarch. In order to overcome such a condition, it was planned a full thickness flap in this area, so as to preserve as much buccal soft tissue as possible.
Once the position of the single attachments was verified not to interfere with the sleeves, the surgical template was modified in the area of the surgical incision, in order to make a divaricating suture.






The surgical template was cold sterilized and intraorally stabilized using the temporary mini-implants. Buccal and lingual local anesthesia was injected as well as at level of the implant sites.
Then, the position of the right posterior implants was marked, in order to make the incision slightly lingually and reposition the buccal mucosa more apically.
Once the surgical template was removed, the incision and the divaricating suture were made.



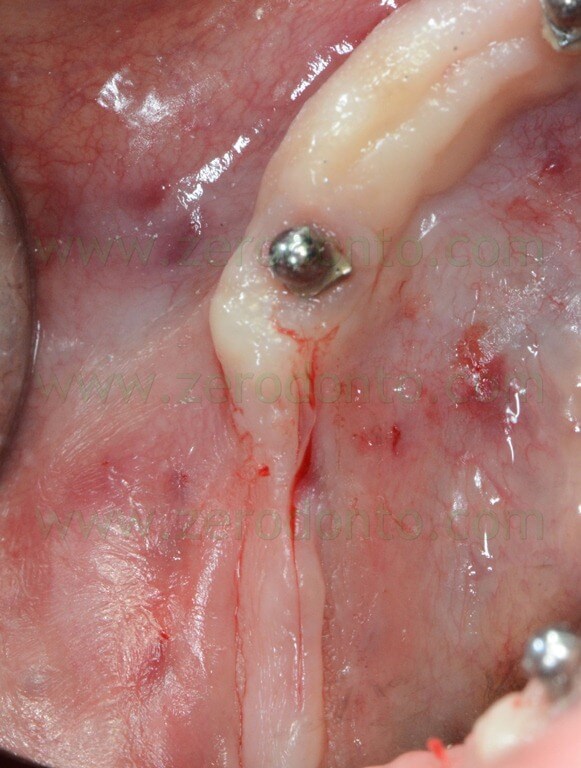
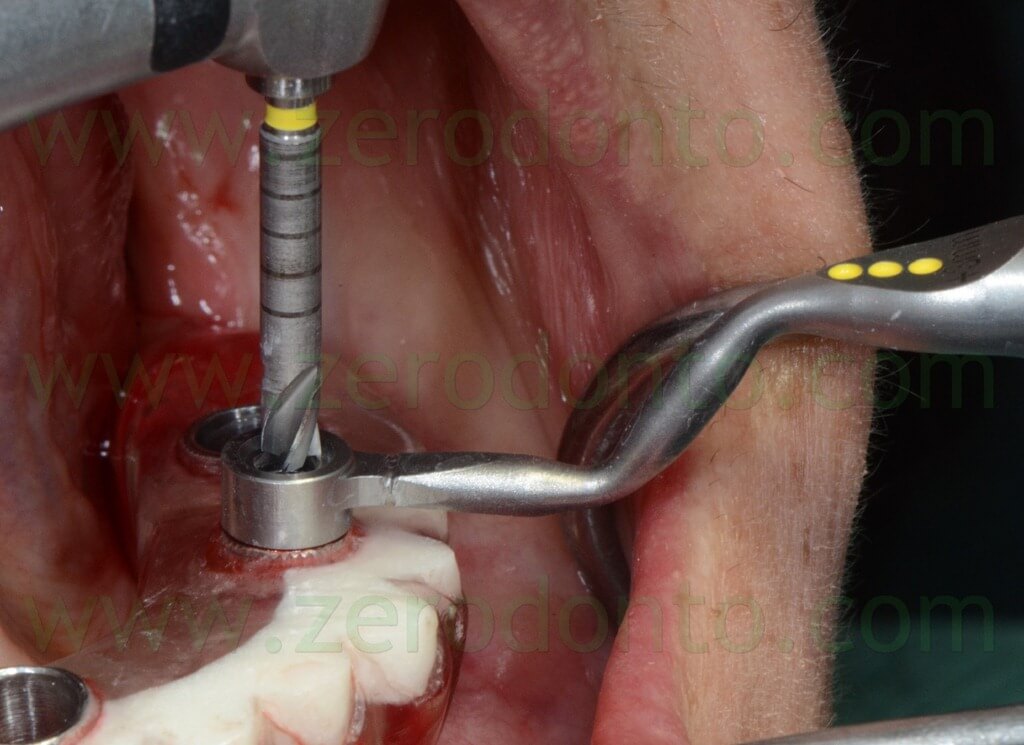
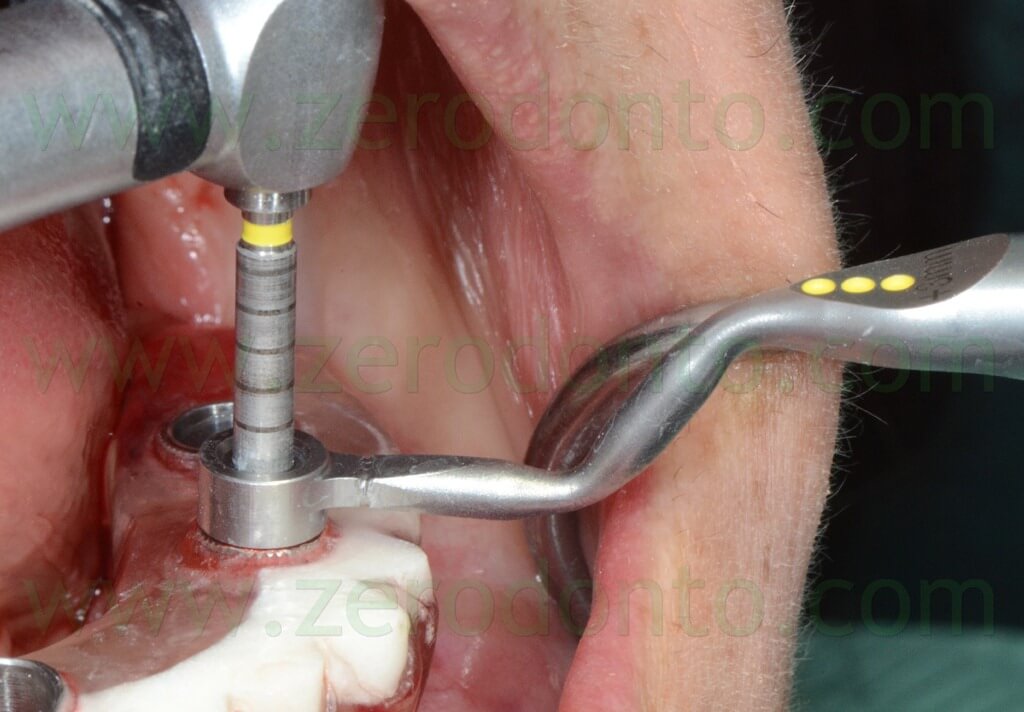
Then, the surgical template was stabilized again on the mini-implants and a guided mucotome and hand instruments were used to remove the mucosa from the implant sites.



