A 71 yo male patient, non smoker and sistemically healthy required a fixed implant-supported rehabilitation in the posterior left mandible.
Teeth in position 3.5-3.7 were extracted 6 months before the screening visit and a socket preservation procedure was performed.
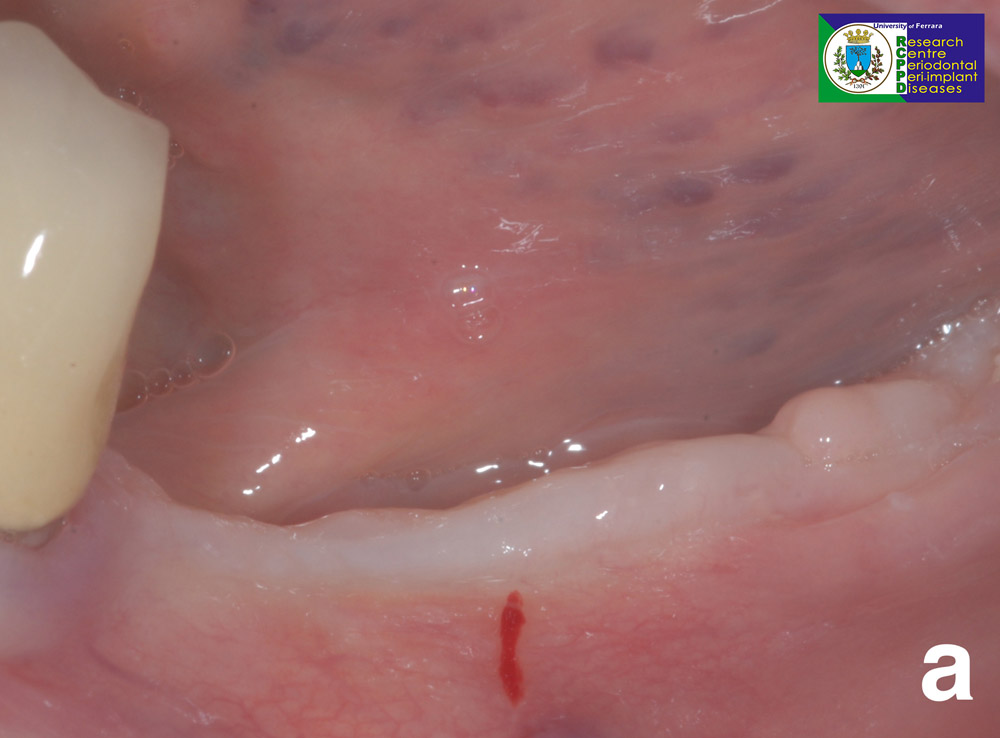
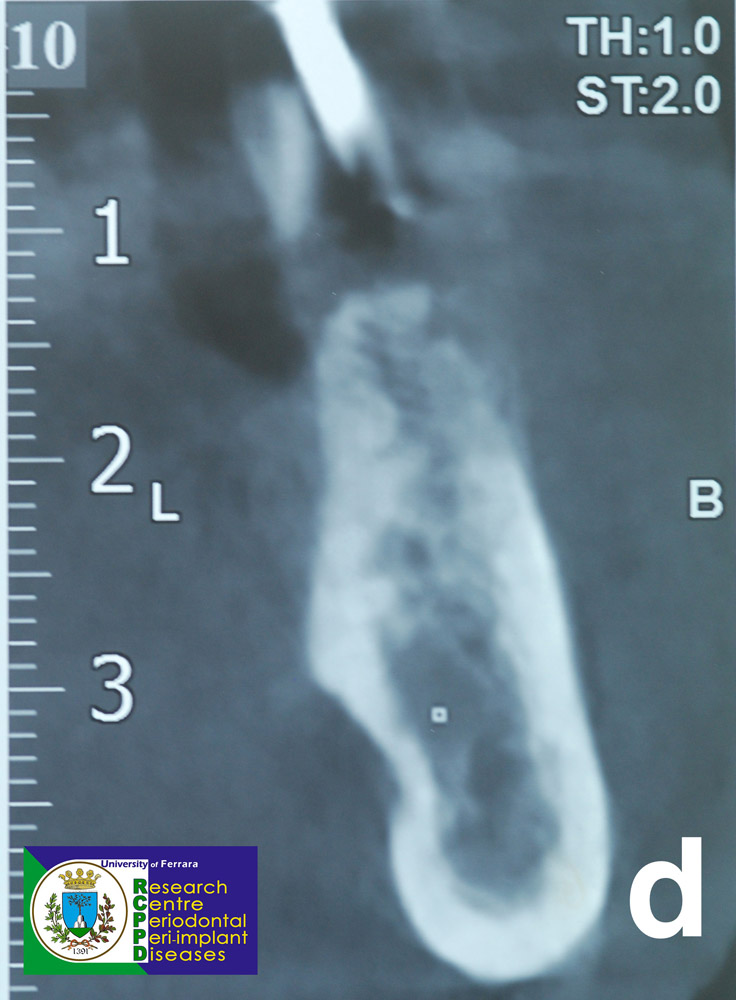
Clinical and CBCT evaluation revealed a thin bucco-lingual dimension of the bone ridge, insufficient to place implants in a prosthetically driven position.

