The high success rate of prosthetic rehabilitation by means of osseointegrated implants both in partially and totally edentulous patients currently represents the proof of power of the rules related to the biological processes of osseointegration (Romeo E. et al., 2004). The presence of an adequate percentage of bone mass is critical, facilitating the three-dimensional positioning of the implant in order to guarantee a morphologically, functionally and aesthetically optimal healing of teeth.
To note that “this percentage of bone mass” (or bone quantity) must be in adequate relationship with the antagonist arch in order to achieve the aesthetic and functional rehabilitation and also to allow the physiological transmission of the forces along the long-axis of the implant.
The reduction of the functional eccentric loads may not influence the biological osseointegration process already performed (Isidor, 1996) and, moreover, it helps to reduce the forces and the level of stress that may be dangerous for the implant and/ or prosthetic components.
Edentulous crest bone dimensions require an adequate bone thickness in vestibular-lingual and palatal direction, able to facilitate the implant insertion in a suitable position for the future prosthesic rehabilitation, whereas around the implant a bone quantity of about 1mm on both sides must be maintained. In mesial-distal direction the edentulous space should allow the re-establishment of a correct interproximal space to achieve an efficient mechanical detersion.
It is well known that the mesial-distal dimensions among the contact points of the adjoining elements must be at least 7-8 mms in order to fix correctly implants having a prosthetic base of about 5mm, similar to the “standard” – Straumann implants. In order to proceed to the implant insertion of a “standard” length, a space of at least 8 mm must be available in the crown-apical approach. After the extraction of the tooth element, a 4-6 month wait period is necessary, to obtain a highly mineralized bone able to ensure a better implant stability (Chen et al., 2004; Cardaropoli et al., 2005) .
This waiting period represents an uneasiness for the patients who insistently ask to reduce the long waiting period leading to the prosthetic implant rehabilitation.
Although there are several factors influencing the entity of the post-extractive bone healing process (i.e. pathologies caused by the extraction, surgical trauma due to the extraction, bone biotype, gingival biotype, elapsed time, etc.), there is always evidence of bone remodelling, by a reabsorption of the vestibular- cortical bone (Cardaropoli et al., 2003) that can make more complex the future displacement of the implants.
According to Carlsson and Persson, six months after the tooth extraction, a bone reabsorption equal to the 23% of the residual crest average can be observed, increasing by a further 11% after two years.
In order to reduce the long treatment periods and avoid or diminish the post-extractive bone re-absorption, clinicians use implants rapidly inserted in the post-extractive alveoli during tooth extraction (immediate post-extractive implants), or immediately after soft tissue healing (delayed post-extractive implants).
However, in the past there has been reported a high percentage of failures, especially due to the insertion of cylindrical or smooth surface titanium implants, the use of non-absorbing membranes(often exposed to the oral cavity during their displacement), the poor knowledge on bone healing biology and the approximated surgical techniques, especially in case of immediate-loading post-extractive implants (Gher et al., 1994).
Nowadays, the use of rough surface implants (more osteofilic) with a trunk-conic shape to facilitate space reduction between the alveolar bone walls, the use of reabsorbing membranes and more sophisticated surgical techniques employed and more importantly, better scientific knowledge acquired about the bone healing process have helped to increase the average percentage of success, that is over 92-93% (Chen et al., 2004).
Today implants inserted inside the natural alveoli are defined post-extractive. They are distinguished in two types: immediate or type I (characterized by the implant insertion inside the natural alveolus immediately after the tooth extraction that is seen as part of the surgical act), and delayed or type II (characterized by the implant insertion inside the natural alveolus, 4-8 weeks after the extraction, following soft tissue healing).
Both these methods allow to use the reparative regeneration properties of the bone tissues thanks to the presence of a big quantity of growth factors in the alveolus influencing the site neovascularisation and bone cell proliferation.
The advantages of the immediate implant loading in the post-extractive alveolus are related to the reduction of the number of surgeries and the treatment period length. The disadvantages are related to the site morphology that could not be optimal for the loading and the stability of the implant, or because of cheratinization of the mucosa that could be inadequate for an optimal adaptation to the edge especially in case of a thin gingival biotype.
