Edentulism was defined as a pathological condition by the World Health Organization in 1990. The discomfort and inconvenience that this condition can generate in terms of aesthetics, function, as well as psychologically, can be so debilitating as to consider edentulism a social handicap.
Due to the gradual increase in the average age of the population, today there are more and more people in their seventies who are enjoying overall good health and intrapersonal relationships. Their expectations have significantly increased as well, and as patients are no longer satisfied with traditional removable dentures; explicit requests are now frequently made for fixed prosthetic solutions with a high level of aesthetics and correct function.
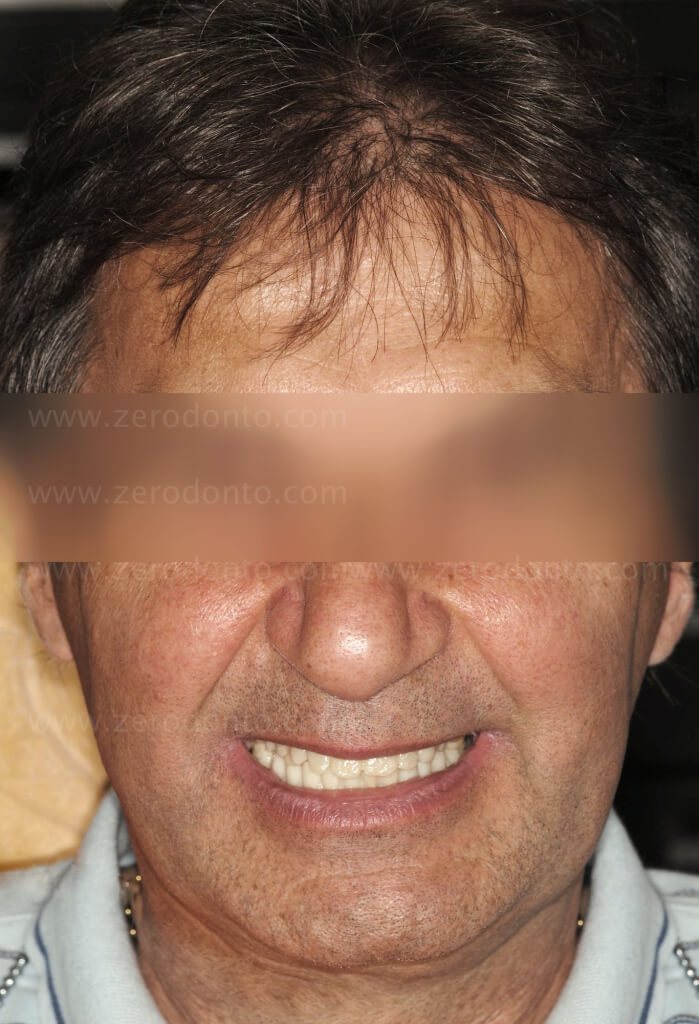
One such example is this patient who came to our observation in 2009 complaining of severe discomfort from a functional and aesthetic perspective (Fig. 1). His dentures were worn and unstable, causing frequent lacerations and sores on the gingival tissues and oral mucosa. The patient reported that this condition was causing psychological problems and lowering his self-esteem, therefore his desire was to solve this complex situation , if possible, with a fixed prosthesis. The assessment of the patient’s systemic risk profile pointed out that his general health conditions were good and that he would classify as ASA class I (Owens et al. 1978).
The evaluation of local risk factors showed the presence of few dental elements (that were in fact compromised) and a particularly marked atrophy of both the upper and lower jaw. The severe bone deficit could have been related also to infrequent readjustment of the prosthesis.
Fig. 1. Photographs taken during the patient’s first visit










Based on these assessments, as well as a panoramic and a lateral-latero cephalometric x-ray (Fig. 2), a thorough diagnosis was effected during the patient’s first visit and a hypothesis of an implant-prosthetic rehabilitation, taking into consideration costs and chair time , was formulated
Fig. 2. Initial Radiographs


