Introduction
Sauro, 50 years old, entrepreneur and semi professional sports-fisherman.
Presented in 2004 with heavy loss of occlusal, palatal and incisal dental surfaces.
Over-bite 0mm. Over-jet 0mm.
18 remaining teeth, 9 in the upper and 9 in the lower jaw.
Many teeth are over-erupted, but they are not mobile, and the patient doesn’t show any signs of periodontal disease.
Very good oral hygiene.
Good general health.
All the lower molars and some of the upper molars and premolars were lost because they were too damaged to be restored, according to him.
Some teeth have been endodontically treated because of major sensitivity.
When chewing, the patient regularly suffers from muscle fatigue and he has had to change his diet to accomodate this problem.
He is also very much concerned with the appearance of his smile and says he cannot laugh naturally and with confidence.
Clinical case

Initial extra-oral images: the upper teeth are almost completely unseen, causing a major impairment in the patient’s smile. The fatty tissues of the cheeks partially hide the shape of the masseter muscles, which are hyper-developed.

Initial intra-oral images: note, in addition to the major wear of the eight upper and lower anterior teeth, the absence of all the lower molars, the marked over eruption of 26 and 27 and the absence of over-bite and over-jet.

The 8 incisors appear heavily worn, but the remaining posterior teeth are well maintained.
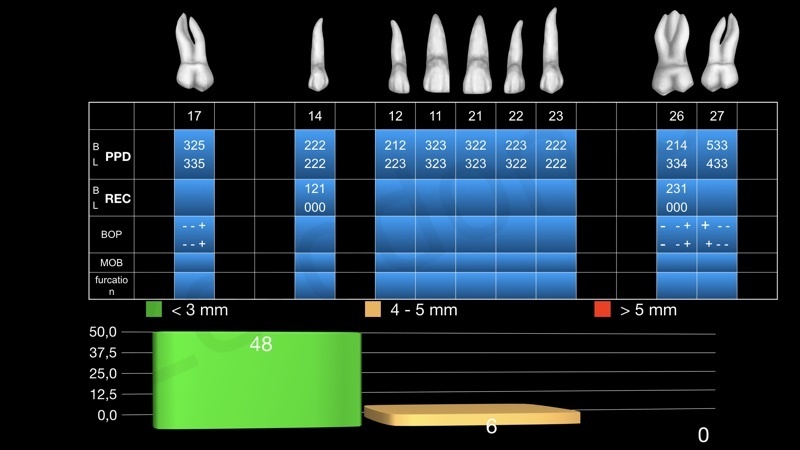
Initial periodontal charting upper arch: 6 out of 54 sites show a 4-5mm ppd with bleeding on probing; all the others are 3 or below, with no bleeding.

Initial periodontal charting lower arch: the only problem here is 4mm of recession on the mesio-buccal surface of tooth 34
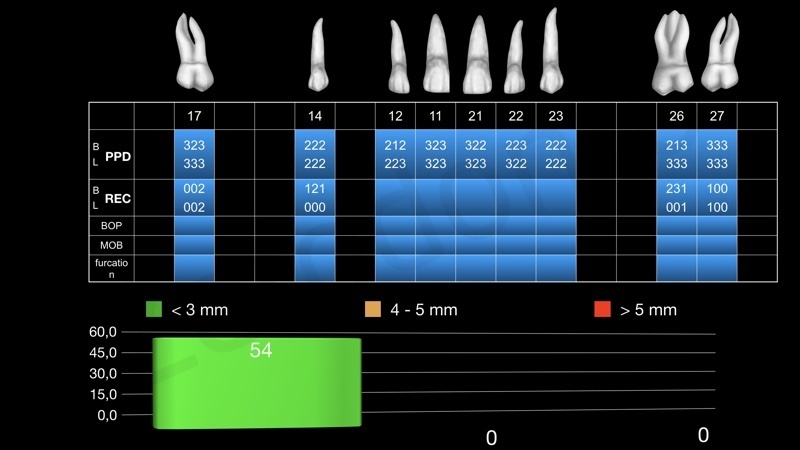
Periodontal charting upper arch after initial periodontal non surgical treatment: no more bleeding on probing and all the sites probing 3mm or less. As a consequence, there has been a slight increase in the recession values at those sites and the molars have lost, in total, 1-2mm of periodontal attachment.

