Bracketless invisible orthodontics is a new orthodontic device to treat malocclusion, based on the use of thin wires directly bonded on invisible teeth surfaces.
Such appliance is not visible but also well comfortable for the tongue and soft tissues, thanks to the extremely personalized and anatomical modelling, and takes less space than the lingual brackets.
So it represents a possible therapeutic alternative to propose to all those patients that need an invisible and painless treatment.
The application field goes to the simple levelling therapies to the more complex, who need for example teeth extractions and bodily teeth movement. The association to miniscrews can be very useful, as it also occurs in the classical brackets therapy.
The case that we propose is an extractive treatment with a dental and a skeletal anchorage.
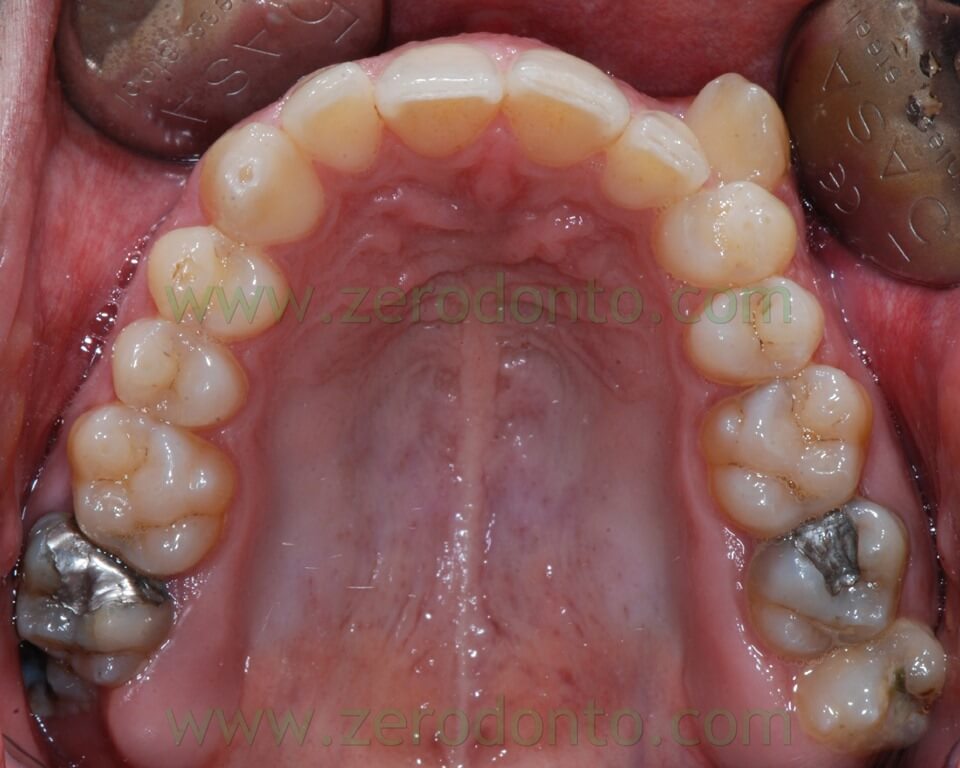
The patient, came to our attention, had a malocclusion characterized by:
- first class molar and canine on the right
- second class molar on the left
- complete absence of space for the left ectopic buccal canine;
- upper and lower teeth crowding
- upper midline shifted 2,5 mm to the left
- Overbite of 1 mm for 12, 3 mm for 11 and 21, 0 mm for 22.
- Overjet of 2,5 mm for 12, 2 mm for 11 and 21, 0 mm for 22.







