Many adult patients require aligned teeth to improve their aesthetics, as dental exposure and smile are fundamental for the beauty of the face.
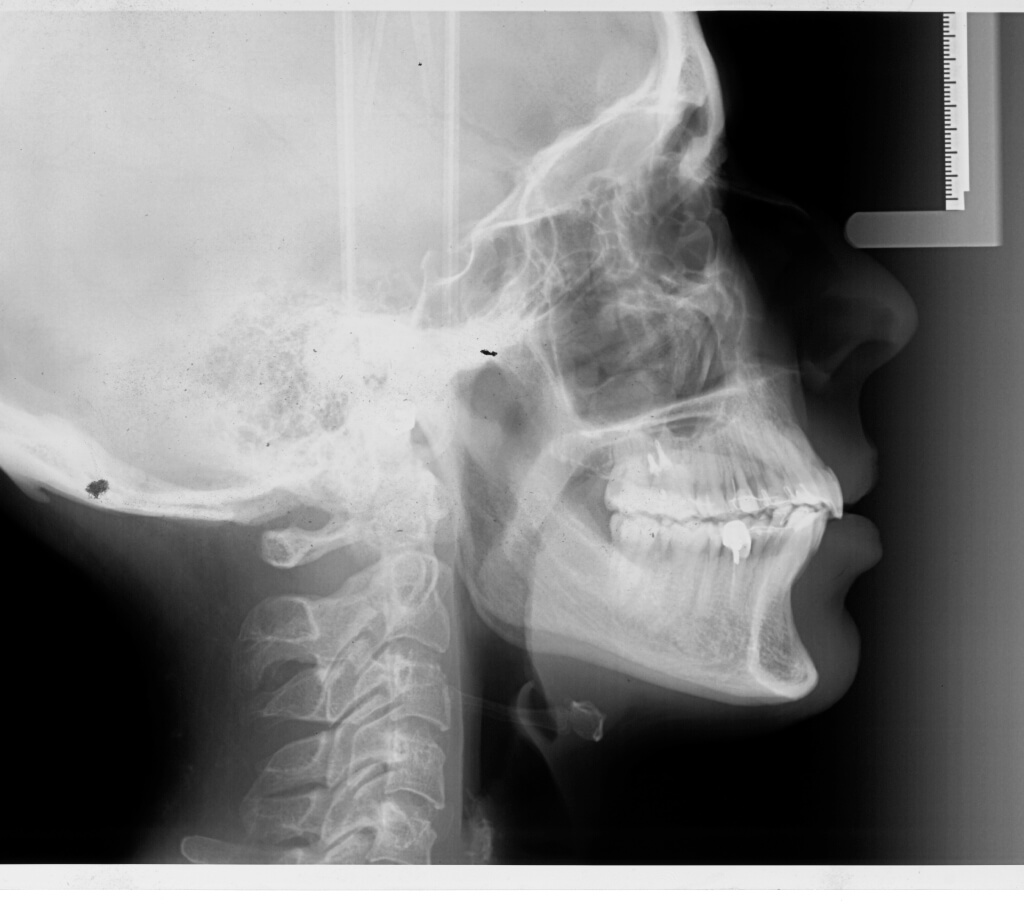
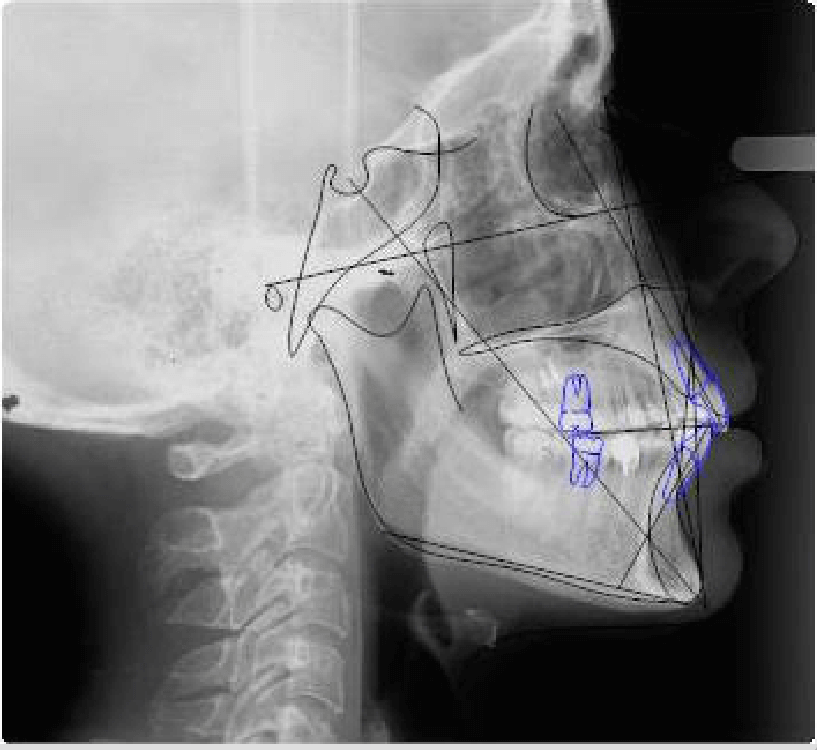
For this reason, the orthodontic treatment plan is the result of a careful radiographic examination and related cephalometric tracing, a detailed examination of the dental casts and related space analysis, but also an accurate aesthetic facial analysis.
We want to focus our attention on the exposure of the maxillary incisors with lips at rest. This is critical, for