Bleeding on probing before and after initial periodontal non surgical treatment.
The patient is in good periodontal health, highly motivated and capable of maintaining good plaque control on his own.

Radiographic exam analysis: tooth 18, 16, 15, 13, 24, 25, 28, 45 and all the lower molars are missing; radiographical appearance of the periodontal health of the remaining teeth. Major bone loss mesially at tooth 17 and 26, probably due to traumatic extractions: in spite of this, healthy supporting periodontal tissues have been maintained at these sites, as confirmed by PPD. There is a space between tooth 33 and 34 in which one more premolar could fit.

Occlusal and functional analysis in MIP: overbite and overjet are absent and the mandible seems to have shifted forward because of the absence of many posterior teeth. The complete lack of masticatory units heavily impairs the masticatory function.

Restoring the patient’s arches according to his MIP would require many teeth to be root canal treated and a lot of supporting bone to be removed for surgical crown lengthening procedures. It would be also very difficult, almost impossible, to find room for the correct amount of restorative materials. Moreover, esthetics of the smile wouldn’t be improved because the position of the upper incisal margins wouldn’t be modified. A centric relation record is needed.
The problem is that the patient’s muscles are tensely contracted so that he hardly opens his mouth while speaking, as the video shows. This condition makes it impossible to register a wax in centric relation.

The patient is required to wear a flat plate for 24 hours. After that his muscles are relaxed and the registration of the centric relation position is possible. The study models are linked together by means of wooden sticks and sticky wax and sent to the lab for mounting on the articulator.

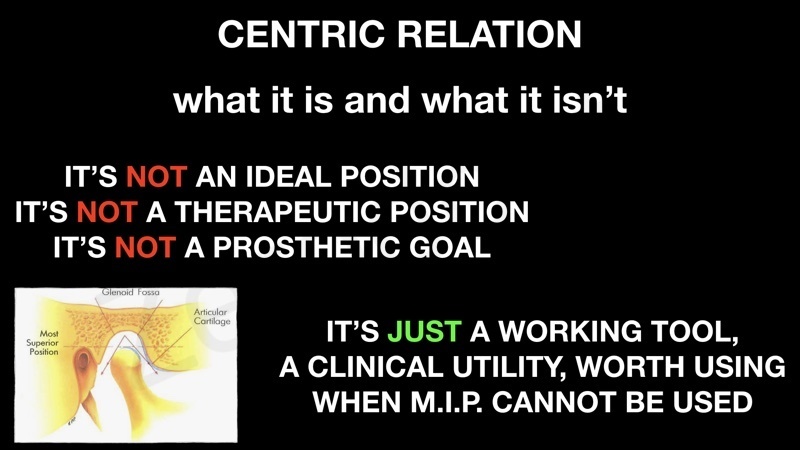
As it always happens in patients with heavily worn teeth, two pre-requisites are necessary to do the treatment planning: 1) increasing the VDO (to get the necessary room for restorative materials, for a more favourable occlusal relationship, to avoid some invasive procedures like preventive endo treatments and finally for a better esthetic outcome); 2) using a reliable position to start from, considering that the patient’s MIP cannot be used as the reference position. This position is the Centric Relation, which is repeatable, can be transferred to an articulator and is physiologically acceptable. It isn’t an “ideal” or “therapeutic” position, it’s only a useful clinical tool.