The proposal consisted of:
- extraction of elements that were compromised and/or had no strategic value;
- new dentures to correct the vertical dimension, which was severely altered;
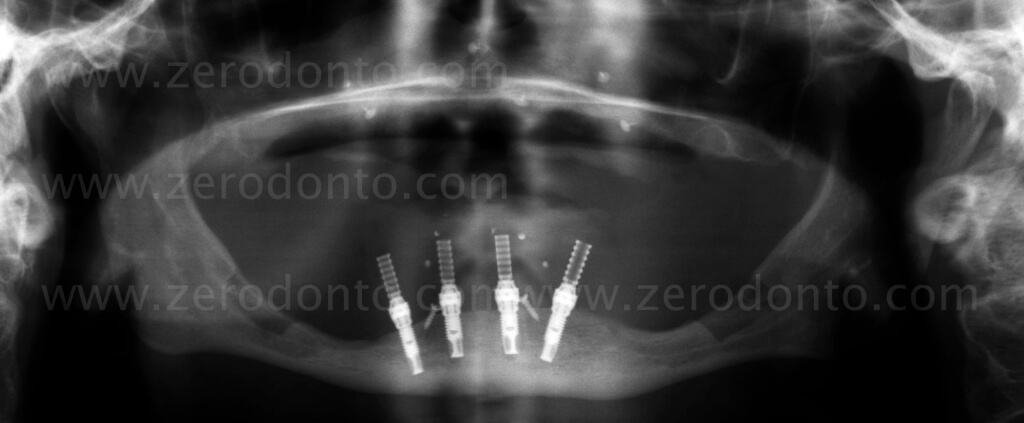
- the insertion of four implants in the lower jaw in the interforaminal region (All-on- 4 ™ technique ) (Maló et al. 2003, 2005, Patzelt et al. 2013) . Given the specific request of the patient to have a fixed prosthesis, this appeared to be the most appropriate solution.
Two solutions were proposed for the upper jaw:
- replace the temporary removable denture with a final removable denture;
- proceed with a fixed prosthesis anchored on implants.
The latter proposal opened up other possible treatment options, both surgical and prosthetic .
The surgical proposal was:
- bone reconstruction harvesting autologous bone from extraoral sites (mainly from the iliac crest), following the onlay or inlay technique;
- bone reconstruction harvesting autogenous bone from intraoral sites;
- insertion of zygomatic implants.
After a meticulous evaluation of the advantages and disadvantages, the financial costs and the time necessary for treatment of each of the possible hypotheses, and, in accordance with the patient, the following treatment plan was chosen: implant supported fixed prosthesis on both the upper and lower jaw. The dentures were manufactured with an acrylic resin coating in order to contain costs. This solution provided for the reconstruction of the upper maxilla with guided bone regeneration (GBR), applying the Fence Technique (Merli et al. 2013).
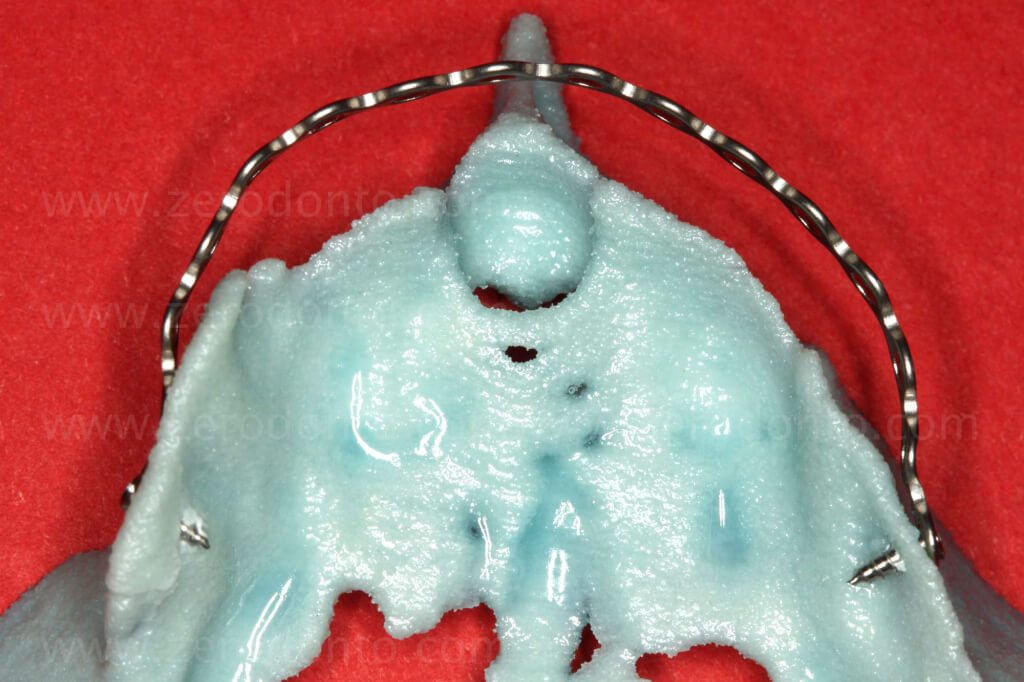
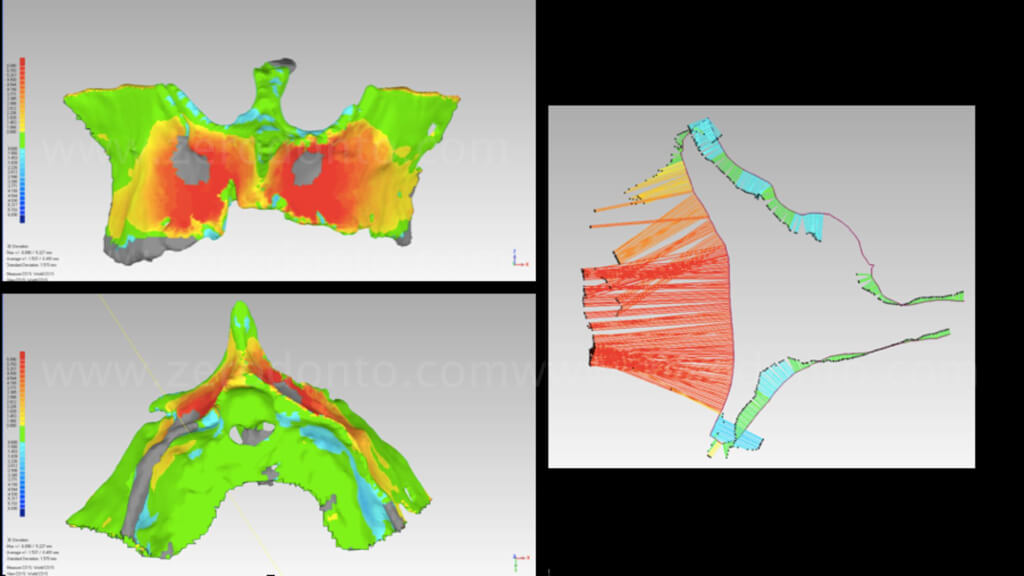
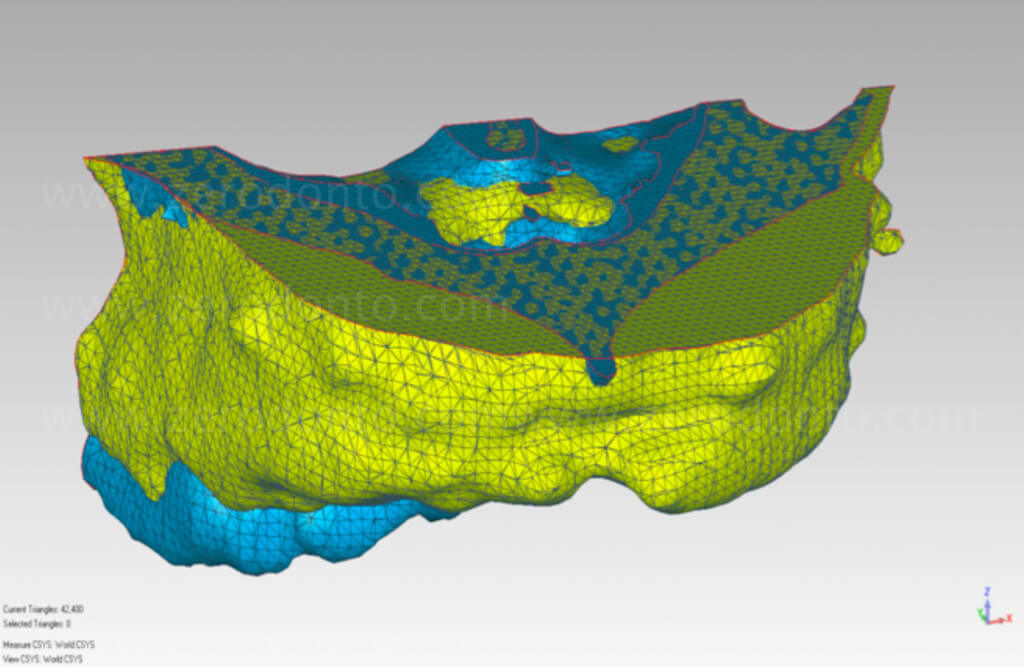
An aesthetic-functional balance was achieved with the realization of post-extraction full prostheses (Fig. 3). Radiopaque reference points were applied on the upper and lower prostheses, so as to perform a double scan computed tomography (CBCT), allowing for a virtual simulation of the surgical procedure. In addition, anatomical stereolithographic models were required for pre-surgical planning of the intraoral bone harvesting and the Fence Technique procedure (Fig. 4).

