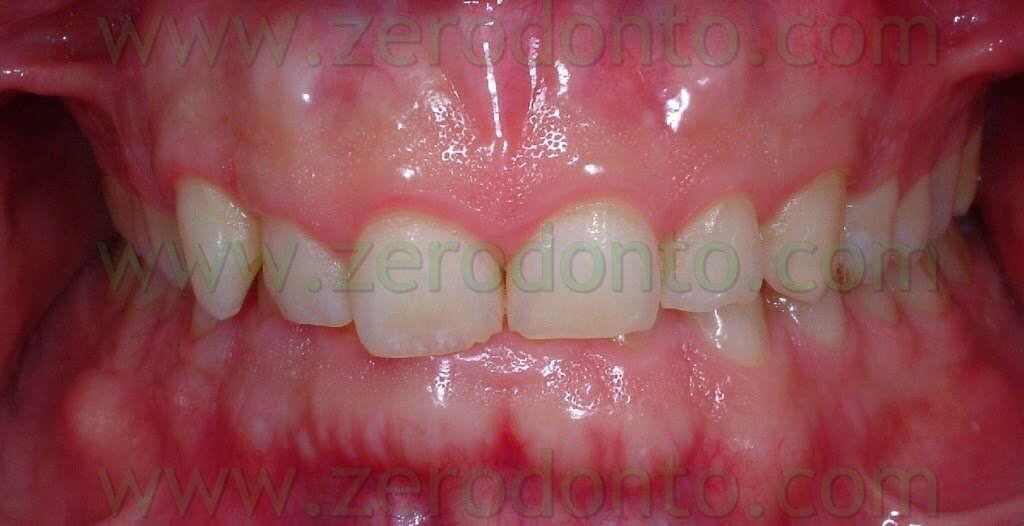
The patient that came to our chairside examination showed a first class malocclusion characterized by deep bite and the upper right canine impacted(Pics 1-7).







The patient, a 30 year old male, was looking for an invisible orthodontic treatment, since the normal multibracket buccal device would have made him feel ashamed because of its visibility.
He was also looking for a device set up on the lingual side of the teeth that was able to prevent phonetic alterations and annoying tongue decubites. This case was thus treated using a completely invisible lingual orthodontic therapy without brackets. This therapy was devised by Prof. Aldo MAcchi in the early 1990s and some of the operations performed were published together with Dr. Nunzio Cirulli (1-2). Afterwards other authors, as well, have performed lingual orthodontic treatments without brackets (3-4-5).
A deep-bite malocclusion is generally defined as an increase of the overbite (OB). The overbite is measured as the vertical distance between the incisal edge of the upper central incisor and the incisal edge of the lower central incisor, and its average is 2.5 mm +/- 2 mm. The treatment of this occlusal state requires an accurate diagnosis: this should include not only a radiographic and intraoral clinical examination, but also an aesthetic examination of the face, in order to choose whether to move mainly the maxillary or the mandibular front group.
The aesthetic evaluation must be performed checking the patient with lips at rest, while smiling and while speaking (6-7-8-9-10). In the first case the patient can be asked to utter 3 times in a row the word mommy or Emma and then stay still. This will let the patient adopt a relaxed position of the lips, in which the margin of the maxillary incisors should be exposed by around 2 mm. However this can vary up to 5 mm according to sex, age and height of the lips.
As a matter of fact, women tend to show a greater amount of incisal edge than men (3.40 mm vs. 1.91); aging reduces the amount of exposed teeth, both because of dental abrasion and a decrease in the tone of the perioral muscles (6-11): this process, while reducing the exposure of the upper incisors, increases the exposure of the lower ones. It is evident that longer lips cover a greater portion of teeth at rest (8-9).
When evaluating the smile of a patient, the dentist must make sure that it is as natural as possible in order to evaluate the amount of teeth and gum exposed.
A smile is considered aesthetic when the gummy exposure is around 2 mm (8-9-10).
The amount of gum exposed also depends on the shape of the teeth. Gummy smiles with teeth having a bigger length and width are better looking than those with smaller teeth, since the aesthetic performance also depends on the white/pink portion ratio (12).
During speech the incisal third of the upper incisors should be visible since otherwise the patient would acquire an ageing appearance: this is due to the fact that, as previously remarked, lower incisors become more and more evident as one gets older (11).
The patient under our examination presented a gummy smile with 4 mm of exposed gum and small teeth.
The clinical examination of the interested patient suggested to solve the problem of the deep bite mainly by an intrusion of the upper front group. It was also suggested, in order to improve aesthetics, to increase the size of the central incisors by applying porcelain veneers at the end of the therapy. As a matter of fact, the incisors were square-shaped being 8.5 mm long and wide: a large number of studies show an average width ranging between 8.3 and 9.3 and a length between 10.4 and 11.2 (12-13-14-15-16-17-18-19-20-21) – width being generally 80% of length (17-18-19-20). Nonetheless the patient didn’t want to change the shape of his teeth.
The first step was the intrusion of 11-12-21-22, joined together using a lingually bonded wire and mini-screws as anchorage. To locate the exact position of the mini-screws before their application by the roots of the dental elements, a very practical and fast technique devised by Dr. Fabio Cozzolino was used: it used tiny round snippets from the lead sheet inside X-ray plates. (Pics 8-10)