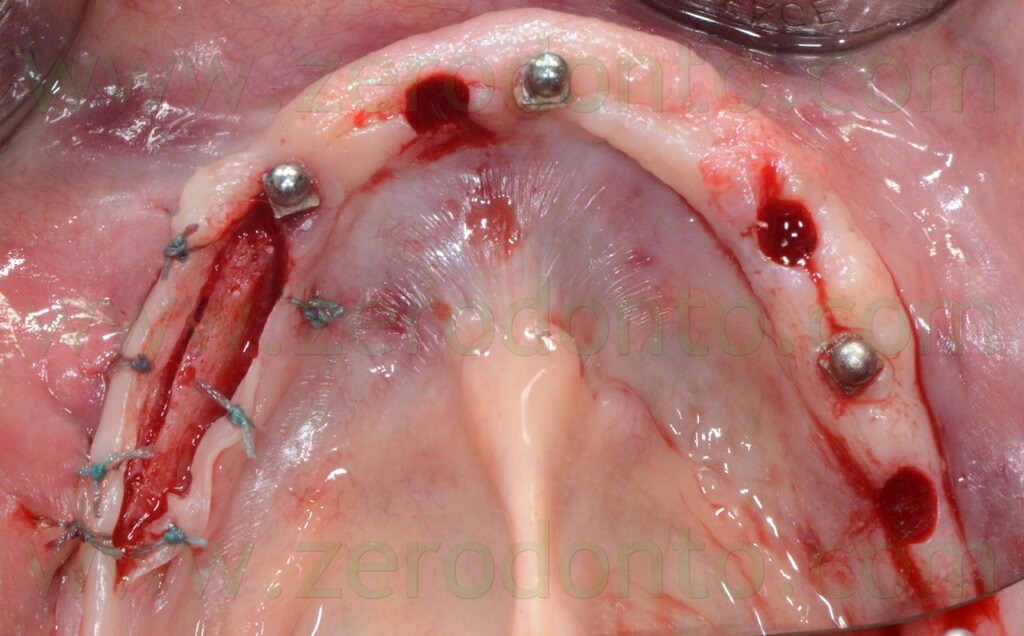
The implants were placed one by one, so as to avoid possible imprecisions that would have exerted friction on the surgical template, negatively affecting the precision of the virtual planning and the placement of the temporary prosthesis.
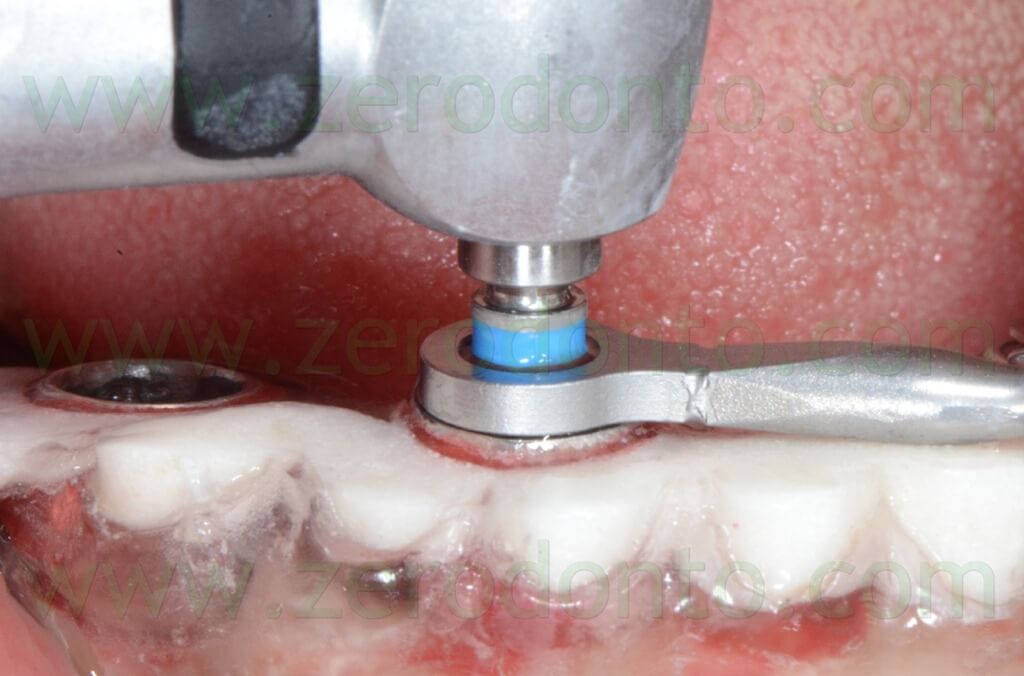
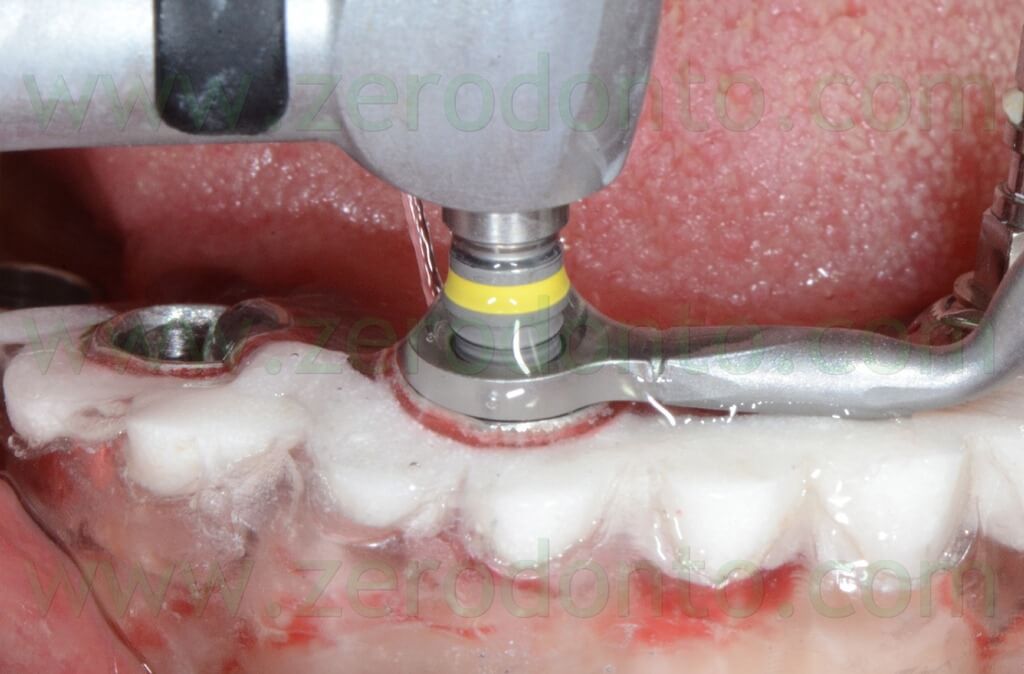
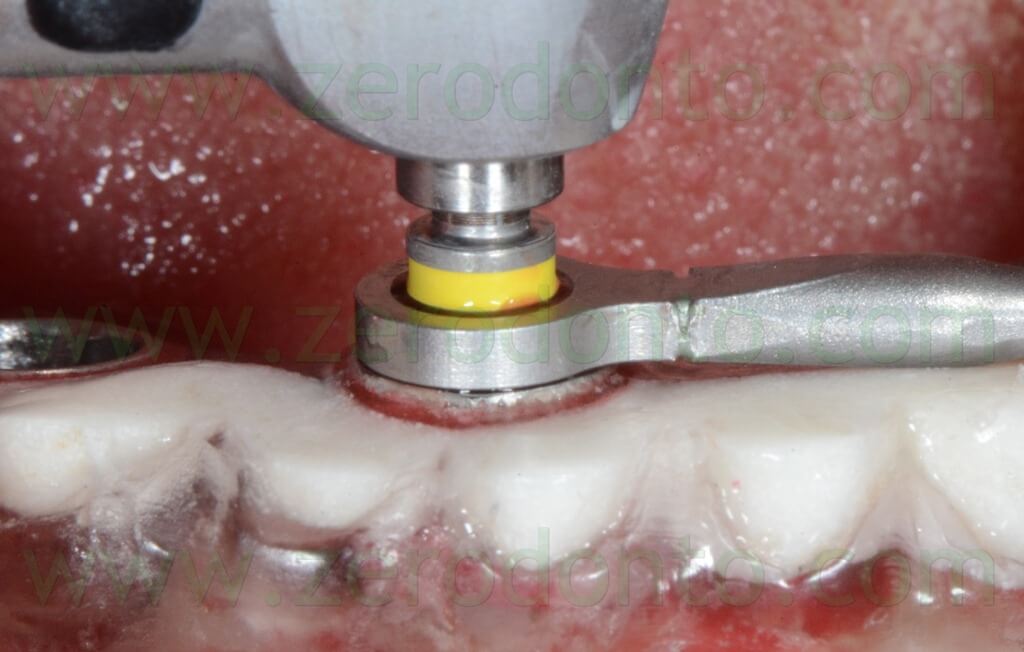
Each implant site was prepared according to the Straumann guided surgical protocol. The coronal-apical position of each drill was checked using the guided handles inside the sleeves. The surgical components can be easily identified by means of colors and reference symbols indicated in the planning printed by the Codiagnostix.
At the end of the preparation using a coronal drill, each site was irrigated with saline solution and the precision between the sleeve hole and the implant position carefully evaluated. The Straumann guided system allows to use fixing pins to be placed into the sleeves and the implant sites to provide further stabilization to the surgical templates during surgery.
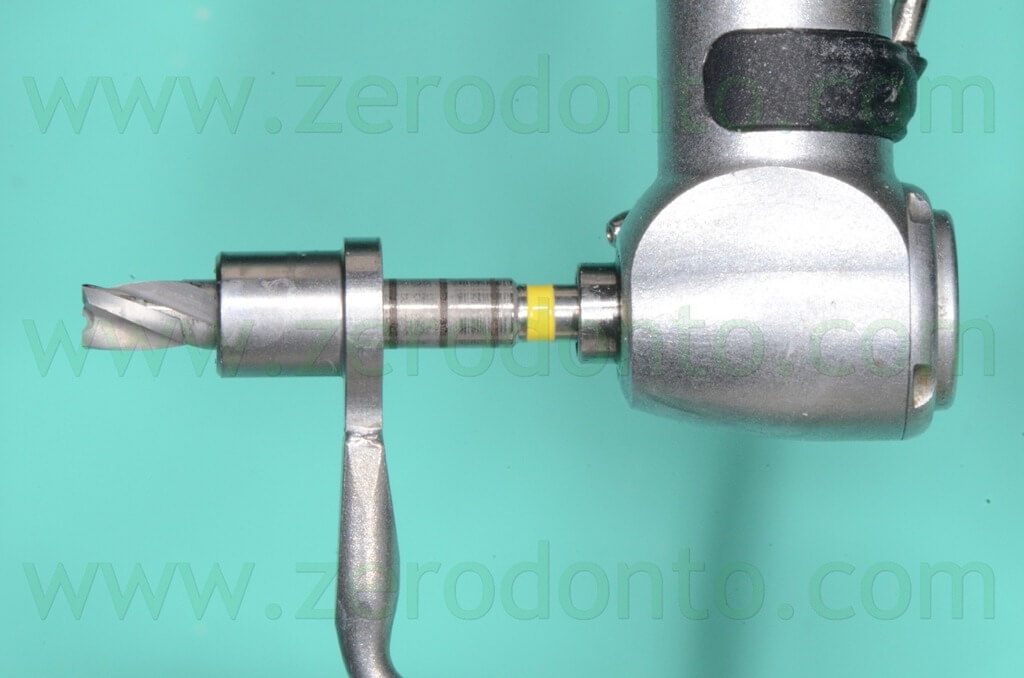