Fig. 3. Reorganization based on the post-extraction full prostheses
Fig. 4. Bimaxillary Rehabilitation: assessment of stereolithographic models


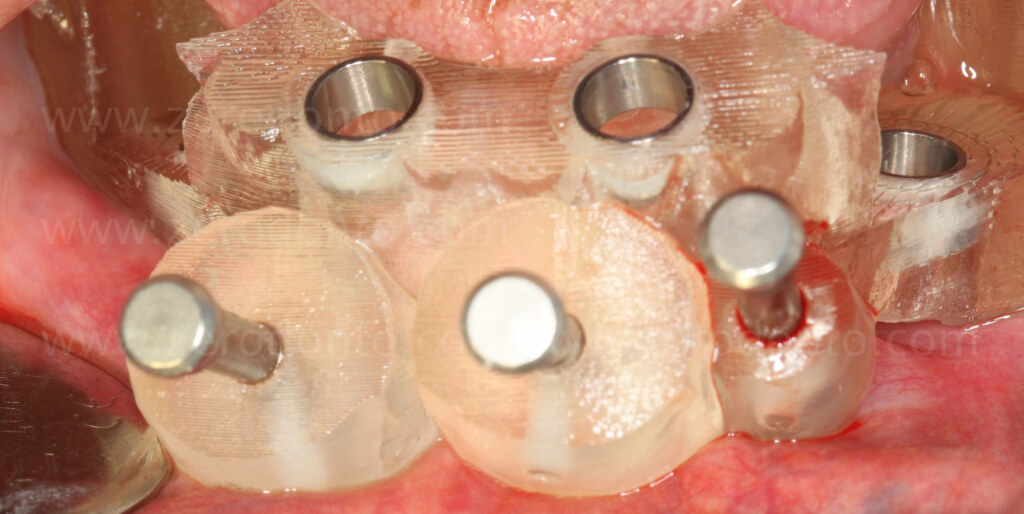
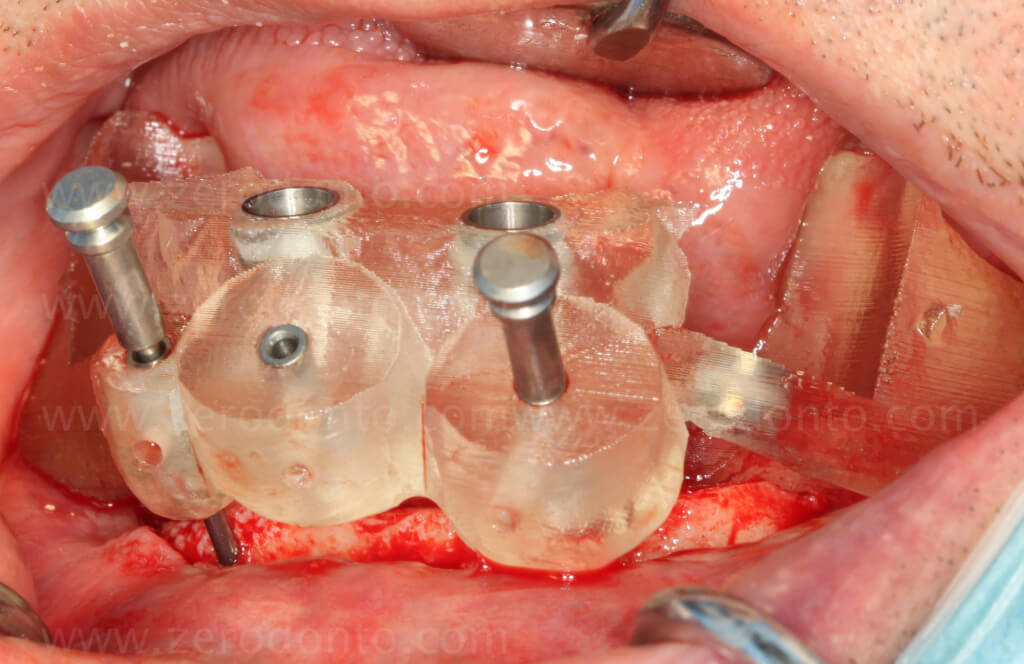
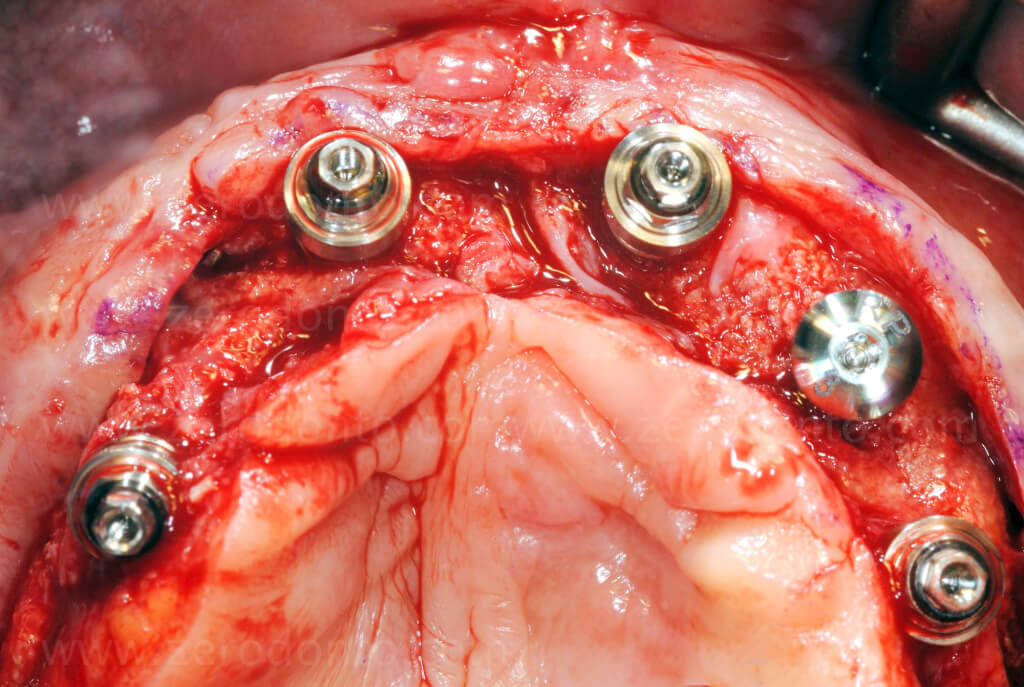
On the basis of the virtual planning, a specific surgical guide was requested. It should be noted that the manufacturer’s operating protocols were only followed in part. In fact, the presence of a significant discrepancy of the residual bone crest required bone leveling prior to implant insertion. Subsequently, the surgical guide was stabilized by means of specific anchor pins in order to memorize the correct position