The delayed post-extractive implant has the advantage to have bigger quantity and volume of mucosal tissue (this makes simpler the “management” of the soft tissues) and it can be displaced in the healthy alveolus, whereas disadvantages consist in the long period of treatment (4-8 weeks) and also any possible premature reabsorption of the bone walls could make more complex the morphology of the post-extractive site.
At this point it must be specified that clinical studies regarding bone restoration show that if there is a small space (<>mm or the insertion of the post-extractive implant is associated to the presence of a reabsorption of one or more alveolar walls, then it is required to effect additional procedures for the bone restoration through the use of membranes and bone grafts (Hämmerle et al., 2004).
In both cases, it should be noted that these are very delicate methods due to difficulties in controlling different parameters taking part in the process of the bone and perimplantar mucosal tissue healing.
Till today, the post-extractive implants have been used particularly in substitution of monoradicular or biradicular teeth. Therefore, these implants are most commonly employed in the anterior areas of the oral cavity as the patients want to reduce the long treatment period especially when is involved an aesthetic area. Furthermore, the clinicians operate easily in these sites of the mouth: the access is simple, the possibility to insert the implants in optimal positions in terms of prosthetic point of view is optimal and it can be achieved a good primary stability with the result of small gap between the bone and the implant.
In posterior areas, the use of these post-extractive techniques is avoided due to the lower aesthetic demands and the presence of greater bone volume. Differently to the frontal areas, any possible post-extractive implant insertion made in the molar areas require the use of inter radicular septa (often very small) for the anchorage and in order to achieve enough stability of the implant. As a result there is a big gap between the bone walls and the implant.
In case of insertion of the implants in the mesial-distal alveoli in order to apply premolar-shaped prosthetic crowns, the nearness between them and the dental roots can often represent a local contraindication for the insertion of post-extractive implants in the alveoli. In fact, it is not possible to guarantee enough space for the detersion of the approximal surfaces of the prosthetic crowns.
The following clinical case shows a prosthetic implant rehabilitation performed through 2 delayed post-extractive implants displaced to the same level of the mesial-distal roots of a molar pulled out six weeks before.
CLINICAL CASE
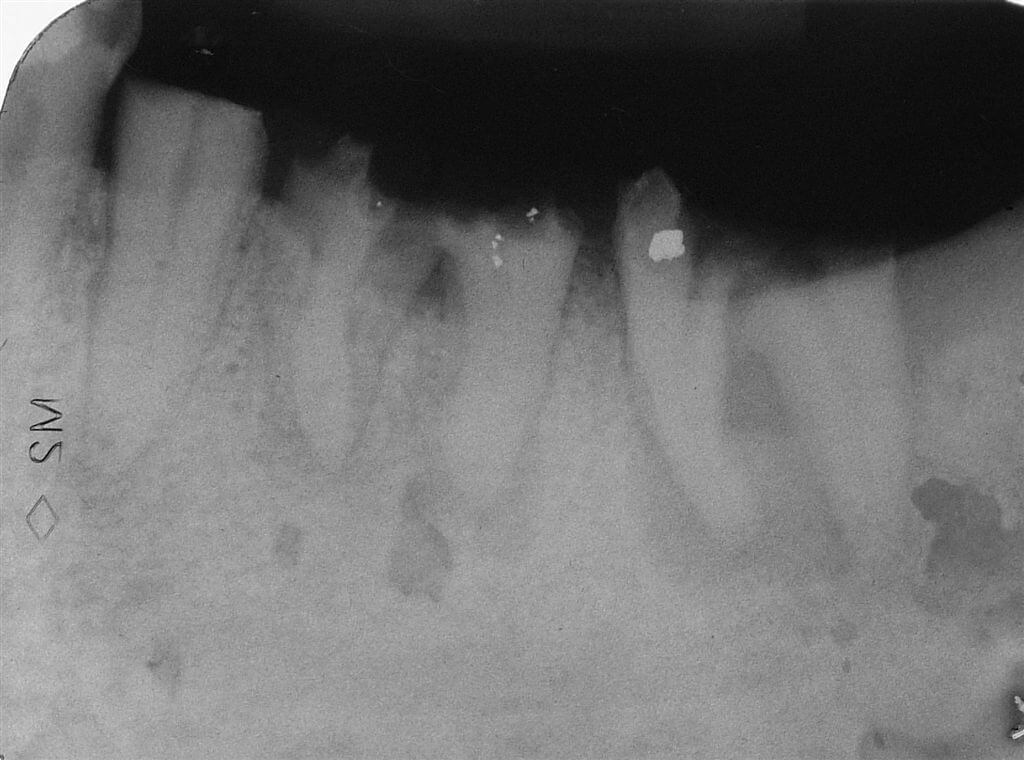
A 51 year-old male patient, non smoker had the molars 36 and 37 irremediably damaged for dental decay process. (Fig.1)
The high rate of functional deficit became aggravated for the loss of the 35 clinical crown. Therefore the patient wished to restore as soon as possible a satisfactory masticatory function through a rehabilitation achieved with fixed prostheses. The lack of 27 to the antagonist arch and the presence of an interradicular septum of a big dimension due to the excessive divarication of the 36 roots allowed us to plan the orthodontic and prosthetic recovery of 35 and the insertion of two delayed post-extractive implants in the alveoli of 36 for the realization of two premolar shaped prosthetic crowns.