example, when we treat a case with overbite alterations, both in excess and in defect.
The clinical case we introduce is an example of treatment in case of anterior open bite. The patient asked for a fixed invisible lingual orthodontic therapy without brackets, to completely hide the presence of the device without phonetic distortions and tongue irritations.
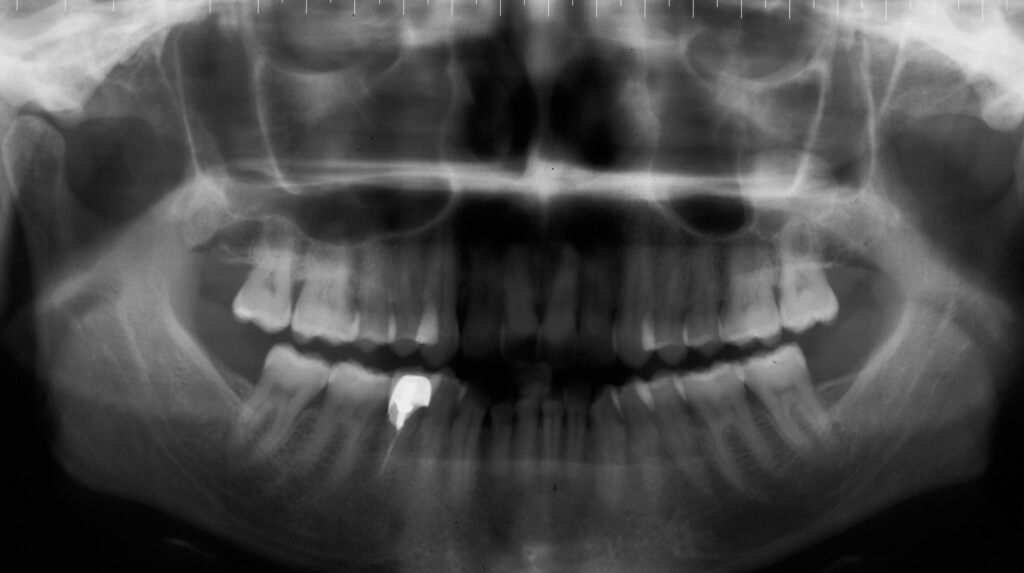
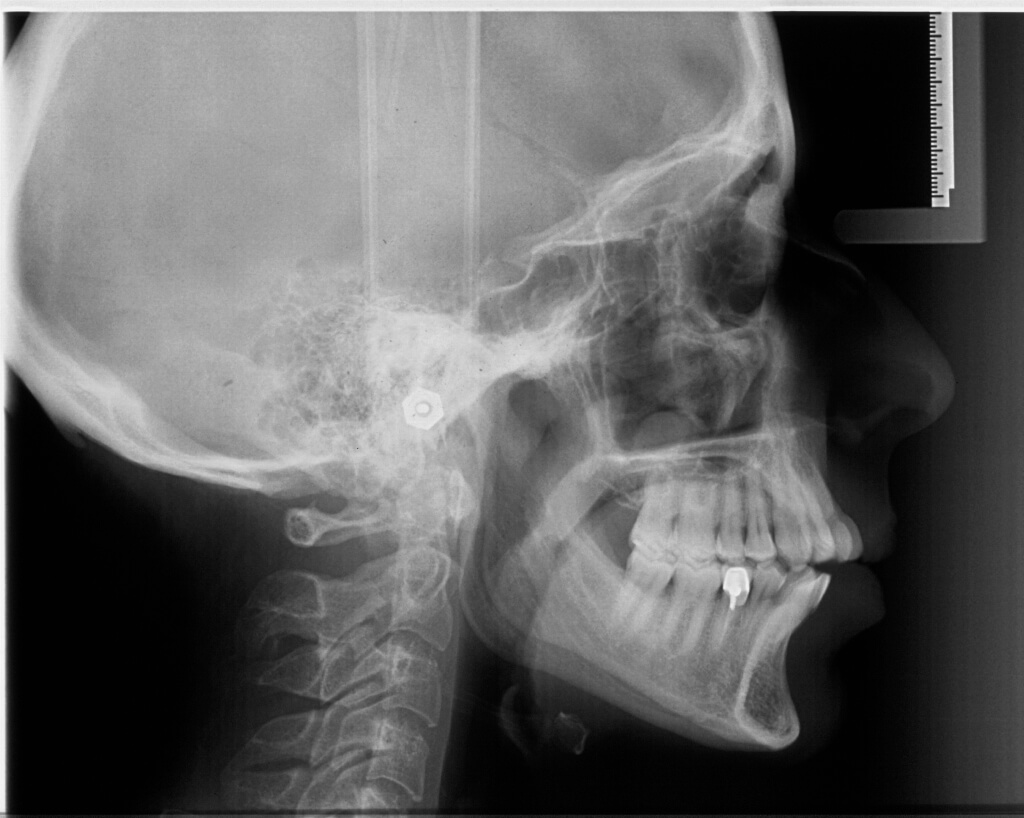
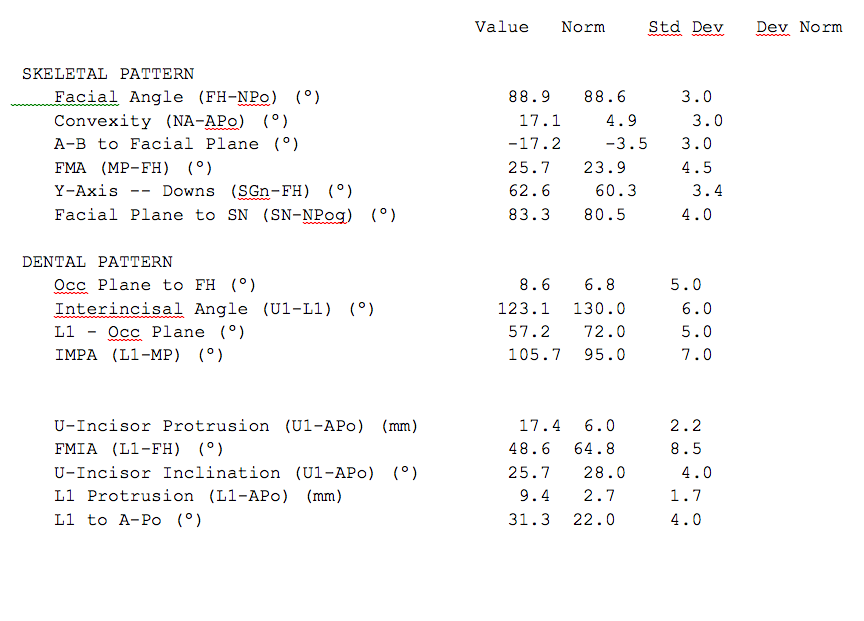
Ortopantomography, Latero-Lateral Teleradiography, cephalometric study, cephalometric values chart :