planned. At this point, the original operational protocol, which calls for a flapless technique, was modified. The guide was removed and a mucoperiosteal flap was raised to gain access to the underlying irregular bone structure. An osteotomy was effected to obtain a uniform platform of the residual crest on which the surgical guide was once again positioned using the previously drilled pinholes. The osteotomic implant insertion procedure was then performed.
Although the virtually planned insertion axis of the implant was respected, the vertical position of the final implant platform was decided directly during surgery without the aid of the surgical guide, as a direct result of the modification of the protocol described above.
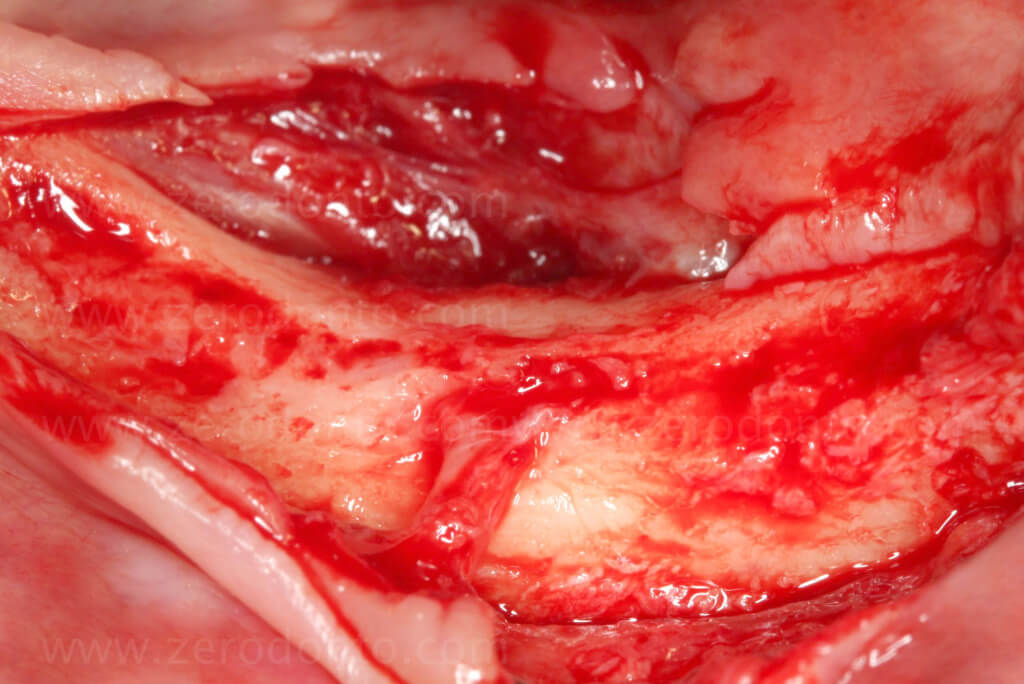
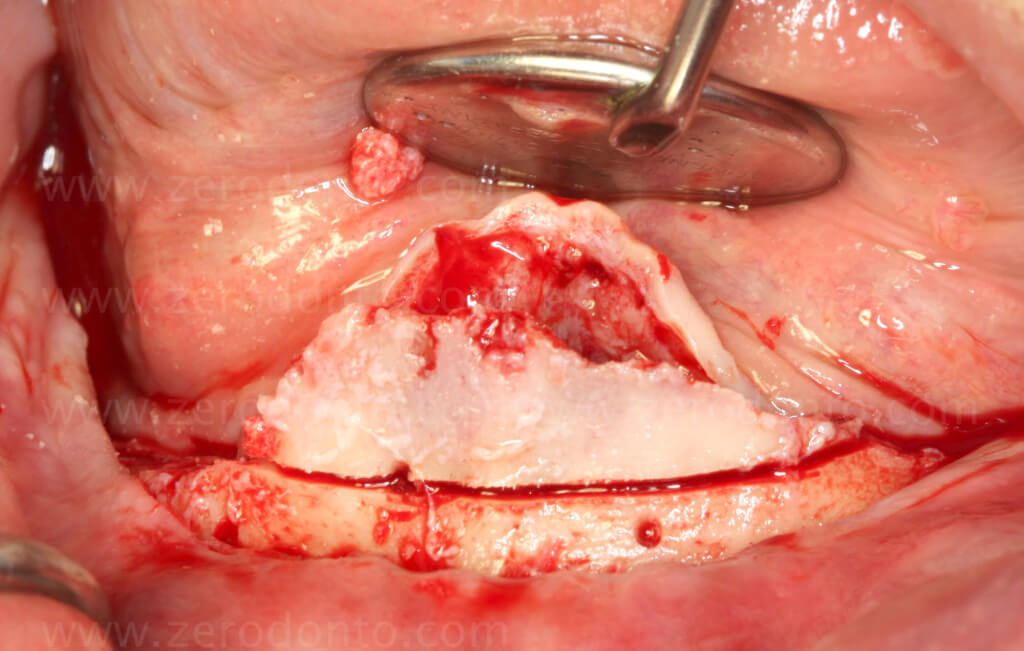
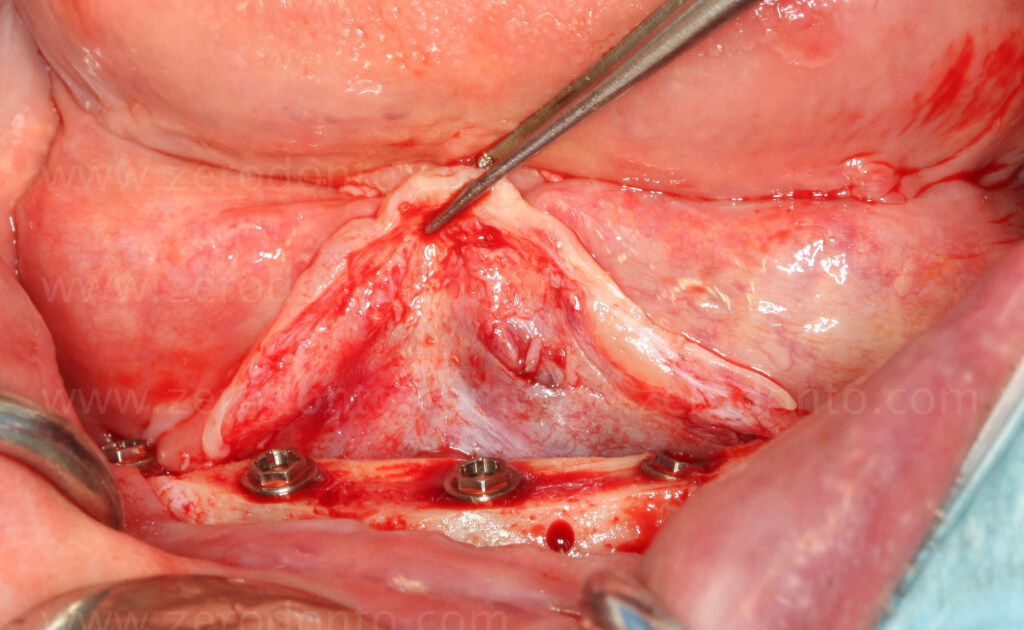
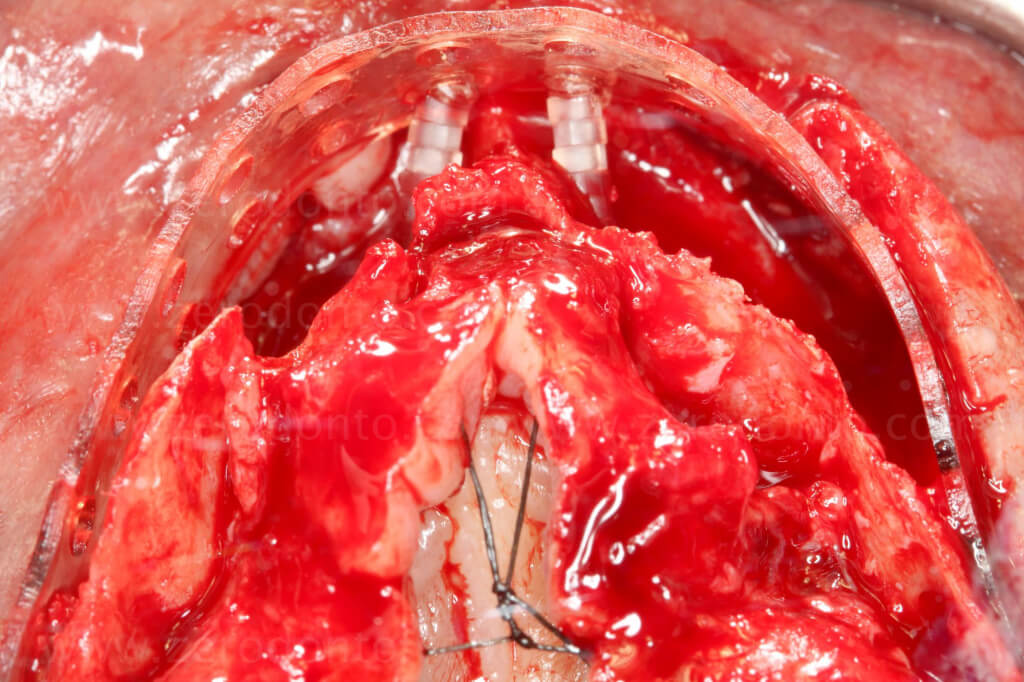
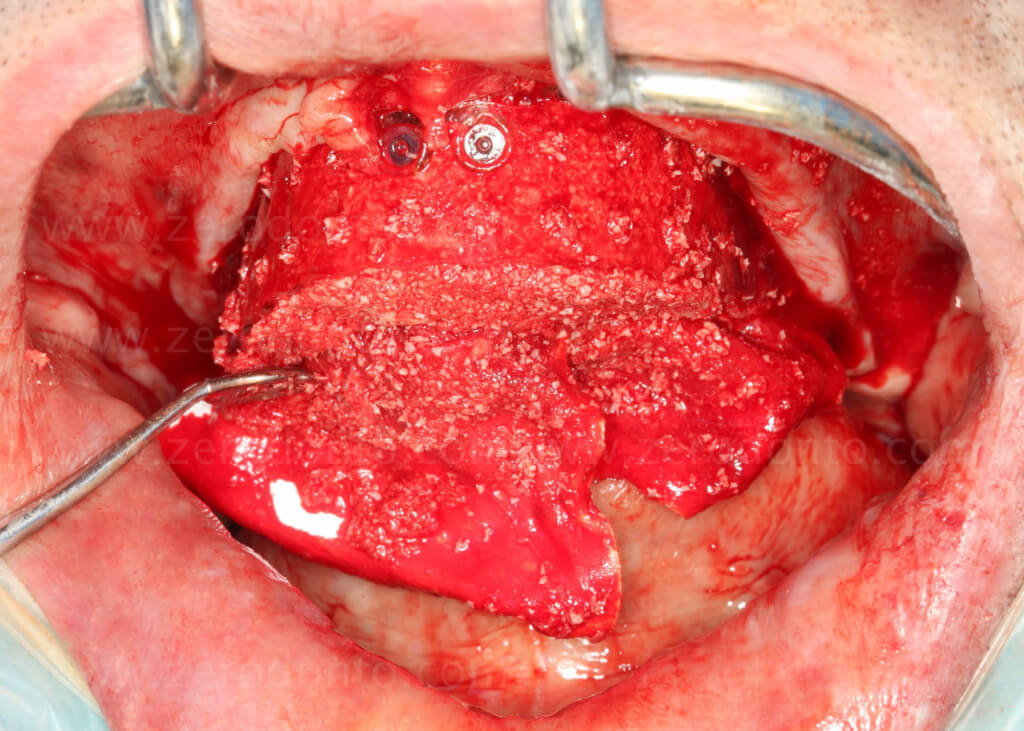
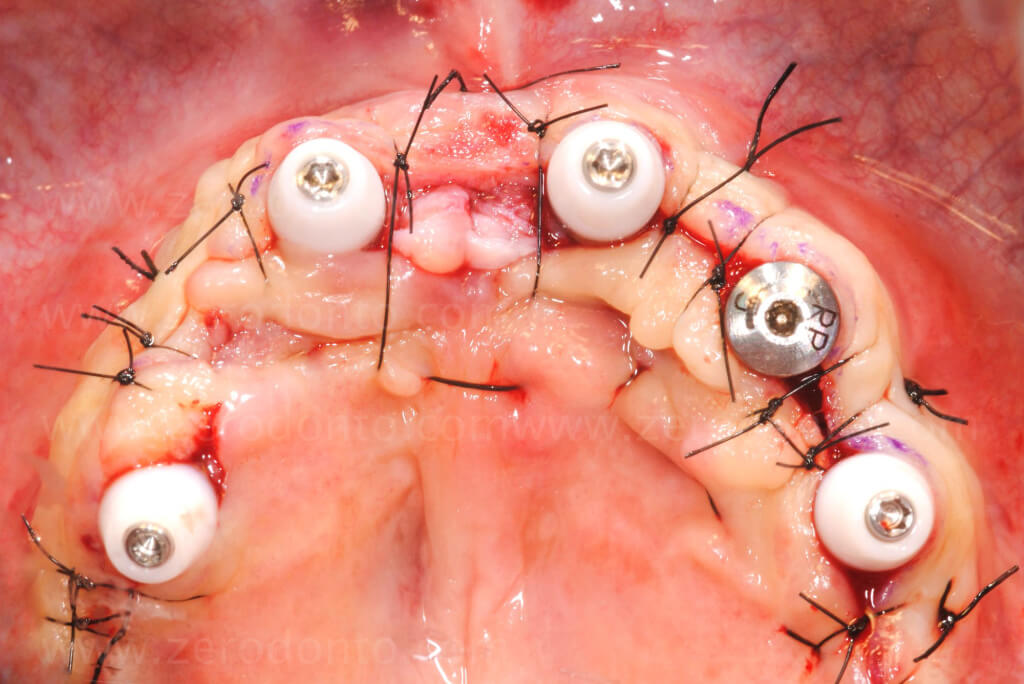
The first stage of the surgery completed, due to the considerable three-dimensional regeneration required, an additional amount of autologous bone was harvested from the mandibular corpus-ramus bilaterally (Fig. 5) before proceeding with the execution of the Fence Technique in the maxilla.
Fig. 5. Bimaxillary Rehabilitation: guided surgery in the mandible and the Fence Technique in the upper jaw