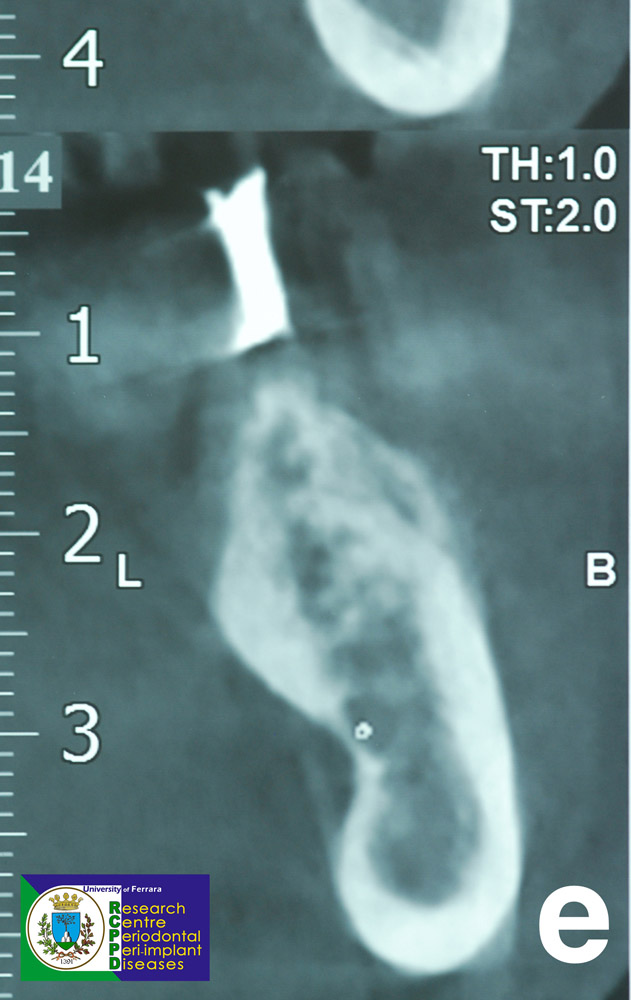
Treatment plan required the placement of 3 implants in position 3.5-3.6-3.7 by mean of the Sub Periosteal Peri-Implant Augmented Layer (SPAL) technique to simultaneously augment the thickness of the buccal bone plate at the time of implant in position 3.5 – 3.6.
A split-thickness, crestal incision was performed in the region 3.5-3.7. A vertical releasing incision was made distal to 3.4.
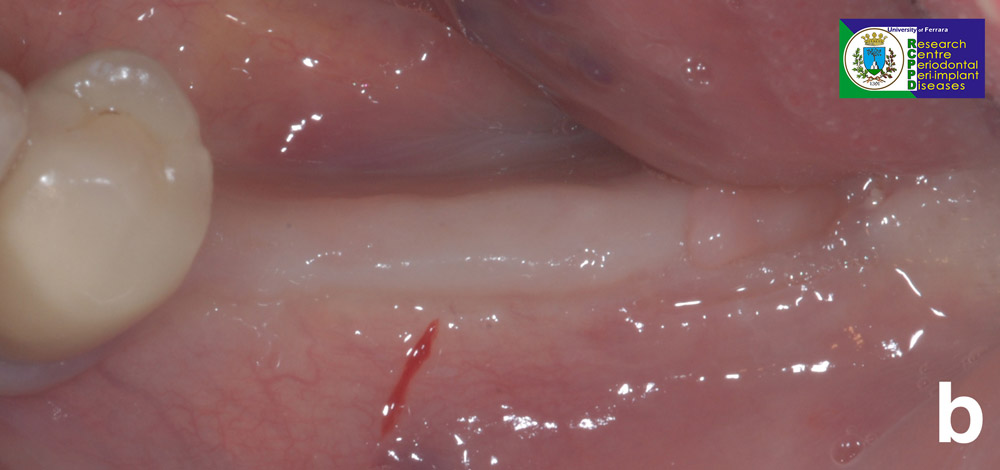
A split thickness flap was then raised using a 15C blade thus creating two distinct layers. A external tension free layer, namely the mucosal layer, and an internal layer attached to the bone ridge, namely the periostal layer. A full thickness flap was elevated on the lingual aspect.