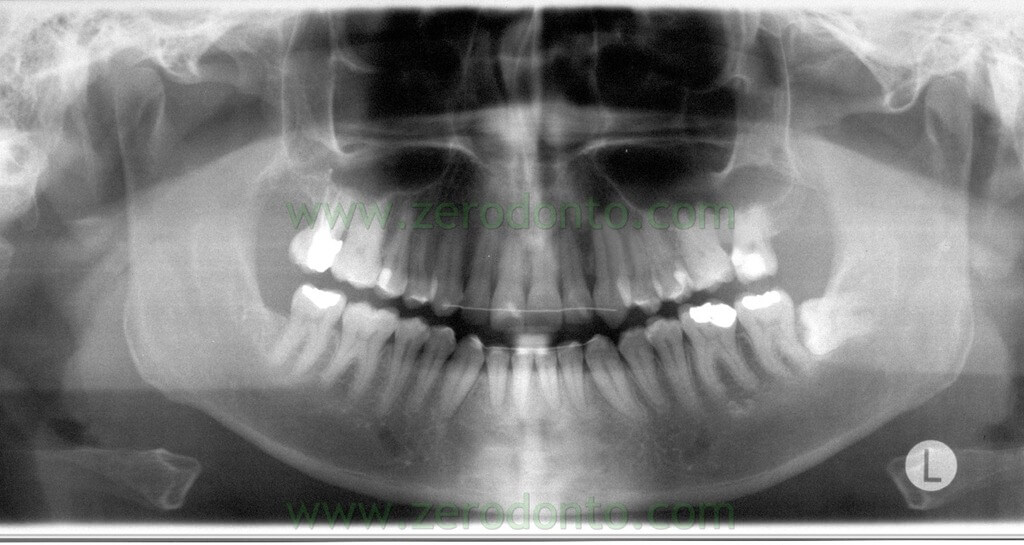
The orthopantomography showed:
- teeth 17 and 27 previous root canal therapies
- teeth 47, 36, 37 extensive reconstructions
- impacted teeth 38
The cephalometric tracing was carried out by identifying 17 landmarks that evaluated dental, skeletal and soft tissues changes. A perpendicular line was drawn to the SN plane from the intersection of the anterior wall of sella turcica and the anterior cli- noid processes in order to form a vertical reference line.
The stability of these landmarks is widely documented in literature.

Cephalometric landmarks and skeletal measurements. Landmarks: S, sella; Sa, intersection of the anterior wall of sella turcica and the anterior clinoid processes; Na, nasion; Or, orbitale; Po, porion; A, A point; B, B point; Go, gonion; UL, most anterior point of the upper lip; LL, most anterior point of the lower lip; u6f, furcation point of the upper first molar; u6s, sulcus between buccal tubercules of the upper first molar; u5b, tip of the buccal cusp of the upper second premolar; u4b, tip of the buccal cusp of the upper first premolar; U1i, incisal edge of the upper central incisor; L1i, incisal edge of the lower central incisor. SV indicates vertical reference line. Skeletal measurements: 1, SNA; 2, SNB; 3, ANB; 4, Go-Gn SN; 5, FMA; 6, UL – SV; 7, LL – SV. B, dental angular measurements (o): 1, U1-SN; 2, U4-SN; 3, U5-SN; 4, U6-SN. Dental linear Measurements (mm): 5, U6 – SN; 6, U1 – SV; 7, U4 – SV; 8, U5 – SV; 9, U6 – SV.
| Skeletal angular measurements |
| SNA (°) |
81 |
| SNB (°) |
76 |
| ANB (°) |
5 |
| Go-Gn SN (°) |
25 |
| FMA (°) |
20 |
|
|
| Soft tissues measurements |
| UL – SV (mm) |
76 |
| LL-SV(mm) |
68,5 |
|
|
| Dental angular measurements |
| U1-SN (°) |
101 |
| U4-SN (°) |
87 |
| U5-SN (°) |
82 |
| U6-SN (°) |
72 |
|
|
| Dental linear measurements |
| U6-SN(mm) |
67,5 |
| U6-SV(mm) |
58 |
| U1-SV(mm) |
44 |
| U4-SV(mm) |
51 |
| U5-SV(mm) |
36 |
| Overjet (mm) |
2 |
| Overbite (mm) |
3 |
Considering the crowding amount in the upper arch we thought to an extraction treatment for the recovery of 23 space.
We chose to extract tooth 27 instead of 24 because it was compromised by a previous root canal therapy and had a great amalgam reconstruction.

In a first step the residual extraction space was managed by activating the 26-28 closure space with anchorage loss. For this purpose was modelled a spring with a .016 – .022 Titanium Molybdenum (TMA) wire.

The coil was bonded to the 28 lingual surface (according to the traditional procedure and flowable resin) and then to the 26, by activating the mesial arm which, modelled in contraction, moved distally to the lingual first molar surface. The closure elastic movement developed the required force to mesialize 28 and distalize 26.
After one month the previous spring has been replaced with one that starting from the vestibular surface of 28 arrived at the disto-palatal, turned on itself to continue forward describing an interdental loop which was bonded in opening. An elastic chain was used to better control the dental rotations, linked to the spring in the interdental space and directly bonded to the buccal surface of 26.



The following photos show the space closure achieved at the beginning of the fourth month:



When we chose to stop 28 mesialization and to use the remaining space only for the distalization from 24 to 26 it has been inserted a palatal miniscrews, mesial to 28.