Such snippets, as big as the head of a micro-screw, were put between lateral incisors and canines, by the attached gum and kept in place by means of a denture adhesive (like corega-fit or kukident). In X-ray scans they appeared as tiny radio-opaque circlets and in case their position was not favourable they were easily moved away and the new position re-checked. (Pics 11-12-13).



The intrusive force was generated by means of elastic chains stretched from the head of the mini-screws to the third apical of the buccal surface of the lateral incisors. (Pics 14-15)


If we had applied the mini-screws lingually, only one between the roots of the centrals would have been enough. In this way the chains on the buccal surface of the laterals wouldn’t even have been visible; nonetheless the choice fell on the buccal position in order to give crown-buccal torque to the front group.
After an initial intrusion of the incisors only, a stabilizing sectional including canines as well was bonded in order to intrude them, too.
In case lingual brackets had been used, not only they would have encumbered the tongue but it would have also been necessary to create some occlusal raisings in order not to make the device hit the lower incisors and prevent possible detachment and dental wear.
Two months after the start of the therapy the mandibular arch was bonded, as well. When brackets therapy is performed, and some dental elements are included, the first goal is to align the elements on the arch in order to insert a thick steel arch as anchorage and create enough space for the impacted element. The second phase consisted in the surgical-orthodontic recovery of the canine. Lingual therapy without brackets requires the same biomechanical sequence: however, if the teeth do not require substantial shifts, it is possible to start creating the required space for the impacted element or, in case there is already enough space, it is possible to start the disimpaction of the impacted element, as in the present case. Anyway, using mini-screws also allows for a variation in the operating sequence since it is possible, as in this case, to begin with the intrusion phase: in the therapy with brackets this is possible after at least the alignment phase has been performed.
The 83 was thus extracted and at the same time the 43 was surgically exposed.
A .010 inches ligature wire was used to make a loop to be bonded on the exposed surface of the 43 as a link to apply the elastic tractions. (Pic 16)

In order not to change the aesthetics with a post-extraction hollow space, the root of the 83 was cut from its crown to make it possible to reposition it (the crown) in situ. A .017x .025 inches steel wire was used to make a sectional to be used as anchorage for the disimpaction of the 43 and as retention for the crown of the 83. (Pics 17-18)


The sectional extended from the 47 to the 42 and was modeled so as to adapt passively to the lingual surface of those teeth; moreover, it was bound on itself in order to create bends to mechanically retain the crown of the 83. The crown of the 83 was treated on its lingual surface in order to create tiny retention holes, 1-2 mm deep and wide, and then bonded on the sectional adhering to the lingual surfaces of the teeth, as previously explained. The traction for the extrusion of the 43 was accomplished using an elastic chain tied to the loop bonded on the 43, on one side, and bonded on the lingual surface of the crown of the 83, on the other. In the same session a .0175 interweaved steel wire was modelled into an active retainer bonded from the 42 to the 33 in order to correct slight rotations of the 32 and 41 and to move slightly the 33 buccally.
The patient was checked approximately every 4 weeks: every checkup the elastic intrusion chains of the maxillary front group and those used for the buccal extrusion of the 43 were replaced. After several checkups the crown of the 83 was replaced for aesthetic reasons by a provisional resin crown.
Afterwards, in order to increase the space for the 43 in the arch, a 0.16×0.22 inches sectional sealed with wax was bonded: this allowed it to move freely while the coil inserted in the sectional exerted its force. (Pic 19)

This sectional was also used as anchorage to continue at the same time with the extrusion of the 43.
When the position of the 43 was good enough from the vertical point of view the resin provisional was reduced to a shell in order to have enough space to move the 43 buccally. Subsequently a 0.16 x 0.22 inches TMA Alfa Beta spring was modelled on the lingual surface of the 43 and 44 and activated so as to generate the necessary force to move the canine in the desired direction. (Pic 20)

The 44 was stabilized on the 45 and 46 by a buccally bonded sectional.
When the maxillary intrusion was completed and the buccal shift of the 43 almost over a phase of alignment of those dental groups and a control of the torque of the 43 with the retainers activated were performed. (Pics 21-22)


The treatment ended after about 18 months: the patient was given removable retainers to be put on at night.