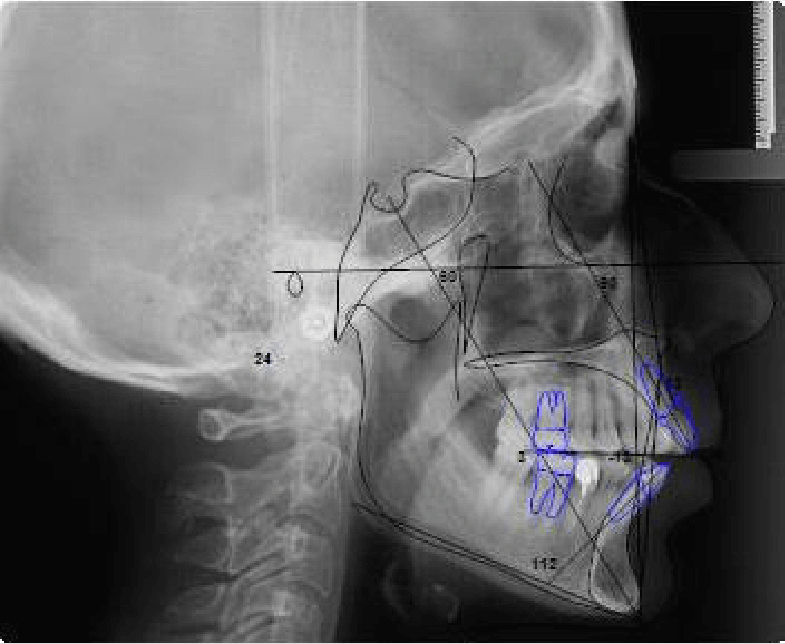
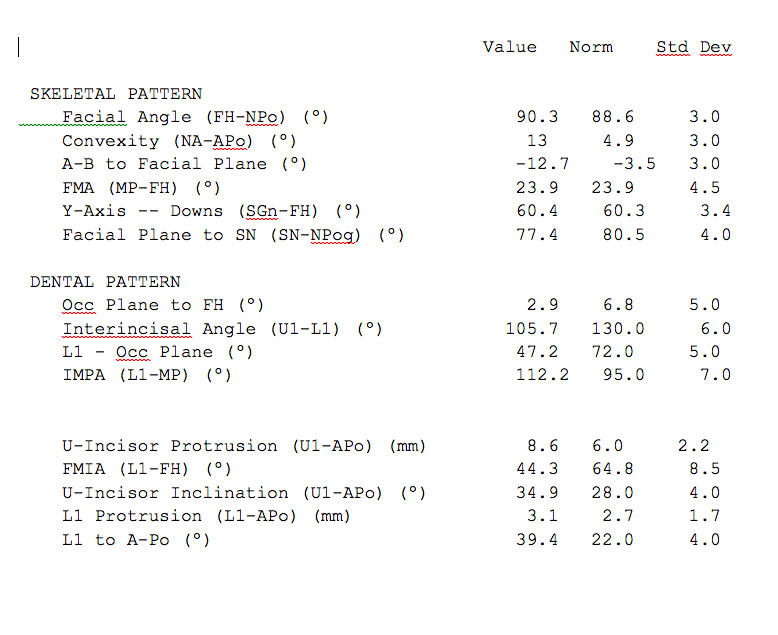
Despite a negative overbite, exposure of the upper incisal edge was about 2 mm, therefore the correction of the vertical discrepancy could not be obtained by extrusion of the frontal group.
It was also considered that an increased incisal edge exposure at the rest lip position would have already been obtained through the reduction of the excessive flaring of the frontal teeth.
The therapy was performed by intrusion of the posterior group and the lingualization of the upper and lower frontal groups.
For this purpose, it was first performed a stripping procedure from the distal surface of 12 to the distal surface of 22 and from the distal surface of 42 to the distal surface of 32, to create the space for the lingualization of the incisors.