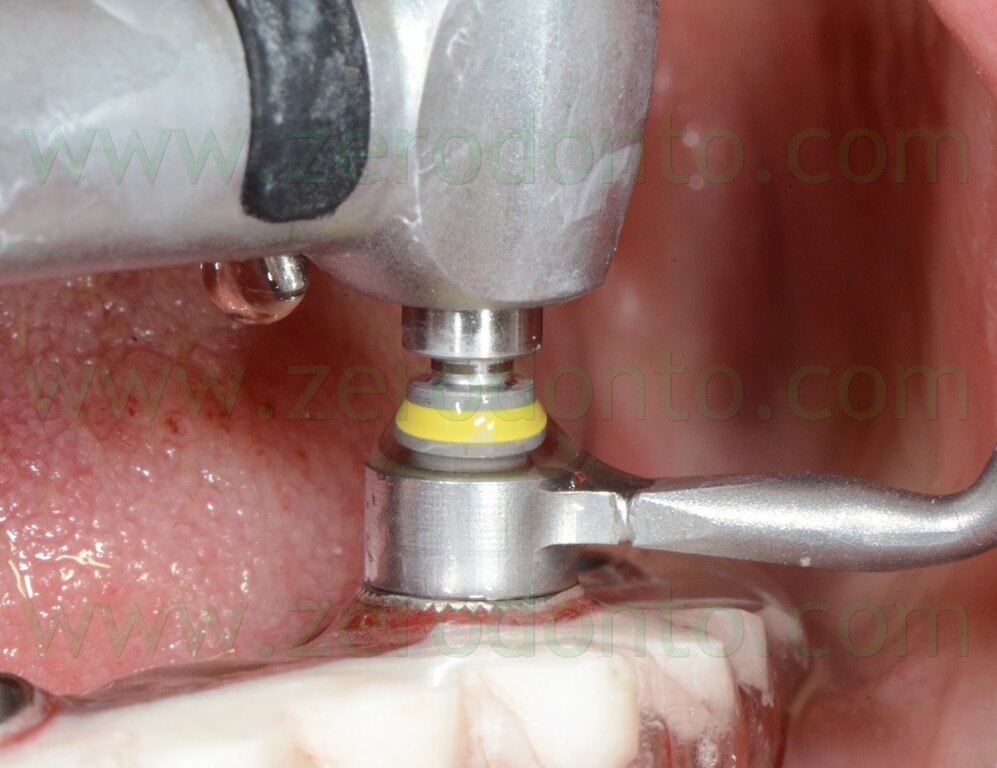


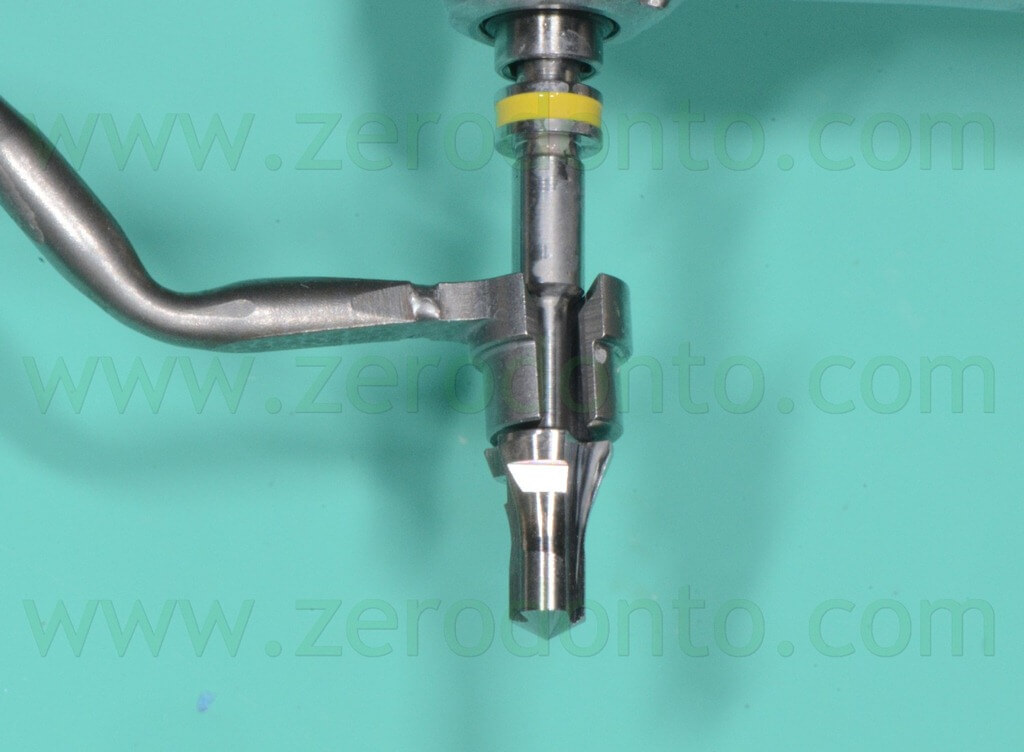

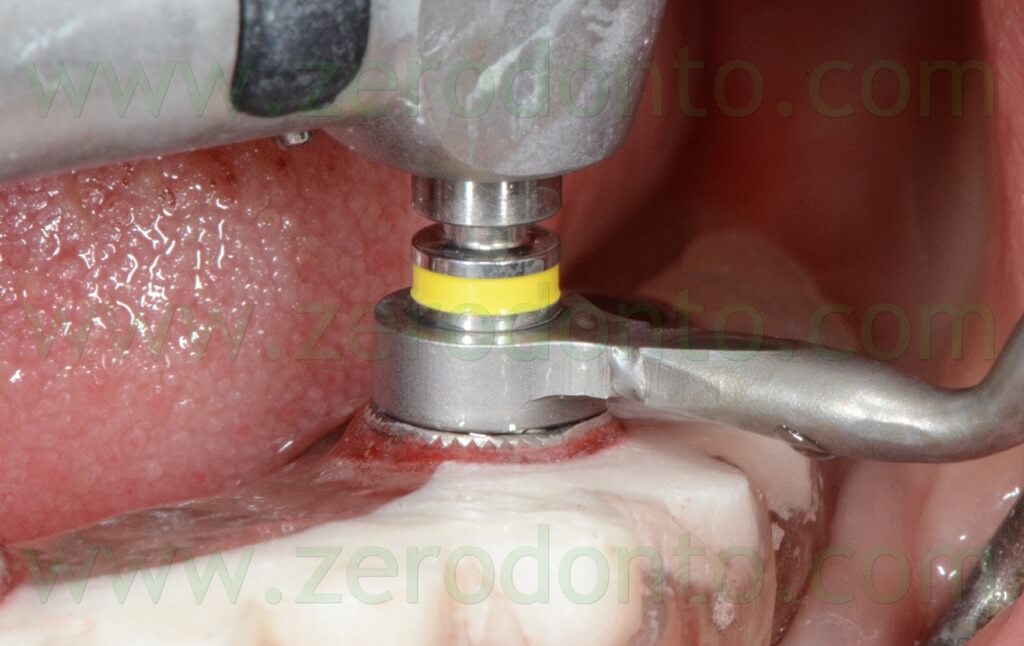



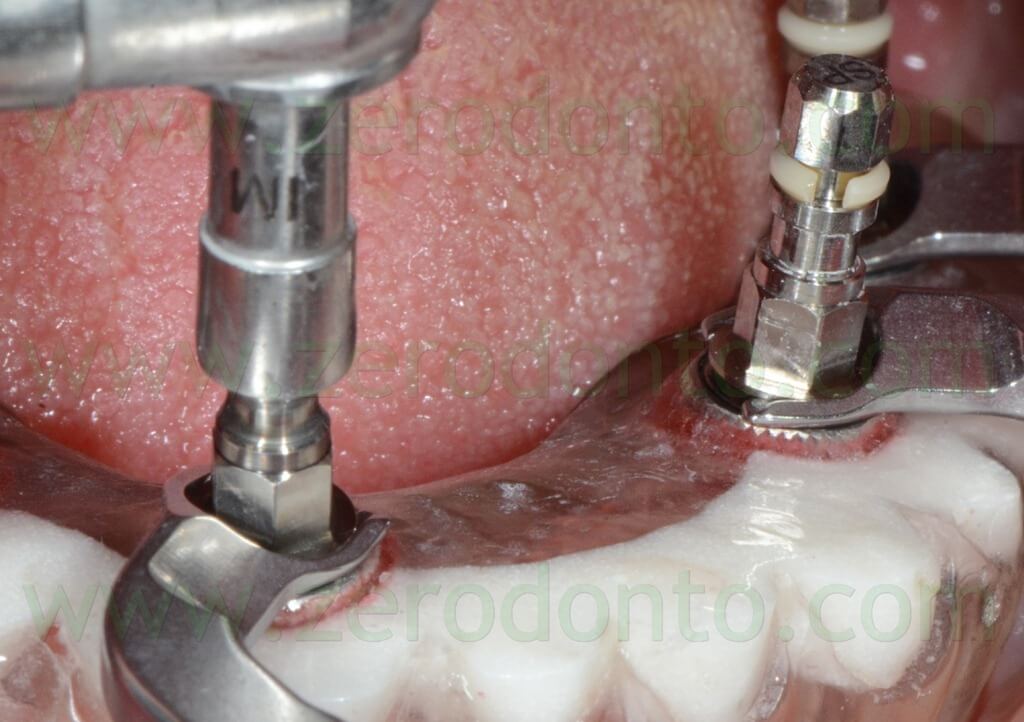
The Roxolid SLActive implants were inserted carefully so as not to touch the sleeves in order to avoid any alteration of the implant surface. The coronal-apical position of each fixture was checked by means of the reference lines marked on the implant mounters. Finally, the fixtures were screwed manually using the stop keys.
It is advisable to remove the stop keys only after achieving a valid mechanical grip of the implant mounter and to verify the correct position of the mounter itself. In order to achieve the best precision (particularly in the presence of solely bone/mucosal-supported surgical templates), it is better to leave the stop keys in situ until all the fixtures have been screwed, to avoid undesired vertical micro-movements of the surgical template.
Although a dynamometric wrench is used, it is worth remembering that it is not possible to precisely evaluate the insertion torque values and the relative primary stability until the surgical template has been removed; such a phenomenon is due to the mechanical friction given by the template itself that can affect the manual sensitivity of the surgeon.








The above mentioned clinical procedures were carefully performed till the correct insertion of all the fixtures. Then, the surgical template was removed and standardized periapical radiographs were made to check the proper placement of the fixtures.