After the delicate extraction of 36 and 37 and the revision of the post extractive alveoli, it had been necessary to wait for 6 weeks to obtain an optimal recovery of the soft tissues (Fig.2).

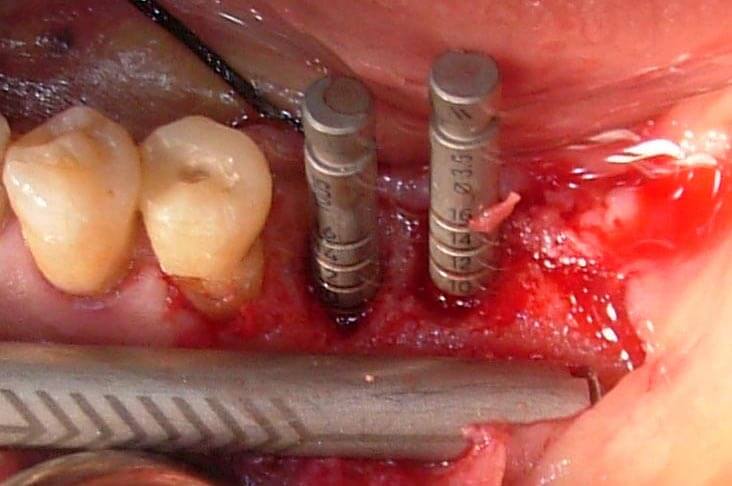
Then, we proceeded with the surgery for the positioning of two Straumann implants in the alveoli of the mesial-distal roots of 36.
The incision was made in the crest, in the centre of the keratinized mucosa through a Bard Parker n°12b scalpel (lancet) and then the ungluing of the total edge thickness was performed (Fig. 3).

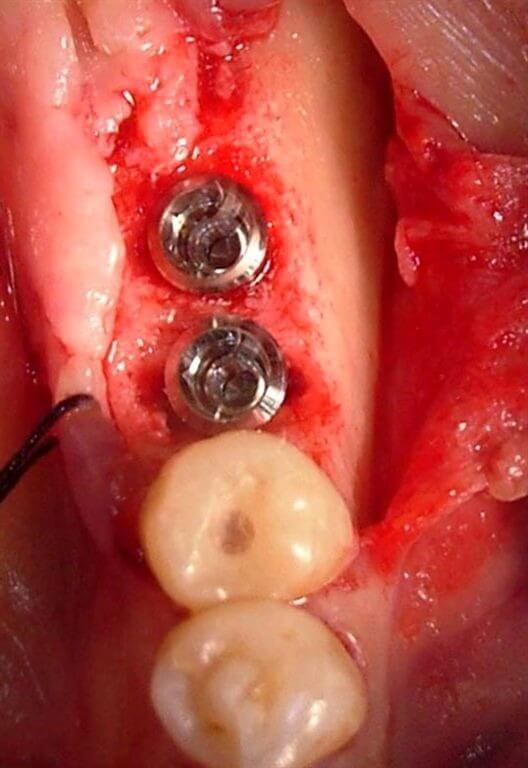
After having performed vestibularly and lingually some divaricable sutures, the granulation tissue was removed on both alveoli using small and sharp Lucas alveolar spoons (Fig. 4)
 We proceeded to the regularization of the bone crest through the use of a manual device (Micross® Meta) to achieve autogenous cortical bone. Afterwards, a further bone sample was achieved through the same device, from the external oblique line, in order to have enough autologous bone quantity to fill the gaps around the implants (Fig. 5).
