The clinical case we present here regards a 25-year old girl who underwent an extremely severe car accident in which she was the only one survivor out of 4 passengers of the same age.

She was immediately brought to a First Aid/Urgency Surgery and ENT Departments on May 14, 2014 in which, following clinical and radiographic examinations the following lesions were diagnosed:
1) spleen fracture;
2) severe toracic trauma but fortunately without rib fractures;
3) exposed fractures of the right ulna and radium;
4) multiple fractures of the maxillo-facial skeleton, including: a) the right orbit, the nasal bones, the zygomatic buttrress and arch, the maxillary bone (including the loss of teeth 14-13-12-11 and the corresponding alveolar bone, and the palate. The maxilla and the zygoma were heavily displaced upward and outward.
4) multi-focal fracture of the mandible with exposure of the mandibular bone between teeth 43 and 42;
5) contused/lacerated wounds of the upper and lower lip and the face skin.
She was immediately put under general anesthesia and she underwent the following procedures:
1) tracheotomy;
2) total splenectomy
3) reduction and fixation of the ulnar and radial fracturs of the right forearm;
3) “open” reduction and stabilization via an intraoral apporach of the maxillary, zygomatic, nasal fractures, and stabilization with titanium mini and microplates and screws.
4) open reduction and stabilization of the mandibular fractures and fixation with titanium miniplates and screws.
Because of the severe bone loss both in the maxilla and mandible, the surgeons declared that they were not able to properly reposition the maxilla, the zygoma, and the mandible, but just their stabilization.
Post-operative recovery was favorable as regards the general health and the patient was discharged on June 9th, 2014.
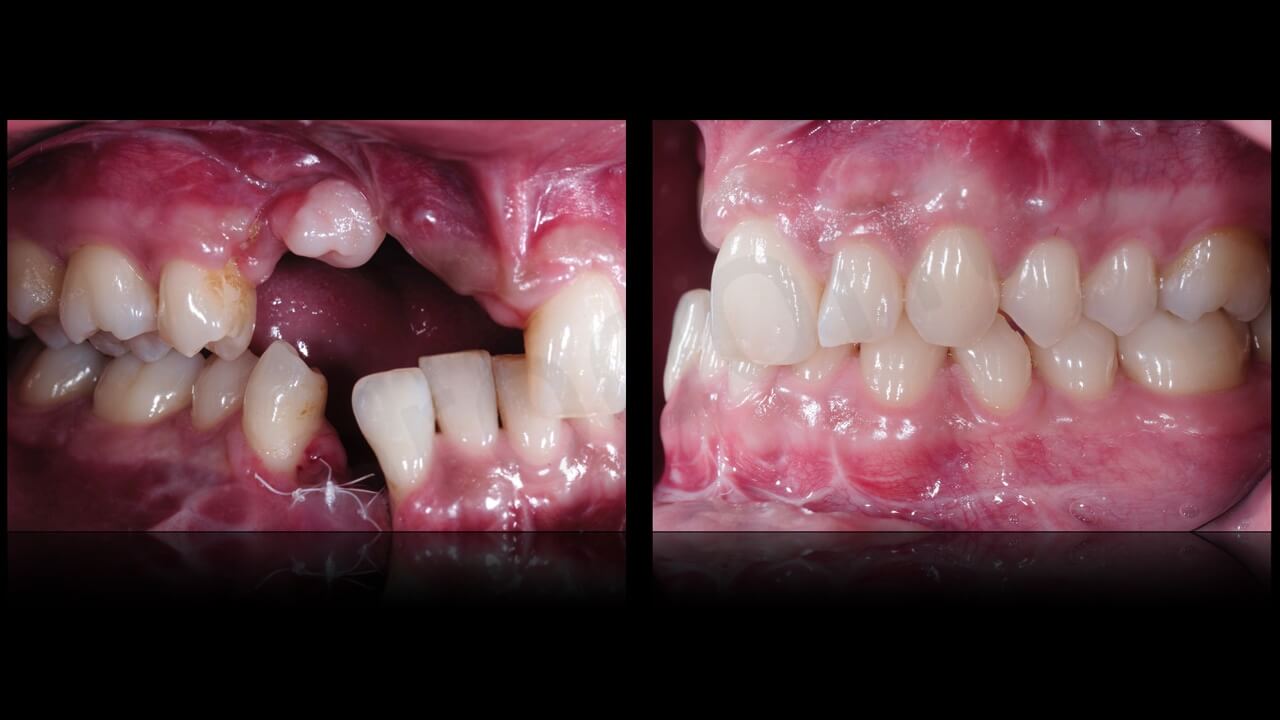
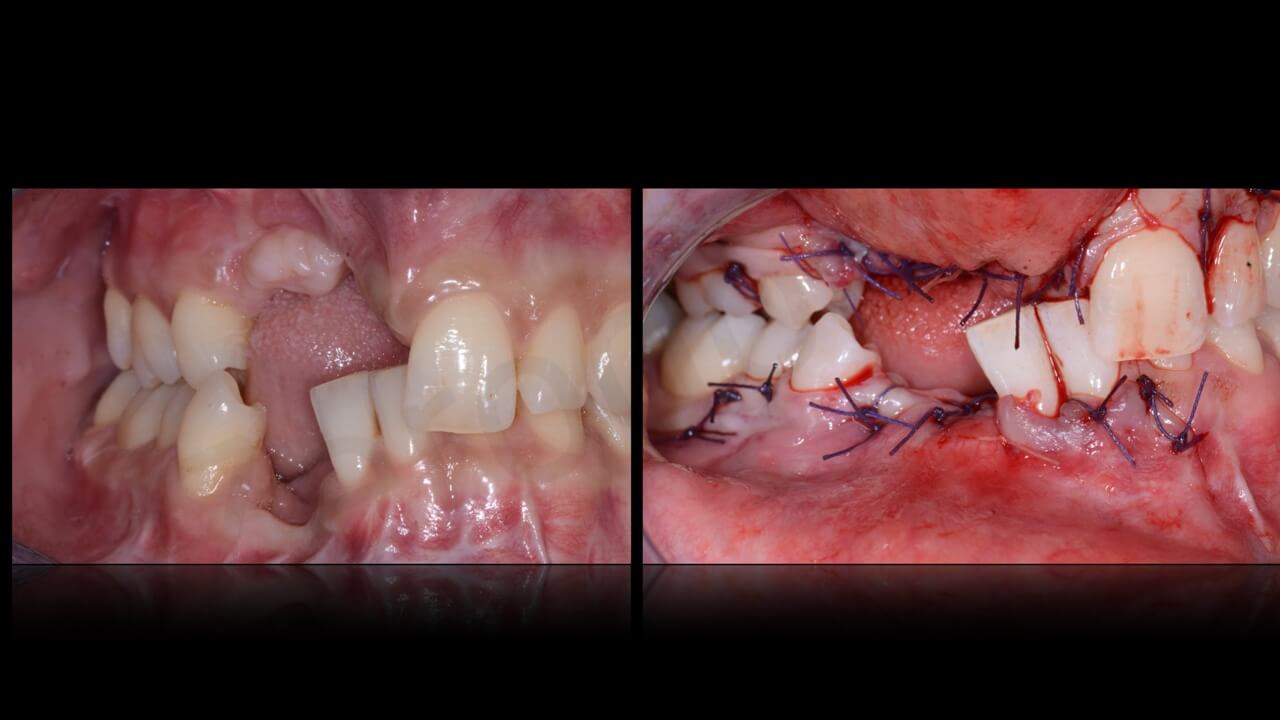
Once healed, however, the patient presented evident sequelae of improper repair of the facial skeleton resulting in complete loss of occlusion on the right side, because of cranial and buccal displacement of the zygomatic-maxillary complex and lingual dispacement of the right hemimandible associted with the formation of a pseudo-arthrosis between teeth 43-42 which were mobile, necrotic, and lost.
The surgeons who first operated the patients were not able to find a solution to restore the pre-trauma situation and the patient was sent for re-evaluation to another maxillo-facial surgeon in Milan, Italy (Prof. Matteo Chiapasco) to evaluate possible solutions.