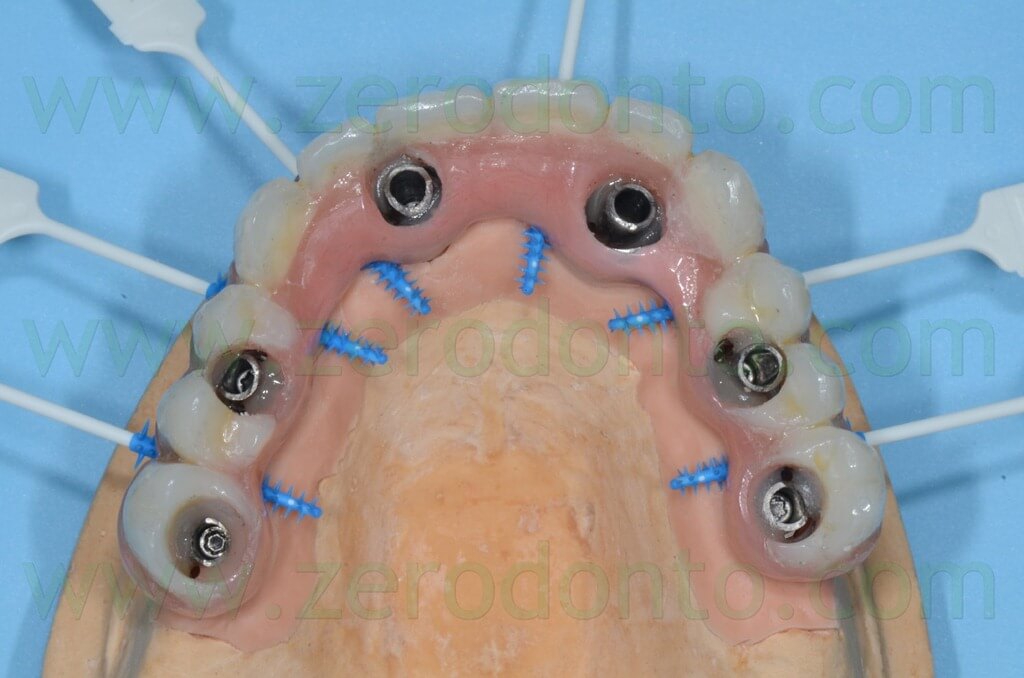
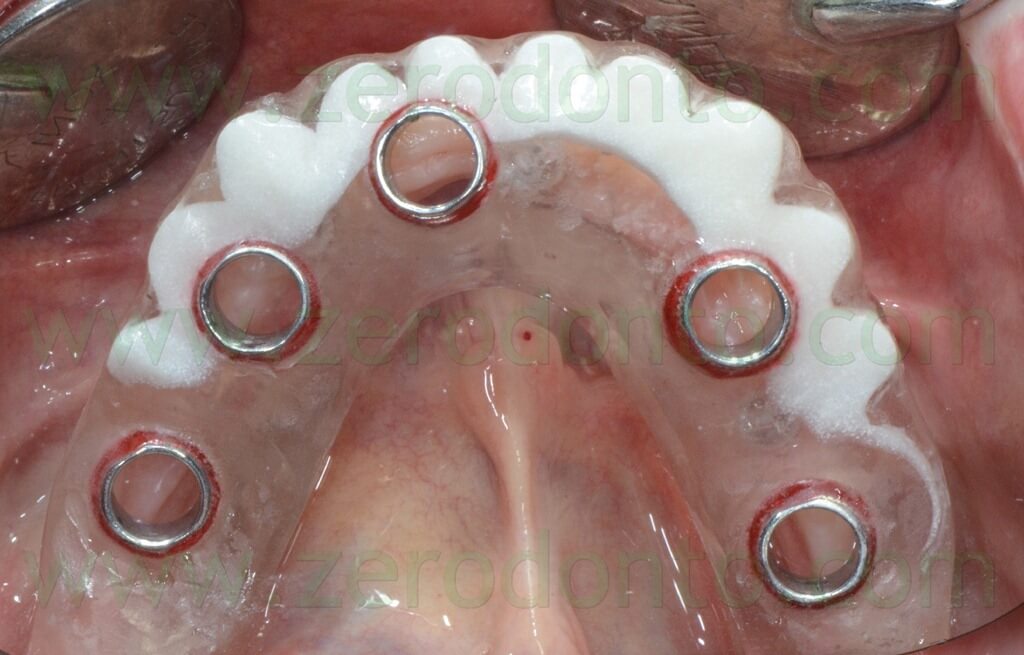
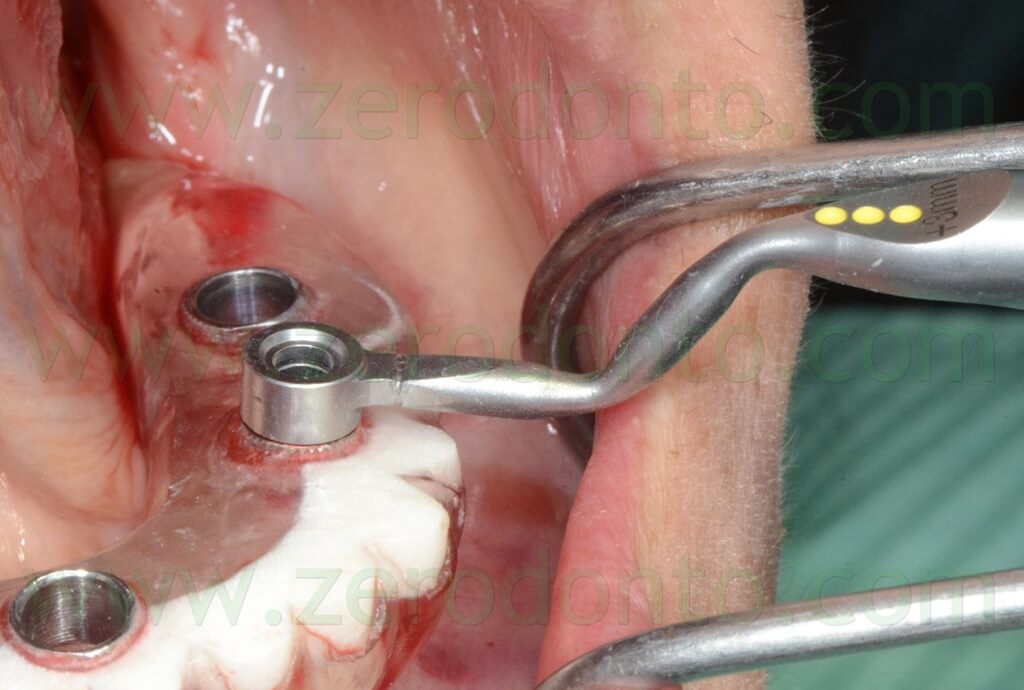
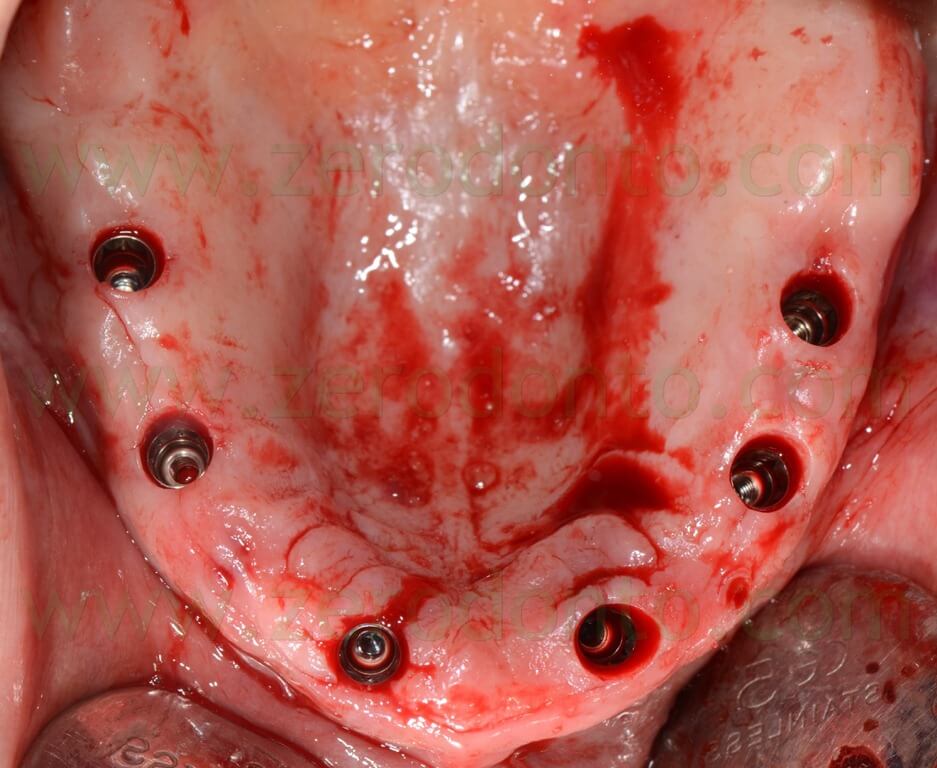
MANDIBULAR ARCH: PROSTHETIC PROCEDURES
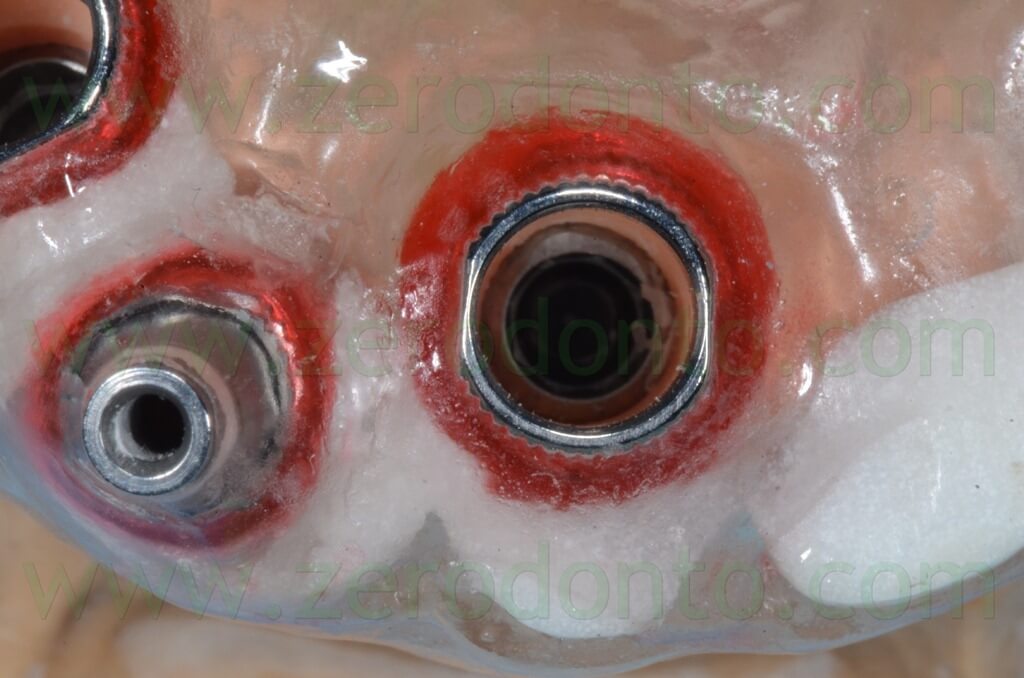
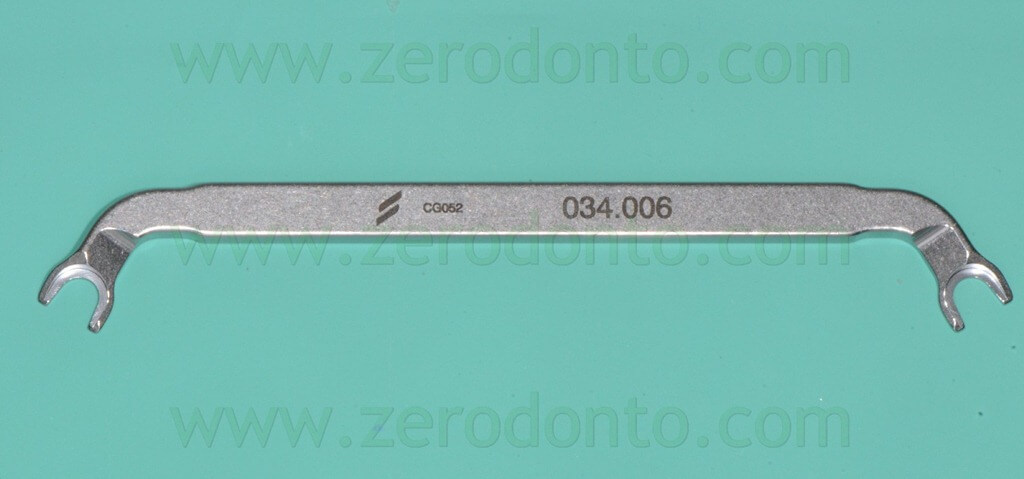
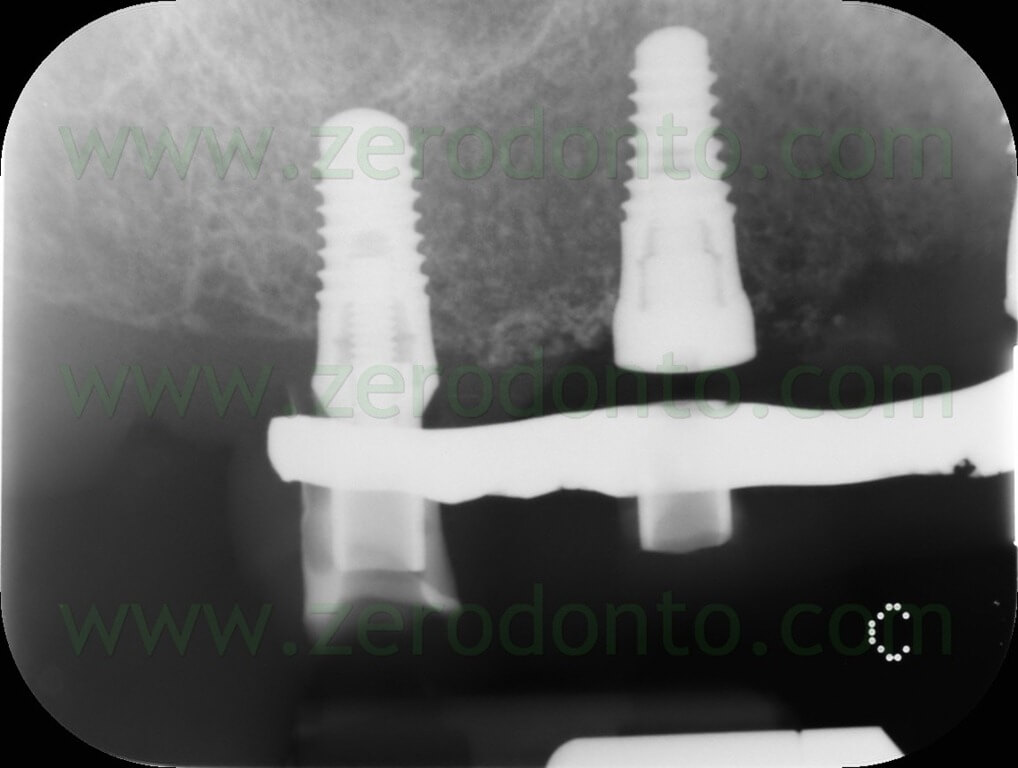
Before placing the temporary prosthesis intraorally, the neck of the prosthetic cylinders was cleaned with 1% chlorexidine gel. A manual dynamometric wrench was used to tighten the prosthetic screws at 15 Ncm. The fit between the prosthetic cylinders and the fixtures was verified by means of standardized periapical radiographs.
The prosthetic passive fit was optimal onto all the implants but the fixture in region 36, where a gap was evidenced. Consequently, the flowable resin composite blocking the cylinder was broken forcing the screw tightening.




