CLINICAL CASE PERFORMED EMPLOYING FIXED LINGUAL ORTHODONTIC THERAPY WITHOUT BRACKETS
Lingual orthodontics rises from the need to satisfy the request, usually from adult patients, for a non visible treatment. This request can be fulfilled neither with a treatment employing porcelain buccal brackets nor with transparent trays. Both these therapies, although more aesthetically pleasant than metal buccal brackets, are not invisible: the only invisible option is lingual orthodontics.
Lingual orthodontics using brackets, despite the improvement of the brackets design over the years, can cause phonetic problems and tongue decubitus. Moreover the downsizing of the brackets in order to reduce the discomfort sometimes makes it difficult to control dental rotations and torque. This problem has only recently been overcome by Prof. Aldo Macchi’s i-TTR brackets which allow an accurate control of these parameters, as well. Prof. Macchi was also the first to perform, in the early nineties, lingual orthodontic treatments without brackets employing superelastic wires bonded on the lingual surface of the teeth.
This treatment was first carried out on patients who showed a relapse of misalignment after a previous therapy with brackets, using both the buccal and the lingual techniques. The aim was to solve the relapse avoiding a second treatment with brackets and to offer a completely invisible and comfortable solution. The subsequent step was to treat much harder cases and in patients undergoing a therapy for the first time.
The lingual therapy without brackets, subsequently performed by other authors, as well, is both invisible and extremely comfortable. Most patients who undergo lingual therapy without brackets after having undergone lingual therapy with brackets state that in the therapy without brackets they had a lot less nuisances or none at all. The phonetic alterations are hardly ever present and, when present, generally disappear in a few hours.
Tools employed and clinical procedure
In order to perform a lingual treatment without brackets the dentist will use wires that will be modelled, activated and bonded directly on the teeth employing fluid composite. Different kinds of wires will be used according to the different kinds of needed movements.
For example, Ni-Ti wires can be used to align a sector while steel wires (e.g. 16-22, 18-22, 17-25, etc) will be used to make stabilizing sectionals. 0.175 inches thick interweaved steel wires, commonly used to make passive retainers, can also be used to achieve an alignment.
These wires are modelled with first and second order bends and activated (active retainers) before being bonded on the lingual surface of the teeth. For example, step bends make derotations of the teeth as well as solving small crowdings (interproximal margins overlapping for less than 2mm) possible.
Second order bends, such as vertical U loops are added for more severe crowdings: the bends are closed for 2 mm during the bonding phase so that the elastic return of the wire makes enough space for the dental alignment. The wire can be activated to obtain both a horizontal and a vertical shift.
Before bonding the previously shaped wire (this operation can also be performed on the chalk mould by novices) the teeth are either cleaned with a small rubber wheel or brushed with a toothbrush. The lingual surfaces where the wire is to be bonded are first etched for 30 seconds with orthophosphoric acid, then the adhesive is applied and polymerized (from 5 to 30 seconds depending on the lamp used).
The retainer is bonded using medium viscosity fluid composite and covering the wire with a layer about 2 mm thick. The bonding sequence is another important element for the good outcome of the treatment using active retainers. In general it is necessary to bond first the teeth closer to the wire or the ones that are to be moved less. It is also important to keep the horizontal plane of the wire not to add unwanted intrusion or extrusion forces.
The patient treated with the active retainers is checked every 3-4 weeks and the retainers are reactivated. This is done detaching the wire from 1 or more teeth that are to be moved and performing the activations (such as adding step bends, expanding the previously shaped loops, bending the wire in buccal-lingual sense, etc.).
The detachment of the wire is obtained using a diamond bur at low RPM and under irrigation until almost all the composite covering the wire is worn. In order not to damage the wire the last layer of composite is not worn down with the bur and the wire is detached using a probe as a lever. After activating the retainer the layer of composite left on the tooth is coarsened with a diamond bur, this time without irrigation (this way it is not necessary to etch again), the adhesive is applied and the wire is bonded with fluid composite.