We proceeded to the regularization of the bone crest through the use of a manual device (Micross® Meta) to achieve autogenous cortical bone. Afterwards, a further bone sample was achieved through the same device, from the external oblique line, in order to have enough autologous bone quantity to fill the gaps around the implants (Fig. 5).
It is quite always possible with these very small devices to remove big quantities of autologous bone apically to the site of the implant insertion and in distal inferior areas (Fig.6)

In order to obtain prosthetically driven implant displacement and to achieve a correct interplanar distance, the preparation of the implant site displaced in the mesial root has been slightly mesialized, whereas the distal root has been distalized; this was made been possible for the lack of the seventh. In the mesial alveolus was displaced a Straumann micro-screw implant of 4.1mm diameter and 8 mm length with ta standard transmucosal component as the dimensions of post-extractive alveolus wew small in comparison with the dimension of the implant body. In the distal alveolus has been positioned a type implant ITI TE Ø 4.1-4.8 of 8 mm length. The TE implant allows to obtain a better primary stability and, thanks its trunk-conic shape, reduces the ampleness of the gaps between the bone and the implantar surface (Fig. 7).
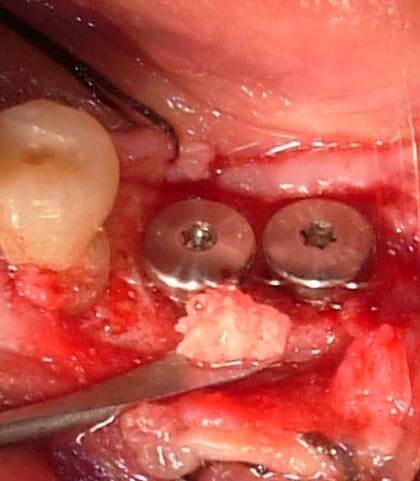
The small gaps around the inserted post extractive implants have been filled with the autogenous bone that has been removed through the Micross® Meta (Fig. 8);
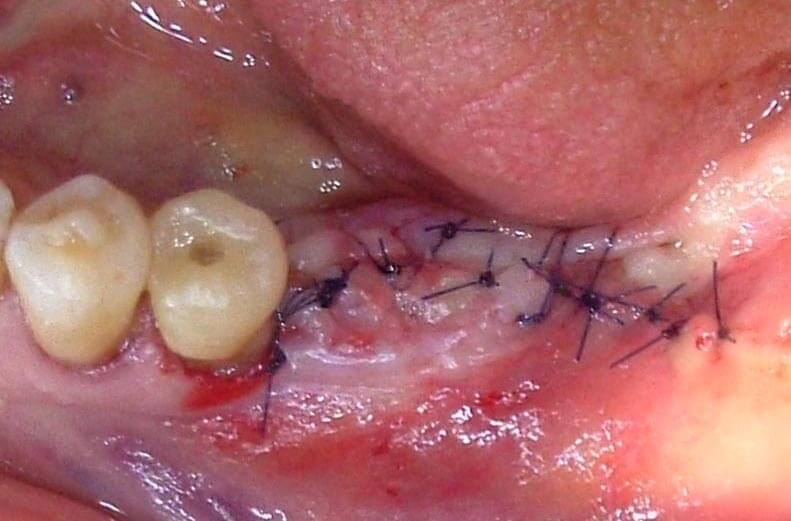
at the end, the edge suture was made (Fig. 9).
Antibiotic treatment has been prescribed to the patient (amoxicillin 1 g, 2/ die x 5 die), anti-inflammatory drugs (nimesulide 100mg, 2/die x 3die) and rinse with chlorhexidine 0.2% for 4 weeks.
After 3 months from the intervention we proceeded to obtain an imprint for the prosthetization of the implants and of the 35 (Fig. 10).