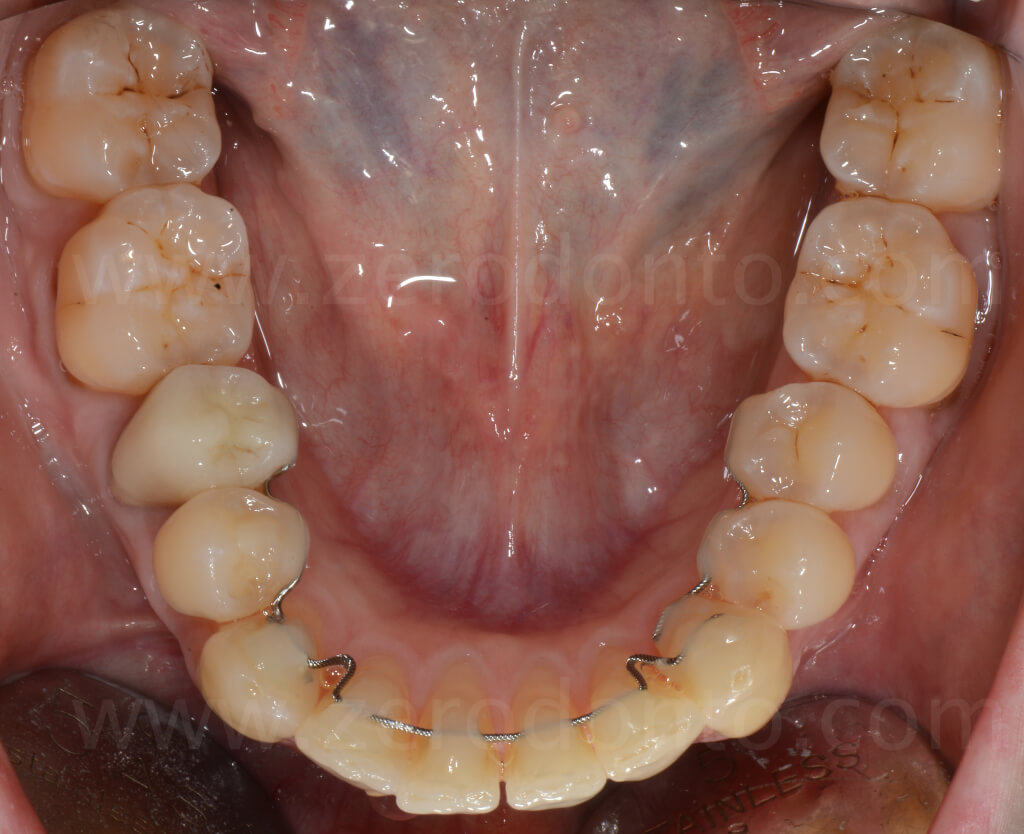
Stainless steel sectional wires were bonded onto the cuspid and bicuspid teeth of each quadrant. A retainer was modeled on the frontal group with U-shaped vertical loops between the lateral incisors and cuspids.