Clinical Case
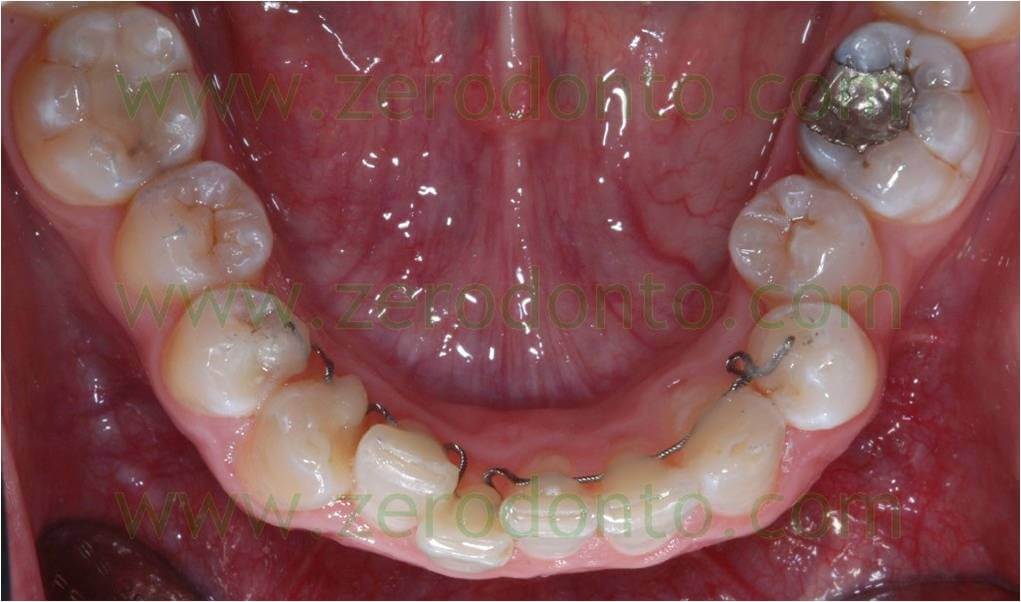
A patient came to our observation showing a moderate crowding of the maxillary arch (picture 1).
Pic. 1

An active retainer (picture 2) was applied from 44 to 34, shaped with mesial and distal U loops by the right central and lateral incisors and right canine and a distal U loop by the left canine.
Pic. 2
The retainer was activated bonding lingually the portion of the wire to be bonded on the 41: this determines the development of a force that shifts lingually the 41 and buccally the adjacent teeth. These shifts make the buccal-vestibular alignment possible while the loops make the needed space.
The bonding sequence, another aspect of primary importance for the wire to exert its action, is the following. The 42 is the first to be bonded as it is the most lingualized tooth and the closest to the wire.
Subsequently, the mesial and distal loops on the 41 are closed, it is bonded on elements 31, 32 and 33, keeping the horizontal plane in order not to add unwanted extrusive or intrusive forces. It is then bonded on the 34, closing the loop between the 33 and 34 of about 2 mm. The segment to be bonded on the 41 ran more lingually displaced than this element because of the previous activations: it was subsequently pushed with a utility tool on the 41 and then bonded. Finally, always closing the loops of about 2 mm, the retainer was bonded on the 44 and 43.
The patient was checked approximately every 3 weeks. During every check-up the retainer was detached from the 41, 42, 43 and 44 to activate the loops in expansion (opening them of about 2 mm) and to bend lingually the segment of retainer to be bonded on the 41. A mesial inset bend was subsequently added on the 43 to derotate it.