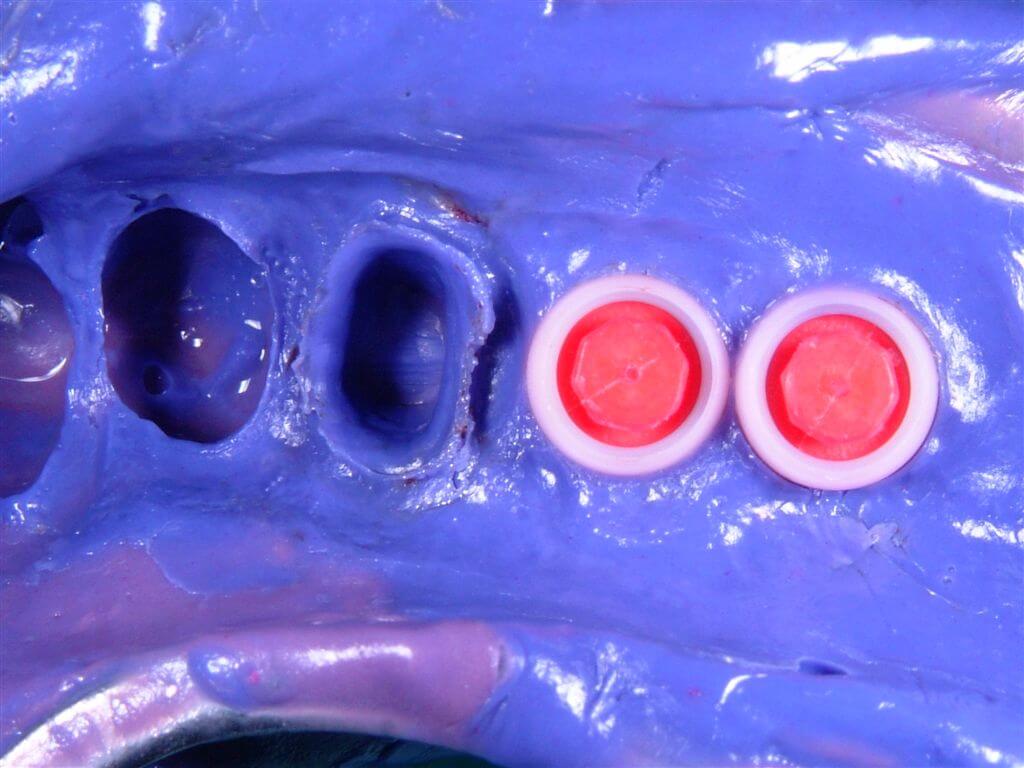
On the implants appropriate transfers have been installed (Fig.11) and a stamp has been taken with the use of polyethers (Fig 12).

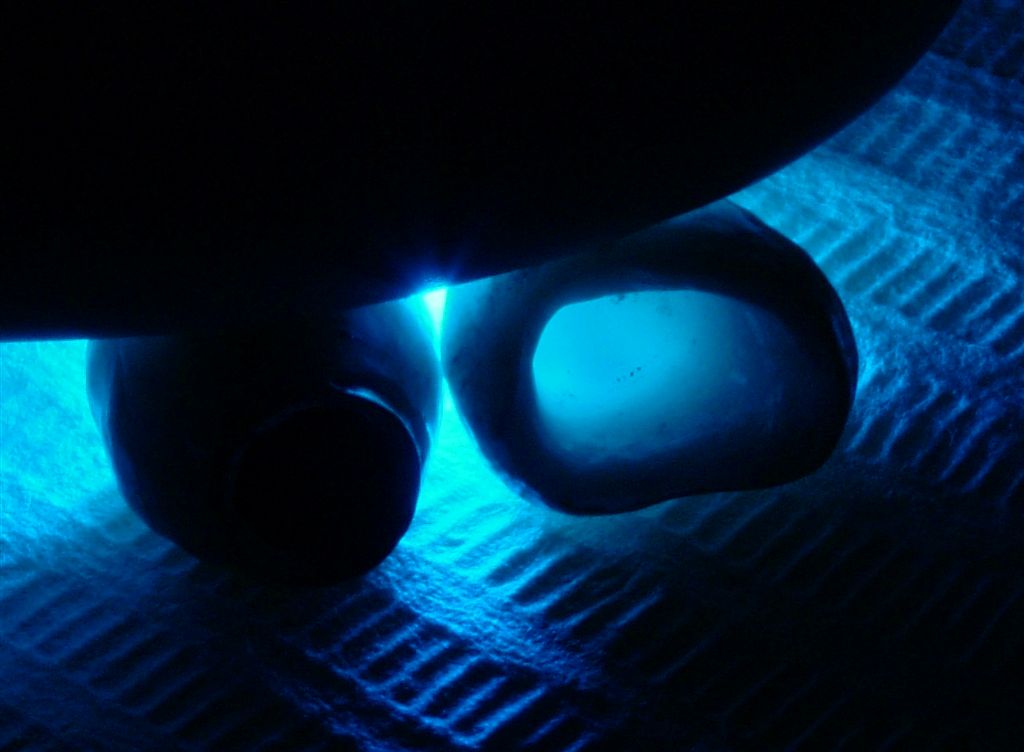
The prosthetic stumps selected for the implants were 5.5 mm synOcta type (Fig. 13) to support gold ceramic crowns, while the 35 dental element, previously prepared, has been prosthetized through integral ceramic crown type strong Procera, which, thanks to its transparency and translightnesst assured us an optimal aesthetical and functional result (Fig. 14-15-16).