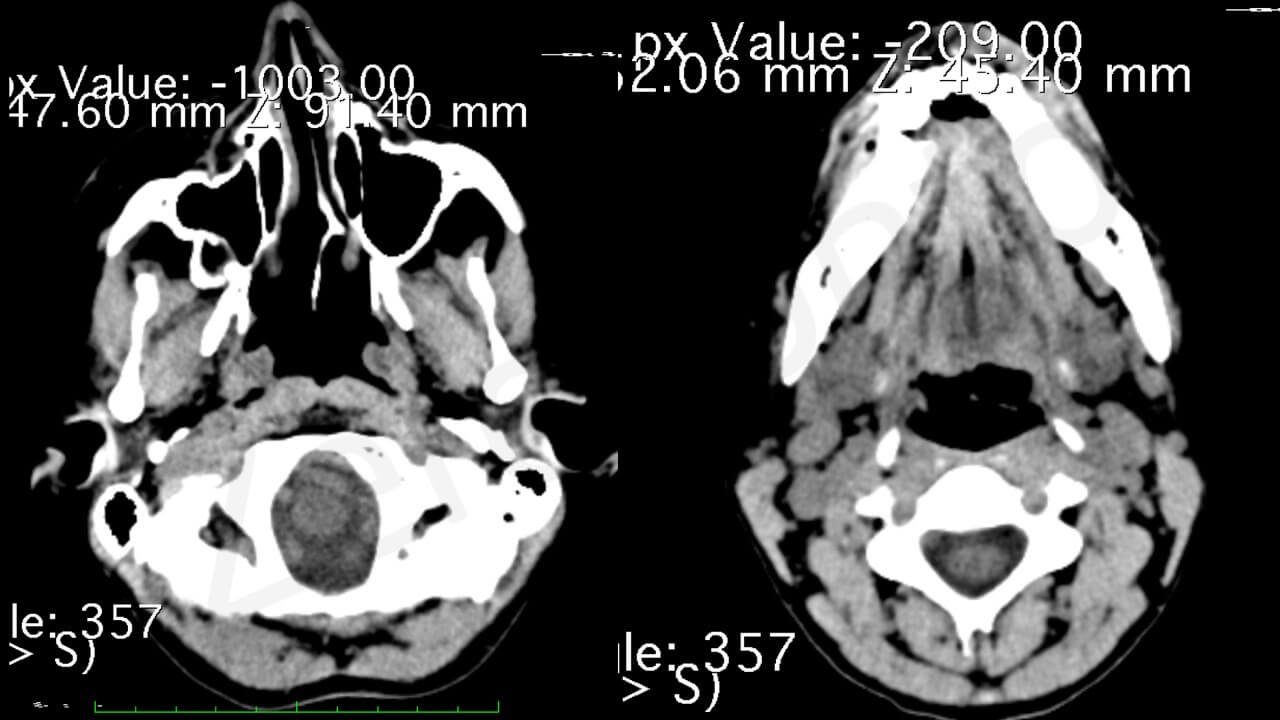
Clinical evaluation and radiographic evaluation with a panoramic radiograph and a CT scan including the whole maxillo-facial skeleton showed a cranialization and buccal displacement of the right emimaxilla including teeth 17-16-15 in association with relevant bone loss of the maxillary bone in the area of the avulsed teeth 14-1-3-12-11.
The right mandible appeared medialized, with lingual inclinitation of the residual dentition and a relevant “step” bewteen tooth 43 and tooth 42 (both mobile and lost) was present


Also, a facial asimmetry with retrusion of the right maxilla, deviation of the mandibular midline, numerous scars of the facial and neck, and a loss of right lip morphology due to improper suturing of the orbicularis muscle was evident.


Patient’s requests were the following:
1) restoration of missing dentition with implant-supported fixed prostheses;
2) correction of lost occlusion;
3) Correction of facial asimmetry.
4) elimination of right upper lip defect
The clinical situation, however, rendered an immediate rehabilitation with implant-supported prostheses unduable, both because of the severe bone loss in the maxilla and mandible, and because of the complete loss of correct intermxillary relationship on the right side.

On August 2014 the patient was sent for consultation to Dr. Piero Venezia, and expert Prosthodontist, c/o the Studio di Odontoiatria Specialistica Cavalcanti-Venezia- (Bari- Italy) to coordinate together with prof. Chiapasco a prosthetically driven rehabilitation including maxillo-facial surgical procedures to repostion and to reconstruct the loss of bone of the maxilla and the mandible, and, in a second stage, implant placement and consecutive prosthetic restoration.