Modeling reabsorbable plates VIDEO (from a similar case)




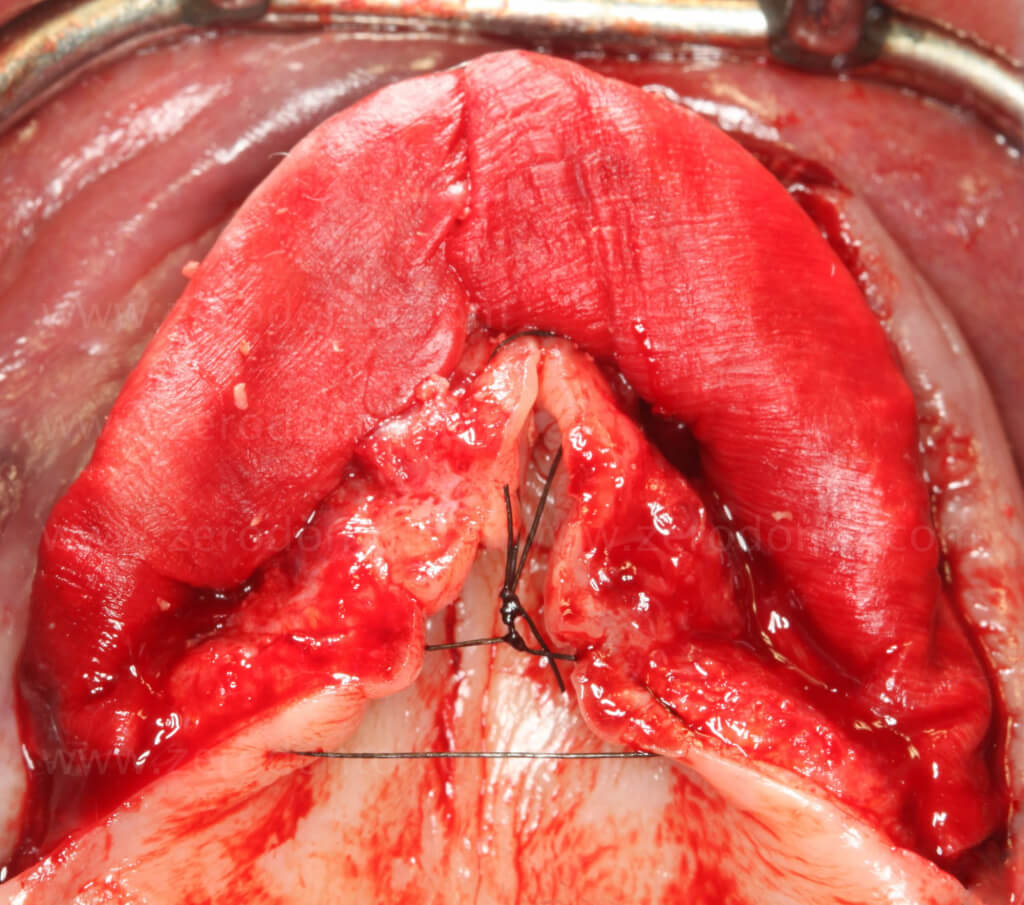
Sutures were removed two weeks post surgery. One week later, the full prostheses were readapted and rebased. The patient was instructed to wear the prostheses for as few consecutive hours as possible over the following 3 weeks (Fig. 6).
Fig. 6. Bimaxillary Rehabilitation: assessment after 2 months of healing