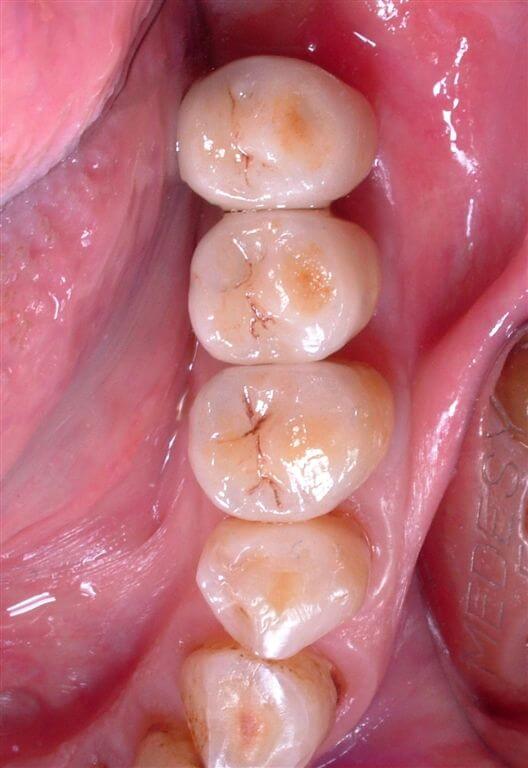
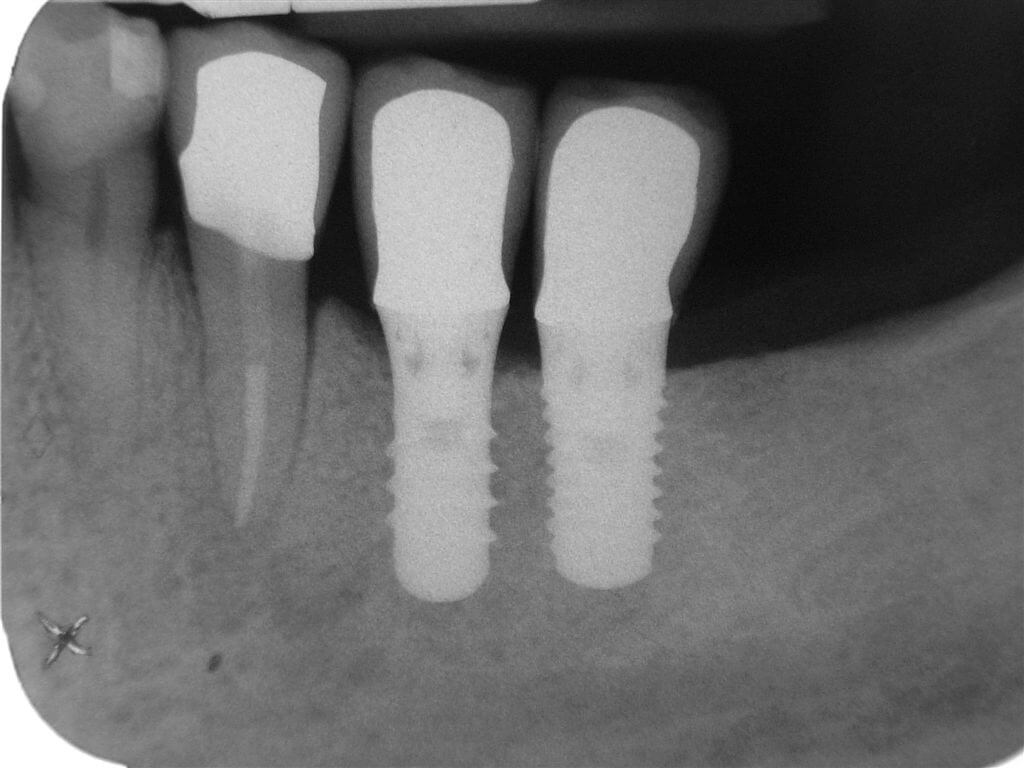
Six months after the prosthetization, clinical and radiographic control showed good response of soft and bone tissue both on functional challenge and clinicla and radiographic examination (Fig.17-18-19).