Periosteal layer was then detached from the bone ridge by mean of a crestal incision reaching the bone and using microsurgical periosteal elevator (PTROM, Hu Friedy, Chicago, Illinois) and tunnelling knives (KPAX- TKN1X- TKN2X, Hu Friedy, Chicago, Illinois), taking care not to damage its integrity. In this way, a pouch was created between the bone ridge and the periosteal layer.
3 tissue-level implant (Thommen Medical, Grenchen, Switzerland) in position 3.5-3.6-3.7 were placed. Implant in position 3.5 presented a buccal dehiscence while implants in position 3.6 presented an intact but thin (< 1 mm) buccal cortical bone plate.
The space between the periosteal layer and the exposed implant surface/buccal cortical bone plate was filled with a bovine derived xenograft (Bio-Oss® spongiosa granules, diameter 0.25-1.0 mm; Geistlich Pharma, AG, Wolhusen, Switzerland) to completely correct the buccal dehiscence and simultaneously augment the thickness of the buccal cortical bone plate. The graft was performed even at the 3.7 region to improve the “space-making” effect.
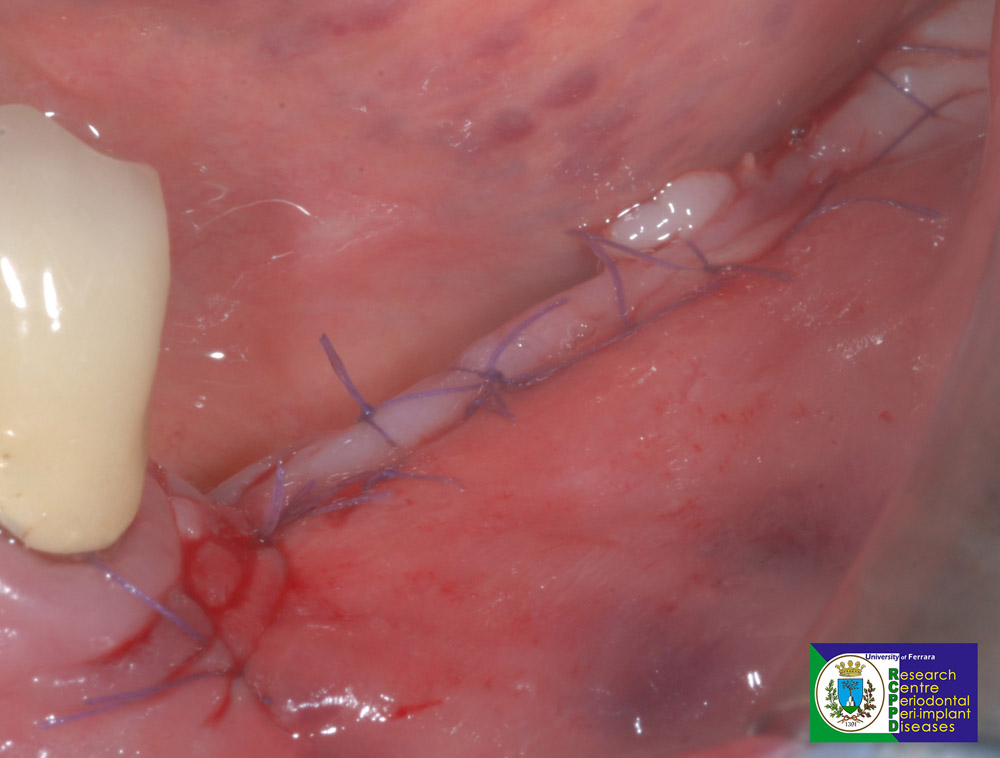
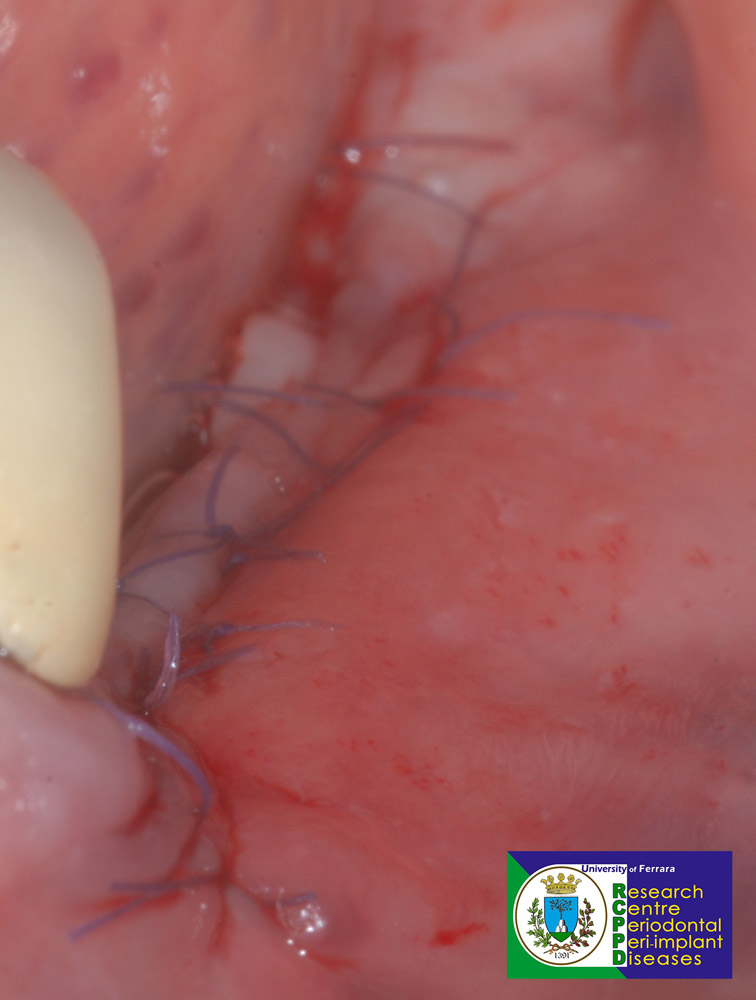