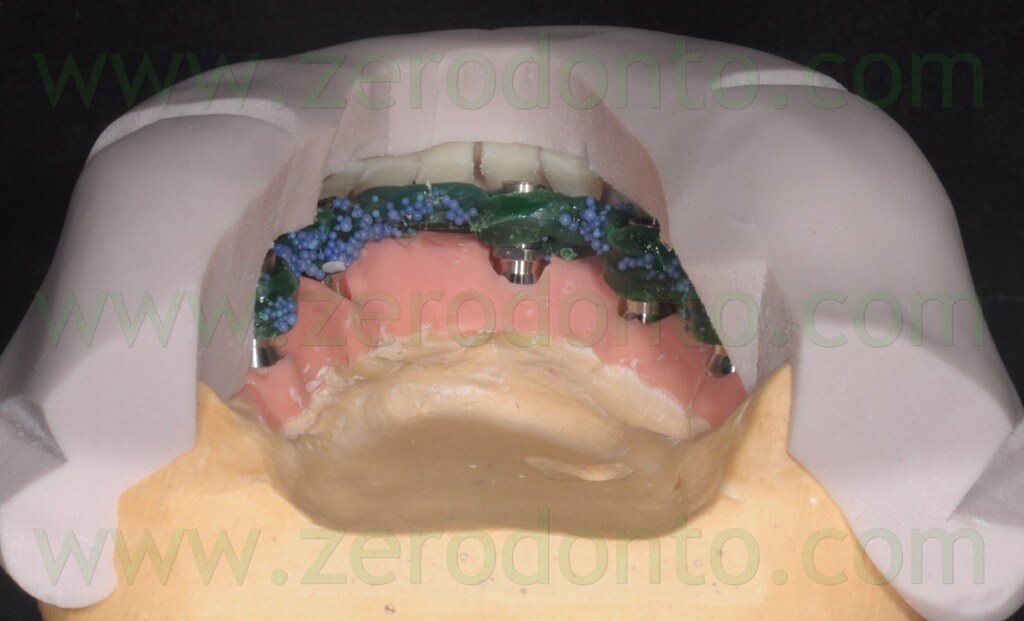
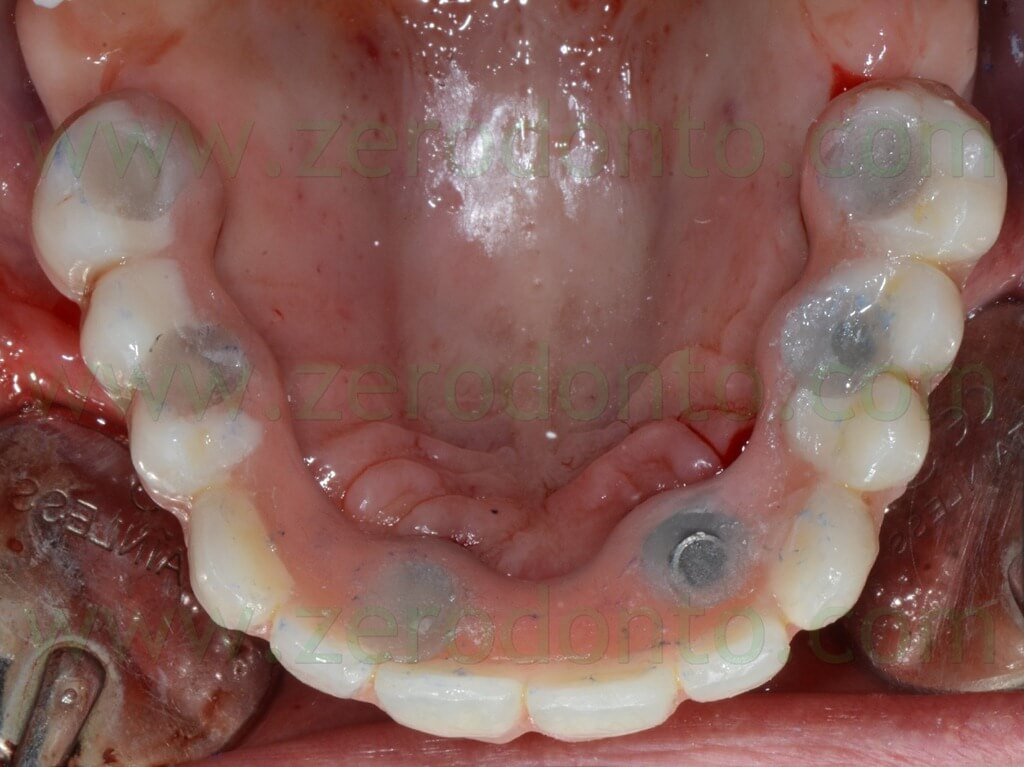
Once the proper fit of the components was achieved, the screwed full-arch prosthesis was relined intraorally with self-polymerizing acrylic resin. Finally, the prosthesis was polished and finished.







The immediately-loaded temporary prosthesis was screwed intraorally at 32 Ncm using a dynamometric manual wrench. As previously described, the proper fit between the implant-prosthetic components was verified by means of standardized periapical radiographs. The prostehtic screws were covered with cotton pellets and the access holes filled with a light-curing composite resin material.