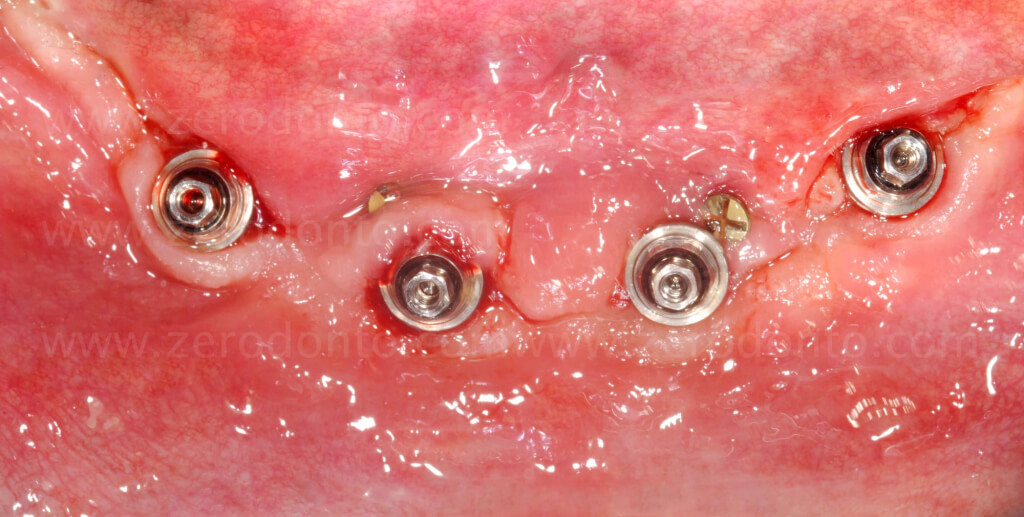

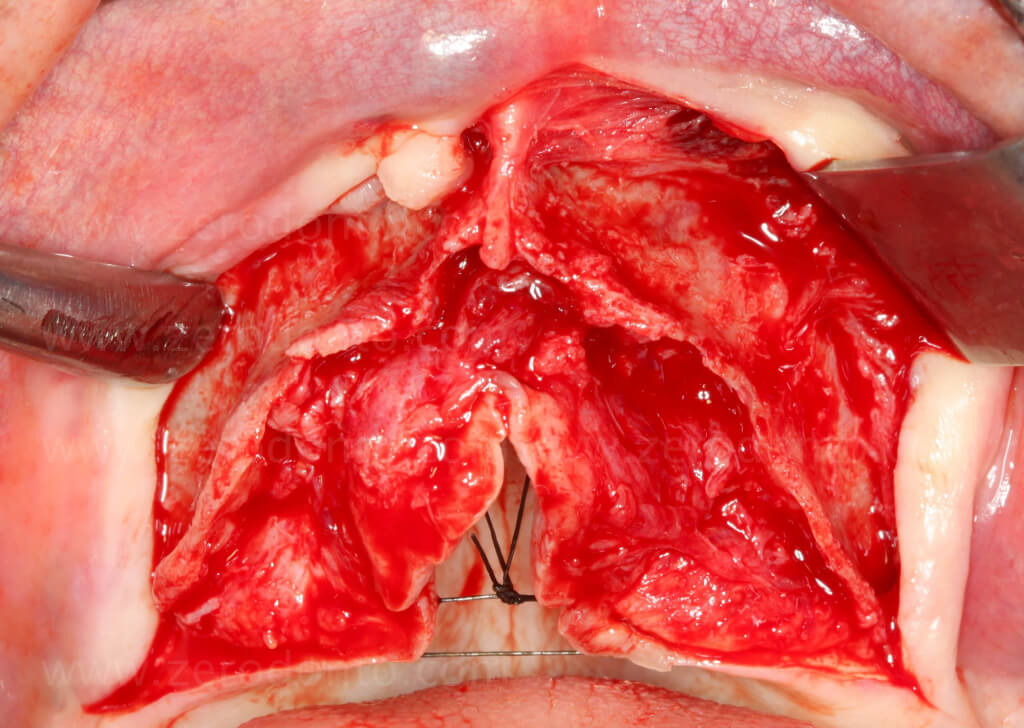
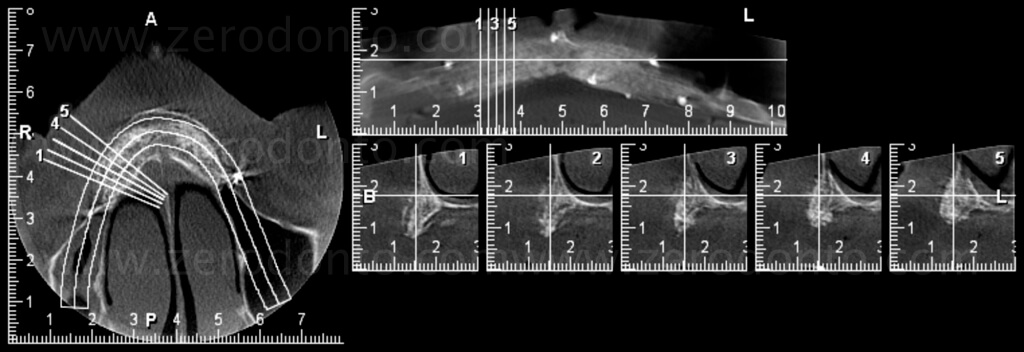
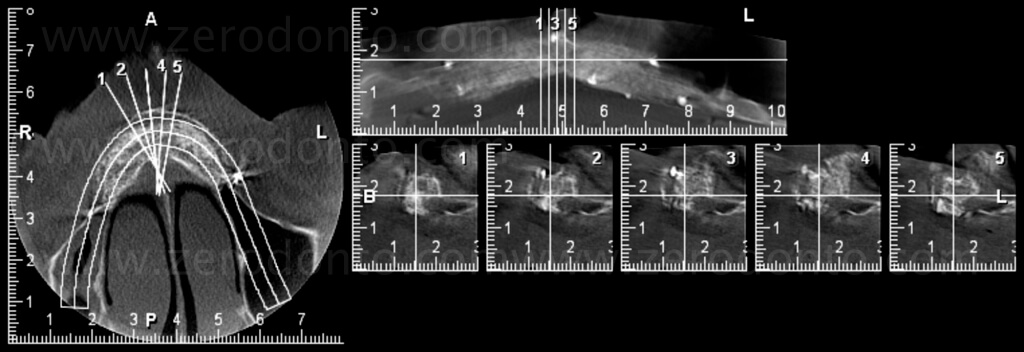
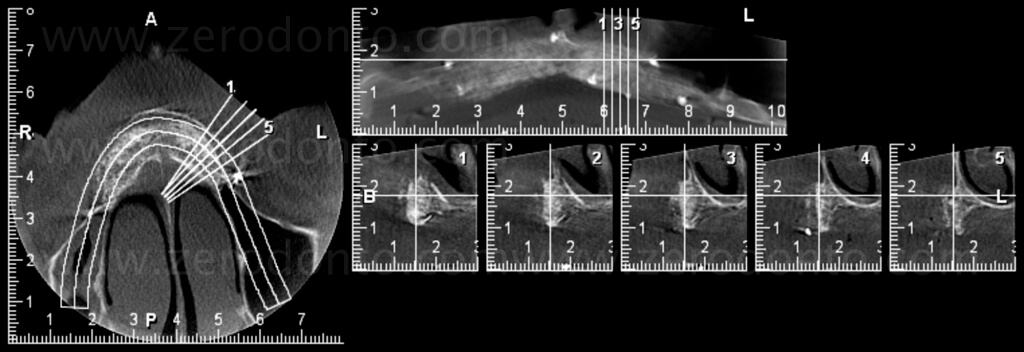
A CBCT (Fig. 7) was performed to plan the implant surgery and implant insertion took place after 8 months from the three-dimensional reconstruction of the upper jaw. The amount of bone available made it easier to obtain a correct prosthetically driven position, however the quality of the regenerated bone at the site 2.3 resulted inadequate for immediate loading. Thus, this implant was excluded from functional loading (Fig. 8).
Fig. 7. Bimaxillary Rehabilitation: Three-dimensional radiographic evaluation of the regeneration obtained by the Fence Technique
VIDEO – IMPLANT INSERTION
Fig. 8. Bimaxillary Rehabilitation: implant insertion in the upper jaw




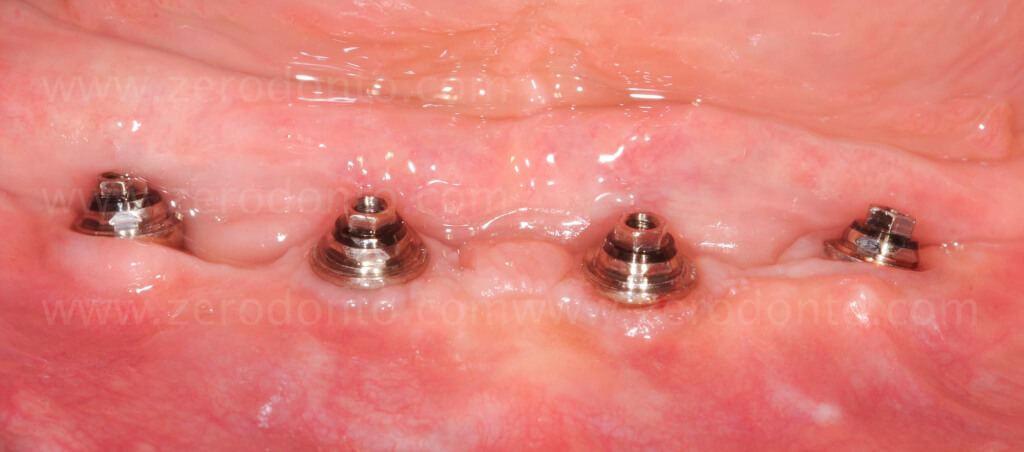
The final prosthetic phase was initiated only after having obtained an aesthetic and functional result deemed satisfactory by the patient and the team, and after an accurate quality control of the healing (Fig. 9).
Fig. 9. Bimaxillary Rehabilitation: peri-implant tissue healing