Periosteal layer was then sutured tension-free to the lingual flap by mean of 6/0 internal mattress sutures to stabilize the xenograft. Finally, implants, graft and periosteal layer were submerged by coronally advancing the mucosal layer and suturing it to the lingual flap by mean of 6/0 internal mattress and interrupted sutures.
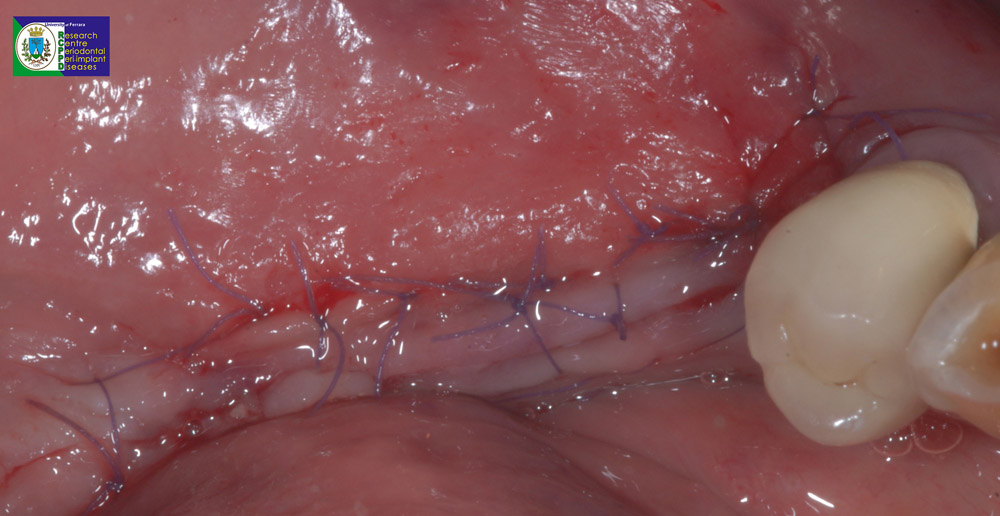
Home use of a 0.12% chlorhexidine solution (Curasept ADS Trattamento Rigenerante®; Curaden Healthcare, Saronno, Italy) was prescribed for chemical plaque control (1-minute rinse b.i.d. for 3 weeks). Painkiller/anti-inflammatory therapy was self-adminestered as needed. Sutures were removed at 2-weeks post-surgery
Implant exposure was performed 4 months after implant placement. A partial thickness flap was detatched in region 3.5-3.6. No implant presented buccal dehiscence and every implant presented a thick (≥ 2 mm) buccal cortical bone plate. Healing abutments were placed. A free gingival graft at implants in position 3.5-3.6 was performed to improve dimensions of peri-implant keratinized mucosa.
Peri-implant tissues are stable 6 months after the insertion of the final prosthesis.


SPAL technique could be considered a valuable simplified surgical approach for horizontal bone augmentation and to correct peri-implant bone dehiscences.