Careful attention was dedicated to the control of possible compression areas as well as to the access to implant necks, so as to guarantee the hygienic maintenance of the restoration.
Finally, the temporary removable complete denture was placed at the maxillary arch and the occlusion was carefully checked both in centric occlusion and in lateral movements.
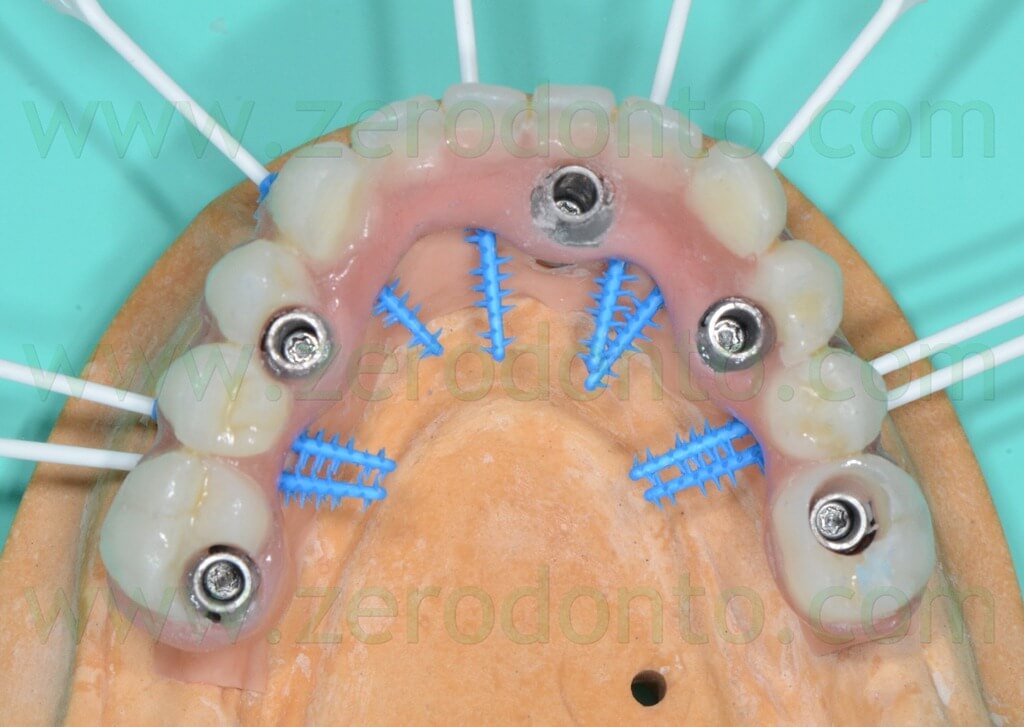
MAXILLARY ARCH: SURGICAL AND PROSTHETIC PROCEDURES
The maxillary surgery was performed 2 weeks after the placement of the mandibular implants. The procedures were comparable to those described for the mandibular arch.
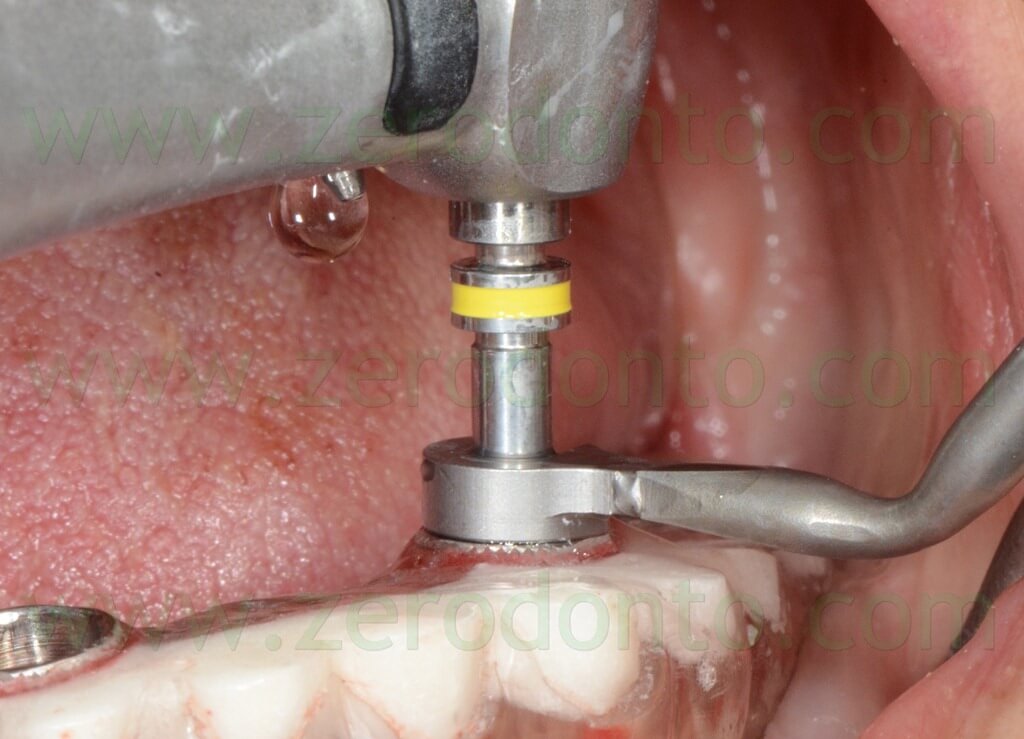
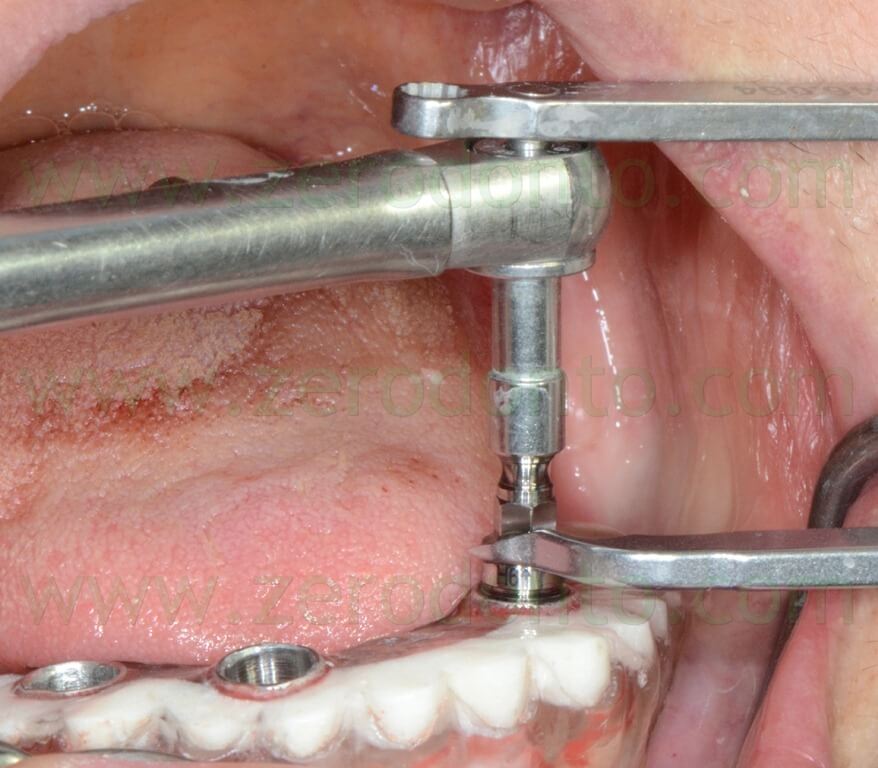
The surgical template was fixed by means of NobelBiocare stabilization pins as previously described.

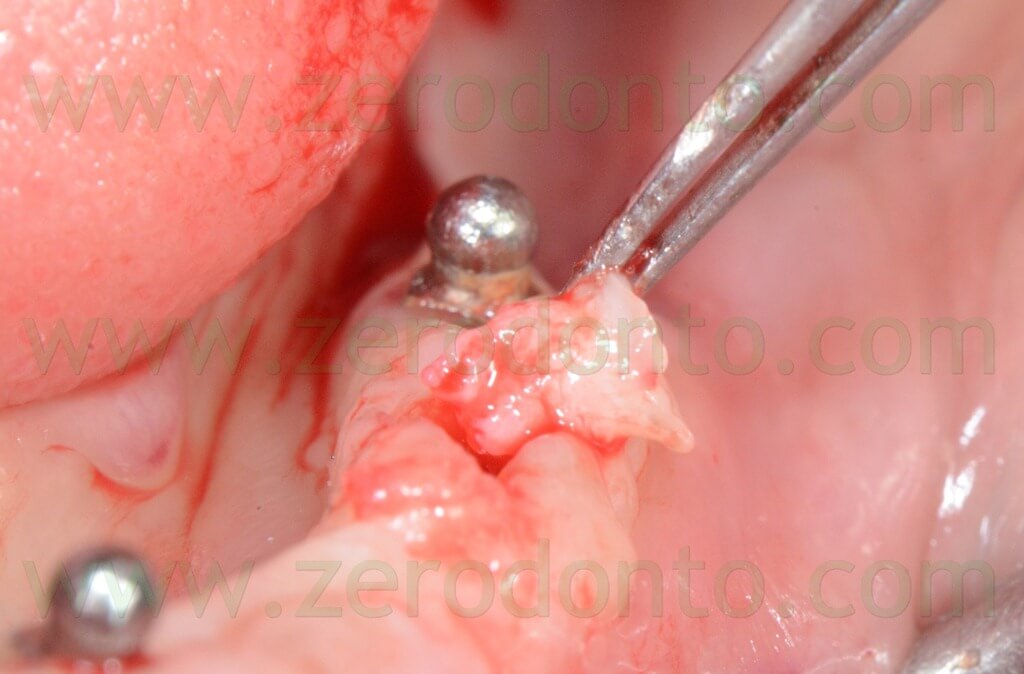
Differently from the mandibular surgery, where the fit between the prosthetic cylinders and the fixtures was slightly complex, a mucotome wider than the implant diameter was used, in order to ease the prosthetic procedures.
During surgery, particular attention was given to the placement of the guided handles, so as not to interfere with the position of the stabilization pins; differently, the surgical drills could have not reached the correct depth.