This miniscrew was used both as distalization anchorage and to stop 28. A .016 – .016 inches stainless steel sectional has been shaped to anchor 28 to miniscrew. Another wire .016 – .016 inches steel has been shaped to realize a sectional bonded from 24 to 26 with an apical loop between 25 and 26. The distalization force was developed by an elastic chain linked on one side to the loop and on the other inserted in the screw’s head.
At the next check we inserted a second miniscrew, mesial and buccal to 28, to apply also buccally the distal force and control a possible rotation of the sector.


The lower arch alignment has been realized by the application of an active retainer modelled according to the criteria widely exposed in previous articles.

In particular it have been modelled:
- a step bend to level 31-32
- some U vertical loops to expand canine sites
Before the bonding procedure the wire has been bent with the help of two pliers ( the bird beak and the Weinghart) in order to move lingually the sections to bond on teeth 33 and 34.
The lower retainer bonding sequence was the following:
- Inizial bonding on 33, 41 and 42;
- by closing the loops the mesial and distal to 33 , the wire was bonded on 34 and 35;
- by closing the loops the mesial and distal to 43 , the wire was bonded on 44 and 45;
- Due to the step bend the wire was displaced lingually to the tooth 41, so was pushed on the lingual surfaces of these teeth by means of a utility probe and then bonded;
- Due to previous activations, the segments to be bonded onto 33 and 43, were displaced lingually so were pushed on the lingual surfaces by means of a utility probe and then bonded.
- This retainer was activated every 4 weeks by traditional debonding, activating and bonding procedure widely discussed in other articles.
When lateral sector distalization was almost completed an upper arch active retainer was applied to start to move the midline. This retainer was extended from 24 to 14, had a vertical U loop mesial and distal 23, and mesial 12. Was bonded on toot 24 to the composite resin of the previous bonded stabilization sectional.

The elastic return of the handles bonded in contraction developed the force to move the sector to the right. There was a step bend to level the central incisors and the handles were activated to move the frontal sector to the right.

After 23 alignment, in a phase in which the palatal miniscrew had been already removed, a double retainer was applied to activate 22-21 space closure with derotation of 22.

The rational for the use of a double retainer is to increase the anchorage of the sector that we don’t want to move, with two retainers in overlay.
The following photos were taken at the end of distalization from 24 to 26 and alignment:





Final orthopantomography
Final teleradiography

Cepalometric tracing

|
Before distalization |
After distalization |
| Skeletal angular measurements |
| SNA (°) |
81 |
81 |
| SNB (°) |
76 |
75 |
| ANB (°) |
5 |
5 |
| Go-Gn SN (°) |
25 |
26 |
| FMA (°) |
20 |
21 |
|
|
|
| Soft tissues measurements |
| UL – SV (mm) |
76 |
75 |
| LL-SV(mm) |
68,5 |
70 |
|
| Dental angular measurements |
| U1-SN (°) |
101 |
103 |
| U4-SN (°) |
87 |
79 |
| U5-SN (°) |
82 |
76 |
| U6-SN (°) |
72 |
70 |
|
|
|
| Dental linear measurements |
| U6-SN(mm) |
67,5 |
64 |
| U6-SV(mm) |
58 |
62 |
| U1-SV(mm) |
44 |
37 |
| U4-SV(mm) |
51 |
44 |
| U5-SV(mm) |
36 |
33 |
| Overjet (mm) |
2 |
2,5 |
| Overbite (mm) |
3 |
2 |
References
Macchi A, Rania S, Cirulli N. Una proposta per la gestione di disallineamenti anteriori: il mantenitore attivo di contenzione (MAC)”. Mondo Ortodontico, 1999; 5: 389-393.
Macchi A, Cirulli N. Fixed active retainer for minor anterior tooth movement. Journal of Clinical Orthodontics, 2000; 34: 48-49.
Liou EJW, Chen LIJ, Huang CS. Nickel-titanium mandibular bonded lingual 3-3 retainer: for permanent retention and solving relapse of mandibular anterior crowding. American Journal of Orthodontics and Dentofacial Orthopedics 2001; 119:443-449.
Mariniello A, Cozzolino F. Lingual active retainers to achieve teeth levelling in orthodontics: case series. International Dentistry SA Vol 10 N 5, pag. 24-29, 2008.
Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod 1983;5:1-46.
Gulati S, Kharbanda OP, Parkash H. Dental and skeletal changes after intraoral molar distalization with sectional jig assembly. Am J Orthod Dentofacial Orthop 1998;114:319-27.
Gelgör IE, Büyükyilmaz T, Karaman AI, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distaliza- tion. Angle Orthod 2004;74:838-50.
For information:
zerodonto@gmail.com