Now it appears very clear how much the centric relation position changes the perspective of this case: now we have a lot of space to fill in and there are no worries about the type of prosthetic rehabilitation we may choose.
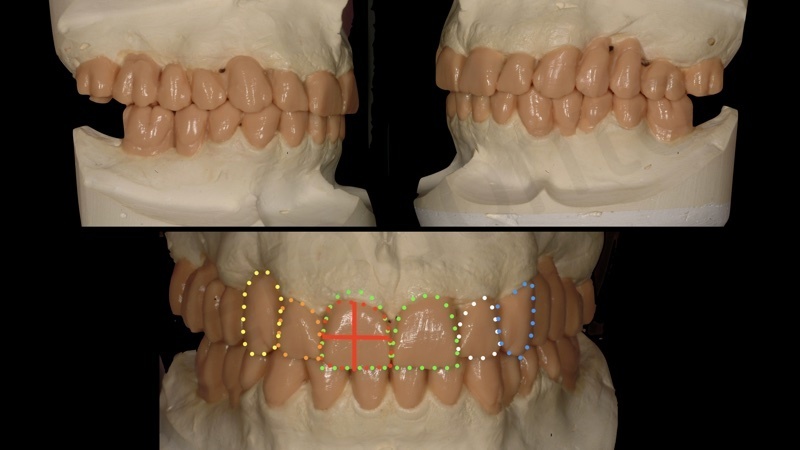
Preliminary wax-up in centric relation position: over-jet and over-bite are re-established and a sufficient number of occlusal units has been achieved in order to fulfill the patient’s functional needs. The esthetic project and outcome will be evaluated with the temporaries in the patient’s mouth.

Treatment planning: tooth 11 is the only one that will be preventively endodontically treated, because of its major sensitivity. All the others, with the exception of 12 and 22, already endodontically treated, are positive to vitality tests. Especially in a case like this, the maintenance of vital teeth is of utmost importance in order to prevent root fractures in the future. Of course maintaining the vitality of the abutment teeth exposes us to the risk of future pulp necrosis, which has a far more favourable prognosis compared to fractures. Surgical crown lengthening will be performed only at the second sextant for improving the retentive ability of the upper anterior teeth. Three implants will be inserted in the sixth sextant. No implants are necessary for the upper arch, where all the remaining teeth need prosthetic reconstruction and they are capable of supporting a full-arch metal-ceramic restoration. No implants are necessary in the fourth sextant: the patient will have a total of six opposing masticatory units, which is more than enough for correct function and occlusal stability. Ridge augmentation of the upper edentulous areas will be performed only if the patient is not happy with the temporary restorations because of food impaction and/or is not able to clean properly.

Preliminary prosthetic preparation and temporary prosthesis in situ, before implant placement in the sixth quadrant and crown lengthening in the second quadrant.

Precision impressions, centric relation waxes for triple check with the split-cast technique, setting of the articulator after pantographic registration. The patient had no complaints during the temporary phase, he could chew efficiently and was happy with his new esthetic appearance. No impairment in plaque control was noticed and all the periodontal parameters were normal at final re-assessment

Final PFM prostheses: occlusal views

Final PFM prostheses: lateral views compared to initial situation

Frontal view, before and after treatment

Patient’s facial appearance after treatment

Patient’s facial appearance when smiling, before and after treatment

Patient’s smile close-up before and after treatment. No digital technologies were used to solve this case. Ceramist Stefano Petreni, CDT
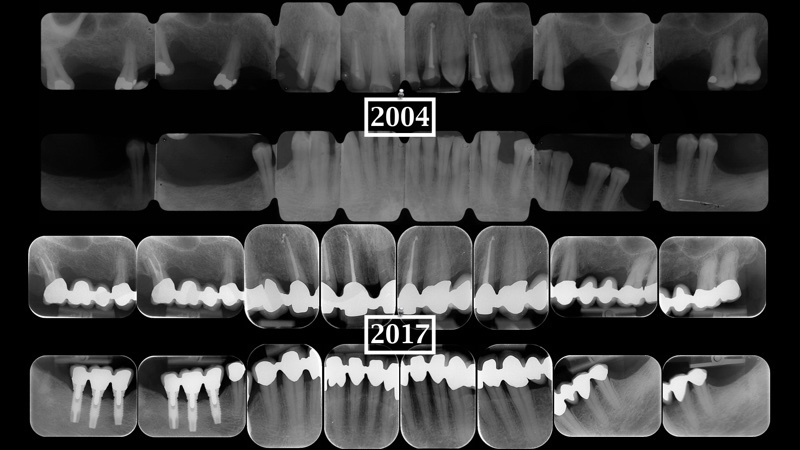
Radiographic exam 13 years after treatment: the only problem encountered in this period was a pulpal necrosis at tooth 17, which had to be endodontically treated in 2011 through a cavity access made in the prosthetic crown.

Clinical situation 13 years after treatment.