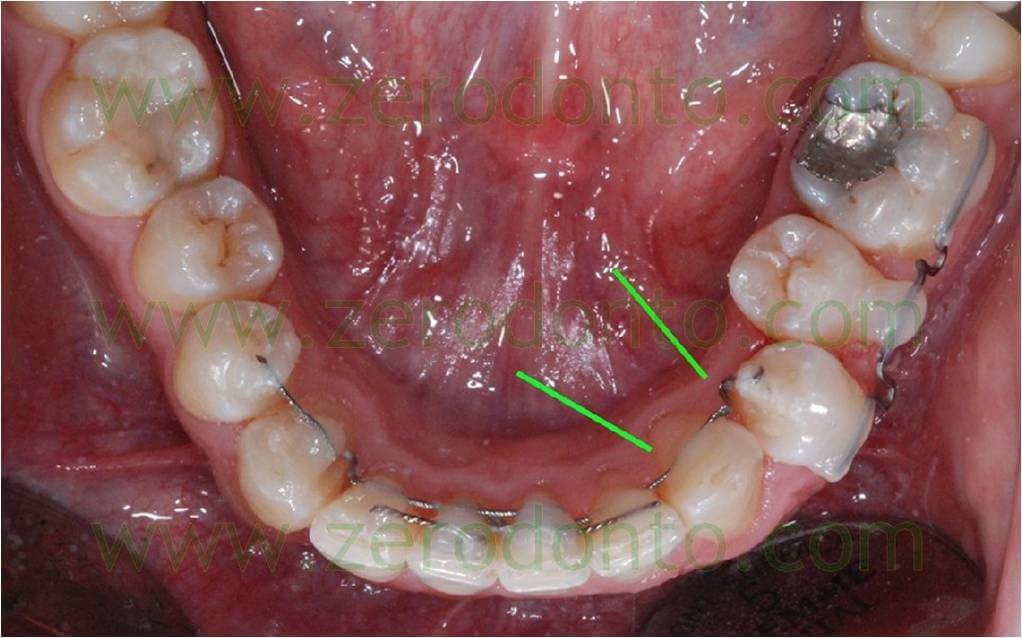
After approximately 4 months the previous active retainer made up of a single wire was replaced with a series of interweaved wires like the previous one and a TMA wire (picture 3).
Pic. 3

An interweaved wire was bonded from the 31 to the 44, passive on all the teeth but the 43. On the latter a loop and an inset bend were shaped to keep on derotating it. Two segments of passive retainers were bonded in overlay to stop the incisors in the achieved position (a segment bonded on the 41-42 and another one on the 32-31-41).
A further segment of active retainer was bonded on the elements 32-33 and 34, with a loop between the 33 and 34. This segment was activated to shift the 33 buccaly and the 34 lingually, applying the V bend principle: before bonding it, the portions of the wire to be sticked on the elements 34 and 32 ran lingually – as the marks on picture 4 clearly show – in order to draw a V with the apex being by the canine and turned buccally.
Pic. 4
Furthermore a sectional was shaped using a 16-22 TMA wire in order to move the 35 buccally. This sectional was bonded from the 34 to the 36; some loops were also added to increase its elasticity and the section to be bonded on the 35 was bent buccally.
The alignment was achieved in about 6 months and a fixed retainer was put on (picture 5).
Pic. 5

Bibliography
1. Macchi A, Cirulli N. “Fixed Active Retainer for Minor Anterior Tooth Movement”. Journal of Clinical Orthodontics, 2000.
2.Macchi A, Rania S, Cirulli . “Una proposta per la gestione di disallineamenti anteriori: il mantenitore attivo di contenzione (MAC)”. Mondo Ortodontico, 1999.
3.Liou EJW, Chen LIJ, Huang CS. “Nickel-titanium mandibular bonded lingual 3-3 retainer: for permanent retention and solving relapse of mandibular anterior crowding”. Am J Orthod Dentofacial Orthop 119:443-9, 2001.
4.Musilli M. The Bracketless Fixed Orthodontics: nine years of clinical Experimentation. Prog in Orthod 9:72-91, 2008.
5.Mariniello A, Cozzolino F. Lingual active retainers to achieve teeth levelling in orthodontics: case series. International Dentistry SA Vol 10 N 5, pag. 24-29, 2008.
For information:
zerodonto@gmail.com
tel. 0039 081 2451805