The final prosthetic phase was planned in four stages:
– Final impressions
– Testing of structures
– Aesthetic and phonetic testing
– Delivery of the final prosthesis
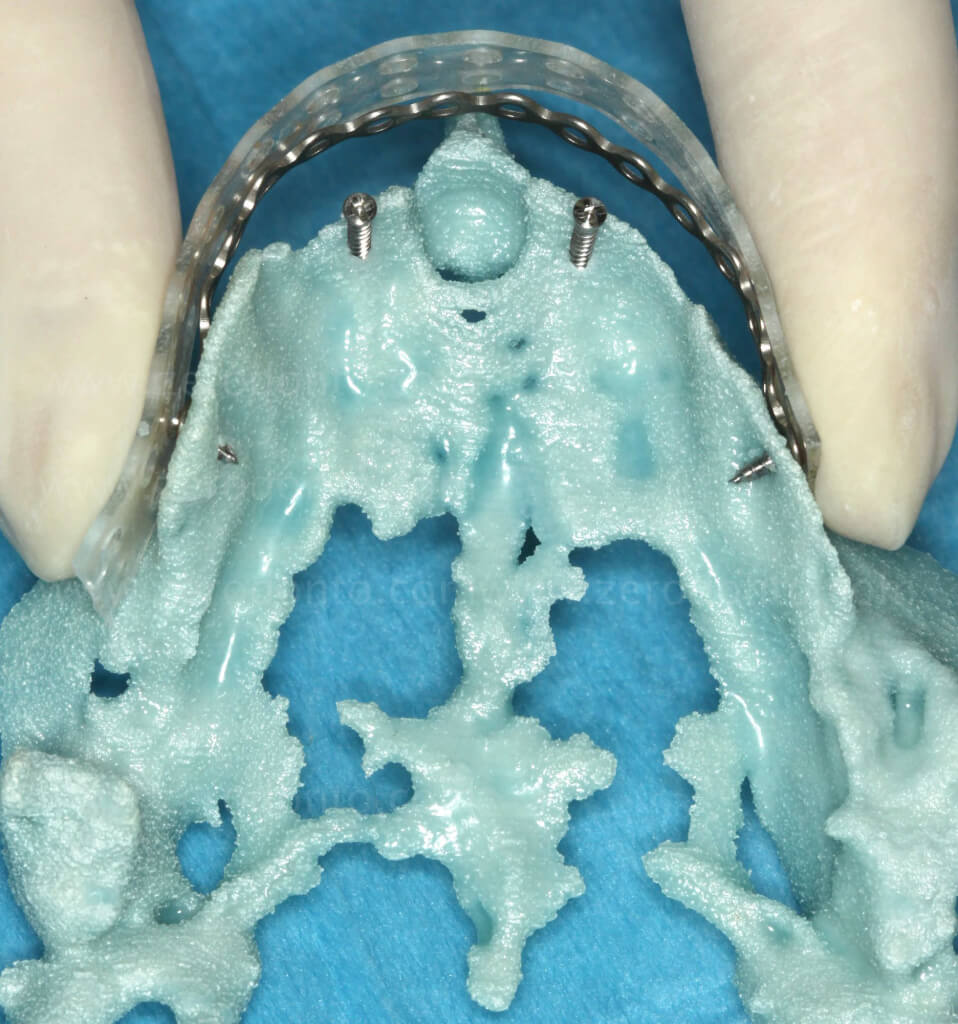
During the first phase (Fig. 10), the intermaxillary relation was registered with the provisional bridges already in function and possibly modified during the assessment period. These were screwed onto the master models to reproduce the vertical dimension reached and to customize the support pin of the articulator in relation to dynamic guides detected through the anatomy of the provisionals. During the clinical phase in normal occlusion, a wax model is taken that will help stabilize the models with the provisional bridges, also facilitating mounting in the articulator.
The data recording for the transfer of the models to the articulator can be performed with average values (configuring pre-defined settings of the condylar inserts of the articulator) or with individual values (individual registration of the posterior articular (joint) determinants), for example, through ultrasonic techniques with ARCUS ®digma II.

Fig. 10. Bimaxillary Rehabilitation: final impressions

Fig. 10. Bimaxillary Rehabilitation: final impressions
The most important aspect of structure testing is the evaluation of the adaptation of the structures to the implant abutments by means of a clinical analysis and possibly further X-rays (Fig. 11). At the conclusion of this phase, a new registration to verify the intermaxillary relations was performed.

Fig. 11. Bimaxillary rehabilitation: Structure assessment

Fig. 11. Bimaxillary rehabilitation: Structure assessment
True aesthetic assessment can only take place at this point: the shape and morphology of the teeth, the perception of colour, and the harmony of the dentofacial integration (Fig. 12).
Fig. 12. Bimaxillary Rehabilitation: Aesthetic trials



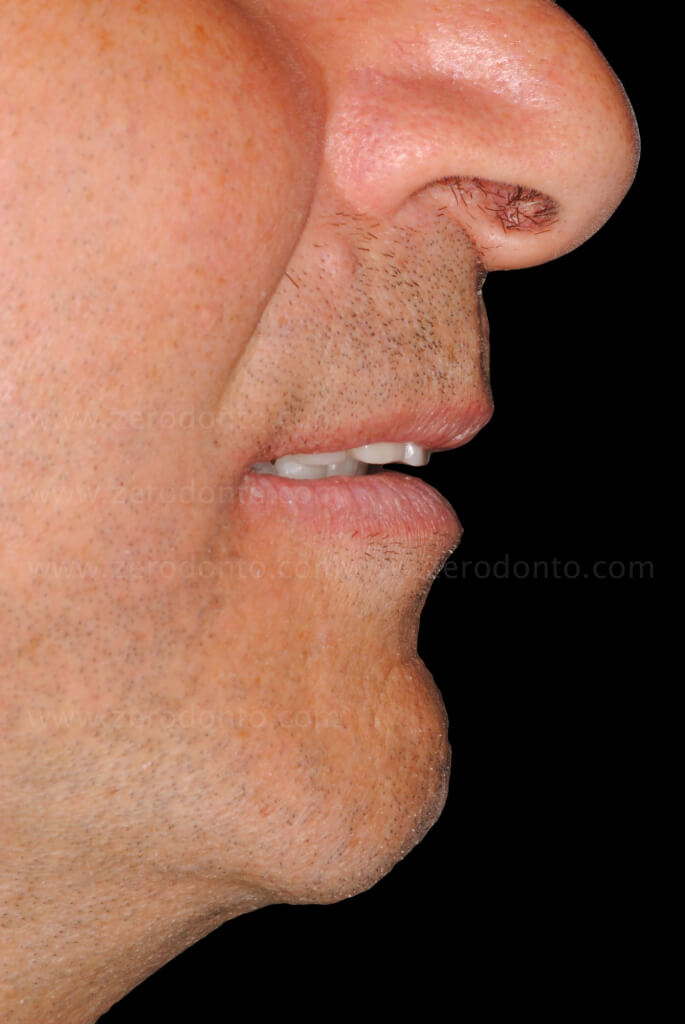

The day of delivery of the final prostheses (Fig. 13) foresees an accurate test of the closure/fixation of implant abutments using a special dynamometer. In addition, particular attention should be paid to the relationship of the static and dynamic occlusion. A final set of X-rays were taken, which then served as the starting point of the support therapy programme specifically designed for this patient (Figs. 14, 15).
Fig. 13. Bimaxillary Rehabilitation: delivery of the final prostheses









Fig. 14. Bimaxillary Rehabilitation: view of the prostheses removed during support therapy


Fig. 15. Bimaxillary Rehabilitation: X-ray image and view of smile


For further information please refer to the original article:
Merli M, Moscatelli M, Mazzoni A, Mazzoni S, Pagliaro U, Breschi L, Motroni A, Nieri M. Fence technique: guided bone regeneration for extensive three-dimensional augmentation. Int J Periodontics Restorative Dent 2013;33:129-136.
Bibliography:
Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 Suppl 1:2-9.
Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7 Suppl 1:S88-94.
Merli M, Moscatelli M, Mazzoni A, Mazzoni S, Pagliaro U, Breschi L, Motroni A, Nieri M. Fence technique: guided bone regeneration for extensive three-dimensional augmentation. Int J Periodontics Restorative Dent 2013;33:129-136.
Owens Wd, Felts JA, Spitznagel EL Jr. ASA physical status classifications: A study of consistency of ratings. Anesthesiology 1978;49:239-243.
Patzelt SB, Bahat O, Reynolds MA, Strub JR. The all-on-four treatment concept: a systematic review. Clin Implant Dent Relat Res 2014;16:836-855.