Implant primary stability was evaluated after removing the surgical template. Although a manual torque higher than 35 Ncm was evidenced on implants in region 14 and 16, their primary stability was unsatisfacory; in the authors’ opinion this was probably due to the friction exerted by the mounters on the sleeves.

















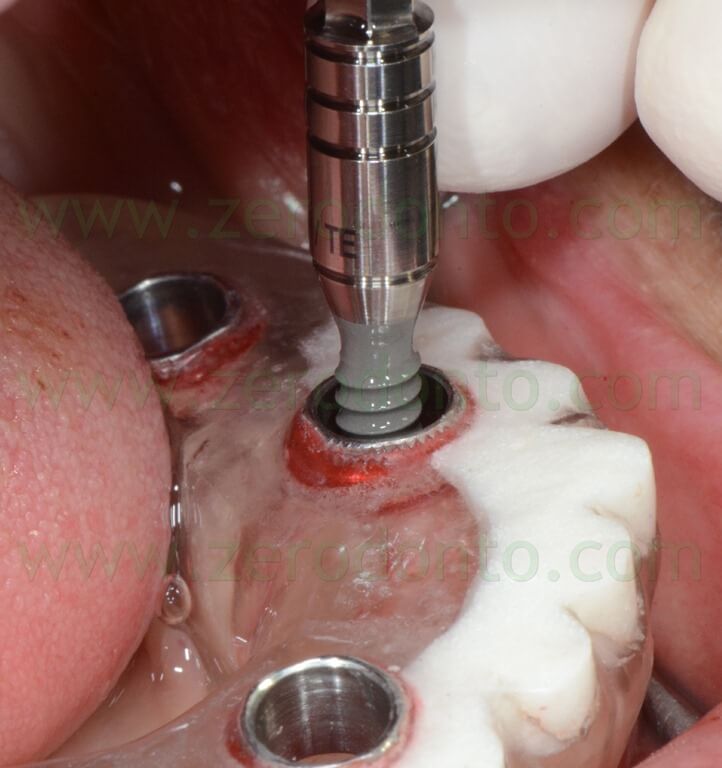
Consequently, the Roxolid SLActive implants planned in these areas were substituted with 2 Tapered Effect (TE) fixtures. After inserting half of these implants into the bone, the standard TE mounters were substituted with guided mounters; then, the surgical template was placed intraorally again from the top of these mounters and the implant placement was completed as previously described.
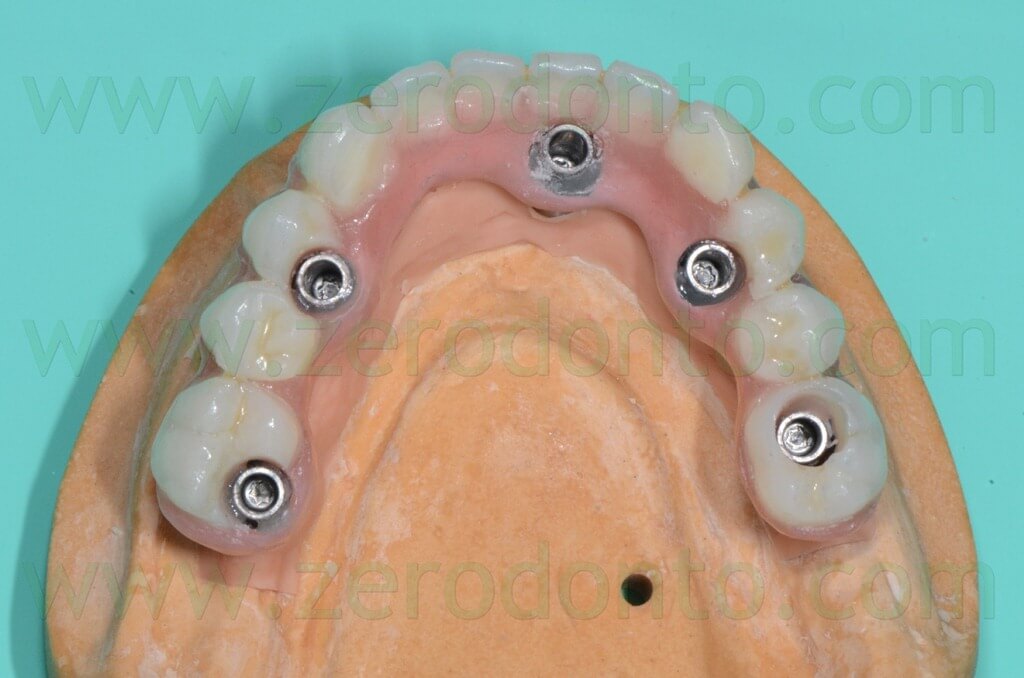
The prosthetic procedures were comparable to those reported for the mandibular arch. Due to its unsatisfactory primary stability, it was decided not to immediately load the implant in region 14; a cover screw was placed onto it and the immediately-loaded temporary full-arch prosthesis was consequently modified.
Differently from the mandibular arch, the prosthetic fit of the maxillary prosthesis was immediately optimal.


The biointegration of both prostheses as well as the mucosal transitions were completely satisfactory soon after surgery. Six months after the immediate loading, both function and esthetics were considered optimal by the clinicians and the patient.






The case was finalized by means of implant-supported zirconia-ceramic full-arch restorations at both arches.


CONCLUSIONS
The planning procedures using the Codiagnostix software were user-friendly and satisfactory.
Although it was not a standard protocol procedure, the planning of the stabilization pins at the maxillary arch was very complex. The three-dimensional placement of such pins, in fact, was negatively affected by the limited angular movements allowed by the Gonyx; consequently, the pins were planned with 45° angulation to the sagittal plane.
Since the Straumann guided surgery system is completely digital, it would be advisable to develop a digital system to transfer planning data from the clinician to the dental laboratory; a paper printed planning seems to be obsolete.
Although it was a precise mechanical device, the Gonyx was proved to be very operator-sensitive and a proper training is necessary to achieve optimal results.
Misfits and imprecisions could be introduced in the system during the manual match of the paper verification template onto the Gonyx platform.
Similarly, the use of magnetic metal spheres to fix such verification template could cause undesired micro-movements on the platform.
The verification system of the coronal-apical position of the sleeves should be improved as well: the deformation of a paper that is not provided and standardized by the system is a very operator-sensitive procedure and it cannot be controlled properly.
The Straumann guided-surgery procedures were proved to be valid and reliable, although it would be advisable to develop stabilization systems more effective than the solely bone/mucosal-supported templates. To date, the system is not provided with specific stabilization pins; temporary implants and bone screws can be considered more expensive and less user-friendly.
It is advisable to use mucotomes slightly wider than the implant diameter, so as to ease the fit between the prosthetic cylinders and the fixtures. Moreover, the friction exerted by the surgical template could negatively affect the operator’s manual sensitivity during implant placement. As a consequence, the real primary stability can be verified only after the removal of the surgical template.
From a prosthetic viewpoint, the system should be implemented with specific components for the immediate loading procedures. This would allow not to use new implant mounters to fabricate the temporary prosthesis, limiting the costs of the rehabilitation.
Although a proper training is necessary to optimize the outcomes, the clinical procedures were less time-consuming than a conventional approach. Moreover, the patient’s comfort in the post-surgical phases was very satisfactory.
In the authors’ opinion, the described system can be considered clinically effective, although the above mentioned improvements would be desirable. A proper multidisciplinary study of the case as well as a correct communication between the clinical and technical teams are paramount to achieve the clinical success.
The present case will be followed-up to validate the clinical effectiveness of the described system over time.
TWO YEARS CHECK




REFERENCES
1. Abboud M, Orentlicher G. An open system approach for surgical guide production. J Oral Maxillofac Surg. 2011 Dec;69(12):e519-24.
2. Dreiseidler T, Tandon D, Ritter L, Neugebauer J, Mischkowski RA, Scheer M, Zöller JE. Accuracy of a newly developed open-source system for dental implant planning. Int J Oral Maxillofac Implants. 2012 Jan-Feb;27(1):128-37.
3. Dreiseidler T, Neugebauer J, Ritter L, Lingohr T, Rothamel D, Mischkowski RA, Zöller JE. Accuracy of a newly developed integrated system for dental implant planning. Clin Oral Implants Res. 2009 Nov;20(11):1191-9. Epub 2009 Jul 20.
4. Behneke A, Burwinkel M, Behneke N. Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin Oral Implants Res. 2012 Apr;23(4):416-23. doi: 10.1111/j.1600-0501.2011.02337.x. Epub 2011 Oct 24.
5. Orentlicher G, Abboud M. Guided surgery for implant therapy. Oral Maxillofac Surg Clin North Am. 2011 May;23(2):239-56, v-vi.
ACKNOWLEDGEMENTS:
The authors would like to thank Mr. Marco Mutone for his support in the dental laboratory procedures.
INFO:
zerodonto@gmail.com