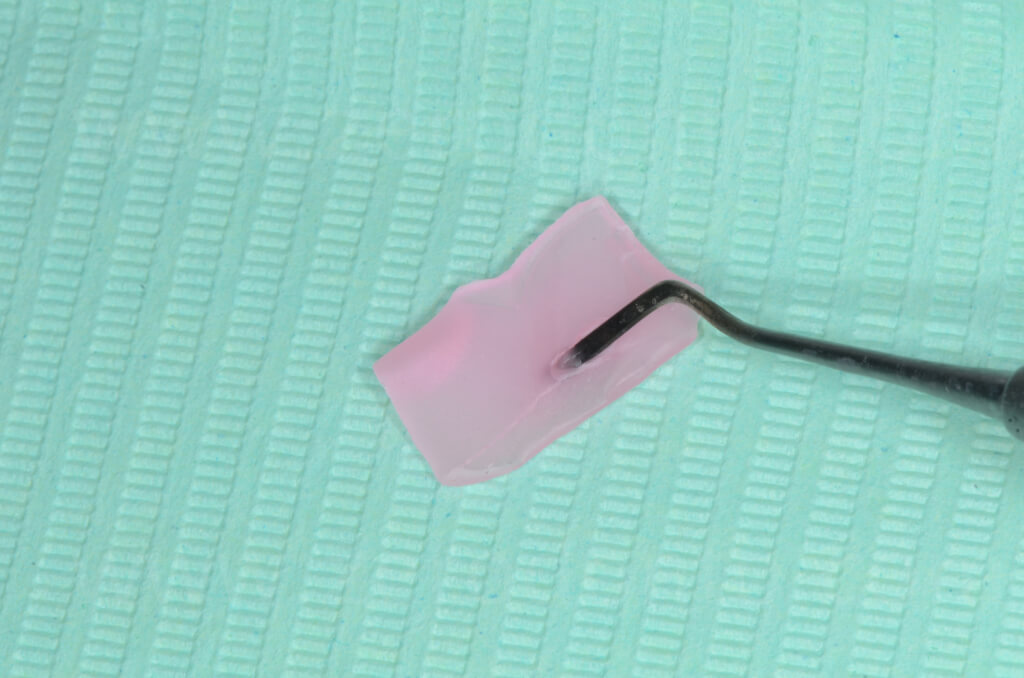
In order to obtain a sliding mechanics in the incisors area, the retainer was isolated with a wax sleeve.