BEFORE
AFTER

Bibliography:
1. Macchi A, Rania S, Cirulli N. Una proposta per la gestione di disallineamenti anteriori: il mantenitore attivo di contenzione (MAC)”. Mondo Ortodontico, 1999; 5: 389-393.
2. Macchi A, Cirulli N. Fixed active retainer for minor anterior tooth movement. Journal of Clinical Orthodontics, 2000; 34: 48-49.
3. Liou EJW, Chen LIJ, Huang CS. Nickel-titanium mandibular bonded lingual 3-3 retainer: for permanent retention and solving relapse of mandibular anterior crowding. American Journal of Orthodontics and Dentofacial Orthopedics 2001; 119:443-449.
4. Musilli M. The Bracketless Fixed Orthodontics: nine years of clinical Experimentation. Prog in Orthod 9:72-91, 2008.
5. Mariniello A, Cozzolino F. Lingual active retainers to achieve teeth levelling in orthodontics: case series. International Dentistry SA Vol 10 N 5, pag. 24-29, 2008.
6. Mauro Fradeani. La riabilitaione estetica in protesi fissa. Analisi Estetica. Quintessensa Edizioni 2004. Volume 1 capitoli 2 e 3.
7. van der Geld PA, Oosterveld P, van Waas MA, Kuijpers-Jagtman AM. Digital videographic measurement of tooth display and lip position in smiling and speech: reliability and clinical application. Am J Orthod Dentofacial Orthop 2007; 131(3):301.e1-8
8. Vig RG, Brundo GC. The Kinetics of anterior tooth display. J Prosthet Dent 1978; 39:52-504.
9. Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofac Orthop 1993; 103:299-312.
10. Allen EP. Use of mucogingival surgical procedures to enhance esthetics. Dent Clin North Am 1988; 32:307-330.
11. Desai S, Upadhyay M, Nanda R. Dynamic smile analysis: changes with age. Am J Orhod Dentofacial Orthop 2009; 1 36 (3):310.e1-10
12. Ward DH. Proportional smile design using the recurring esthetic dental (red) proportion. Dent Clin North Am. 2001 Jan; 45(1):143-54.
13. Owens EG, Goodacre CJ, Loh PL, Hanke G, Okamura M, Jo KH, Munoz CA, Naylor WP. A multisenter interracial study of facial appearance. Part 2: A comparison of intraoral parameters. Int J Prosthodont 2002; 15:283-288.
14. Mavroskoufis F, Ritchie GM. The face-form as a guide for the selection of maxillary central incisors. J Prosthet Dent 1980; 43:501-505.
15. Ash MM. Wheeler’s dental anatomy. 7th ed. Philadelphia: W.B. Saunders Co.,1993.
16. Moores CFA, Thomsen SO, Jensen E, Yen PKJ. Mesiodistal crown diameters of the deciduos and permanent teeth in individuals. J Dent Res 1957; 36:39.
17. Mauro Fradeani. La riabilitaione estetica in protesi fissa. Analisi Estetica. Quintessensa Edizioni 2004. Volume 1 capitolo 5.
18. Shillinburg HT Jr,s, Kaplan MJ; Grace SC: Tooth dimensions-a comparative study. J South Calif dent Assoc 1972; 40:830-839.
19. Bjorndal AM, Henderson WG, Skidmore AE, Kellner FH. Anatomic measurement of human teeth extracted from males between the ages of17 and 21 years. Oral Surg Med Oral Pathol 1974; 38:71-803.
20. Mavroskoufis F, Ritchie GM. Variation in size and form between left and right maxillary central incisor teeth. J Prosthet Dent 1980; 43:254-257.
21. Sterret JD, Oliver T, Robinson F, Fortson W, Knaak B, Russel CM. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J Clin Periodontal 1999; 26:153-157.
For information:
zerodonto@gmail.com
tel. 0039 081 2451805