BIBLIOGRAPHY
1) Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G.Long-term survival and success of oral implants in the treatment of full and partial arches: a 7-year prospective study with the ITI dental implant system. Int J Oral Maxillofac Implants. 2004 Mar-Apr;19(2):247-59
2) Isidor F. Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys. Clin Oral Implants Res. 1996 Jun;7(2):143-52.
3) Chen ST, Wilson TG Jr, Hammerle CH.Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19 Suppl:12-25. Review.
4) Cardaropoli G, Araujo M, Hayacibara R, Sukekava F, Lindhe J.Healing of extraction sockets and surgically produced – augmented and non-augmented – defects in the alveolar ridge. An experimental study in the dog. J Clin Periodontol. 2005 May;32(5):435-40.
5) Cardaropoli G, Araujo M, Lindhe J.Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs.J Clin Periodontol. 2003 Sep;30(9):809-18.
6) Carlsson GE, Persson G.Morphologic changes of the mandible after extraction and wearing of dentures. A longitudinal, clinical, and x-ray cephalometric study covering 5 years. Odontol Revy. 1967;18(1):27-54.
7) Ghier ME, Quintero G, Assad D, Monaco E, Richardson AC.Bone grafting and guided bone regeneration for immediate dental implants in humans.J Periodontol. 1994 Sep;65(9):881-91.
8) Chen ST, Wilson TG Jr, Hammerle CH.Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes.Int J Oral Maxillofac Implants. 2004;19 Suppl:12-25. Review
9) Hammerle CH, Chen ST, Wilson TG Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets.Int J Oral Maxillofac Implants. 2004;19 Suppl:26-8. Review
FIGURE LEGENDS
Fig.1 The endoral radiograph shows lesions of 35, 36 and 37.
Fig.2 Rx after the avulsion of 36 and 37.We proceeded with the endodontic treatment of 35.
Fig.3 Incision in the centre of the keratinized mucous.
Fig.4 Occlusal vision of the alveoli after the granulation tissue removal.
Fig.5 Autologous bone removed from the external oblique line through the use of a manual device of cortical bone removal (Micross® Meta).
Fig.6 A sample of autologous bone taken.
Fig.7 Occlusal vision of the inserted implants. To note the presence of a “gap” of about 2 mms around the implants.
Fig.8 Autologous bone displaced around the implants for filling the gaps.
Fig.9 Suture.
Fig.10 Occlusal vision when the imprint has been taken.
Fig.11 The imprint has been taken through imprint transfers and the red positioning cylinders synOcta.
Fig.12 Details of the polyesthers stamp.
Fig.13 SynOcta stump of 5.5 mms displaced on the implants.
Fig.14 Test of the structures. A structure in zirconium has been realized on 35 allowing us to obtain a high aesthetic quality golden league used in the implants.
Fig.15 Translucentness of the zirconium in comparison to the traditional materials can be noticed with the aid of a light source of substantive intensity.
Fig.16 Internal aspect of the gold-ceramic and zirconium-ceramic crowns.
Fig.17 Occlusal vision of the final elements 6 months after prosthetization.
Fig.18 After six months vestibular vision of the crowns.
Fig.19 Rx review after 6 months.
For further information:
zerodonto@gmail.com