Bonding procedure was first accomplished onto the incisors.
Subsequently, the retainer was bonded onto the cuspids, opening the loops of about 1.5-2 mm.
View of the loop before and after the bonding on 23:


The same system applied to the mandibular arch, after the stripping procedure:

Simultaneously to the retraction of the upper and lower frontal groups to obtain the intrusion of the posterior sectors, two miniscrews were applied at the buccal side between the first and second molars. An elastic chain was tied from one end to the screw while the other end was directly bonded onto the buccal aspect of the second molar.



The patient was checked once a month and at each follow-up it was either replaced the intrusion chain and activated the retraction archs.
To perform these activations, it was removed most of the composite covering the wire with a diamond cylindrical bur at low speed leaving a thin composite layer so as not to damage the wire. The last composite layer was removed with a leverage movement made with a dental explorer.
Debonding and rebonding of the loop on the maxillary left cuspid:


Retraction of the frontal group and gradual reduction of the spaces created by stripping:

Frontal view of the progressive reduction of the open bite:





Lateral view after several months of activations and gradual reduction of the open bite:






Comparison of the initial and final frontal views:


Ortopantomography, Latero-Lateral Teleradiography, cephalometric study, cephalometric values chart:

References
Macchi A, Rania S, Cirulli N. Una proposta per la gestione di disallineamenti anteriori: il mantenitore attivo di contenzione (MAC)”. Mondo Ortodontico 1999;5: 389-393.
Macchi A, Cirulli N. Fixed active retainer for minor anterior tooth movement. J Clinical Orthod 2000;34: 48-49.
Liou EJW, Chen LIJ, Huang CS. Nickel-titanium mandibular bonded lingual 3-3 retainer: for permanent retention and solving relapse of mandibular anterior crowding. Am J of Orthod Dentofacial Orthop 2001;119:443-449.
Mariniello A, Cozzolino F. Lingual active retainers to achieve teeth levelling in orthodontics: case series. International Dentistry SA 2008; Vol 10 N 5, pag. 24-29.
Kluemper GT, Marciani RD, Smith KJ. Biologic response to an intraoral extraosseous implant system: a pilot study. Implant Dent 1995;4:46-49.
Goodacre CJ, Brown DT, Roberts WE, Jeiroudi MT. Prosthodontic considerations when using implants for orthodontic anchorage. J Prosthet Dent 1997;77:162-170.
Huang LH, Shotwell JL, Wang HL. Dental implants for orthodontic anchorage. Am J Orthod Dentofacial Orthop 2005;127:713-722.
Florvaag B, Kneuertz P, Lazar F, Koebke J, Zöller JE, Braumann B, Mischkowski RA. Biomechanical properties of orthodontic miniscrews. An in-vitro study. J Orofac Orthop 2010;71(1):53-67.
Park YC, Lee HA, Choi NC, Kim DH. Open bite correction by intrusion of posterior teeth with miniscrews. Angle Orthod 2008;78(4):699-710.
Moon CH, Lee DG, Lee HS, Im JS, Baek SH. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod 2008;78(1):101-6.
Fritz U, Diedrich P, Wiechmann D. Lingual technique – patient’ characteristics, motivation and acceptance. Interpretation of a retrospective survey. J Orofac Orthop 2002;63:227-33.
Mauro Fradeani. La riabilitaione estetica in protesi fissa. Analisi Estetica. Quintessensa Edizioni 2004. Volume 1 capitoli 2 e 3.
Zachrisson BU, Minster L, Ogaard B, Birkhed D. Dental health assessed after interproximal enamel reduction: caries risk in posterior teeth. Am J Orthod Dentofacial Orthop 2011;139(1):90-8.
Zachrisson BU, Nyøygaard L, Mobarak K. Dental health assessed more than 10 years after interproximal enamel reduction of mandibular anterior teeth. Am J Orthod Dentofacial Orthop 2007;131(2):162-9.