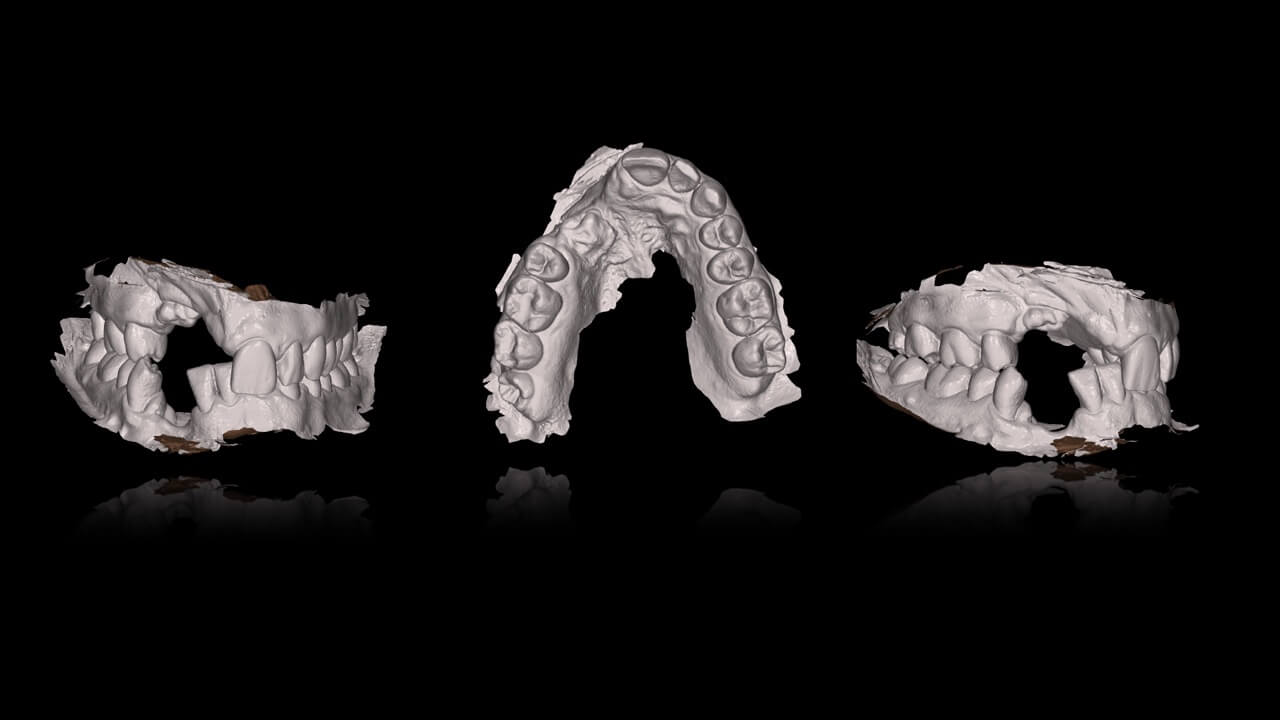
Alginate dental impressions were immediately taken (CAVEX-Holland), as well as a facial bow (UTS 3D– Ivoclar Vivadent – Lichtenstein). The models obtained were sent to a dental laboratory to mount them on an individual articulator (STRATOS 300 – Ivoclar Vivadent – Lichtenstein).
During the same session, teeth 43 and 42 were removed, becasue of severe mobility and th presence of their roots embedded in the pseudo-arthrotic tissue between the right and left, non-consolidated mandible.
Finally, the patient was inserted in a periodic recall program for periodontal preparation and therapy.
In the following session, new impressions were taken with individual impression trays to fabricate a temporary removable provisional to reduce masticatory and esthetic discomfort .
 Based on a new set of model casts obtained by polyether impressions (3M-Espe) assembled on an individual articulator with the aid of a facial bow, Dr. Venezia and prof. Chiapasco were now able to evaluate in the proper way the severe malocclusion following the malposition of the previously fractured maxillary and mandibular bone segments.
Based on a new set of model casts obtained by polyether impressions (3M-Espe) assembled on an individual articulator with the aid of a facial bow, Dr. Venezia and prof. Chiapasco were now able to evaluate in the proper way the severe malocclusion following the malposition of the previously fractured maxillary and mandibular bone segments.
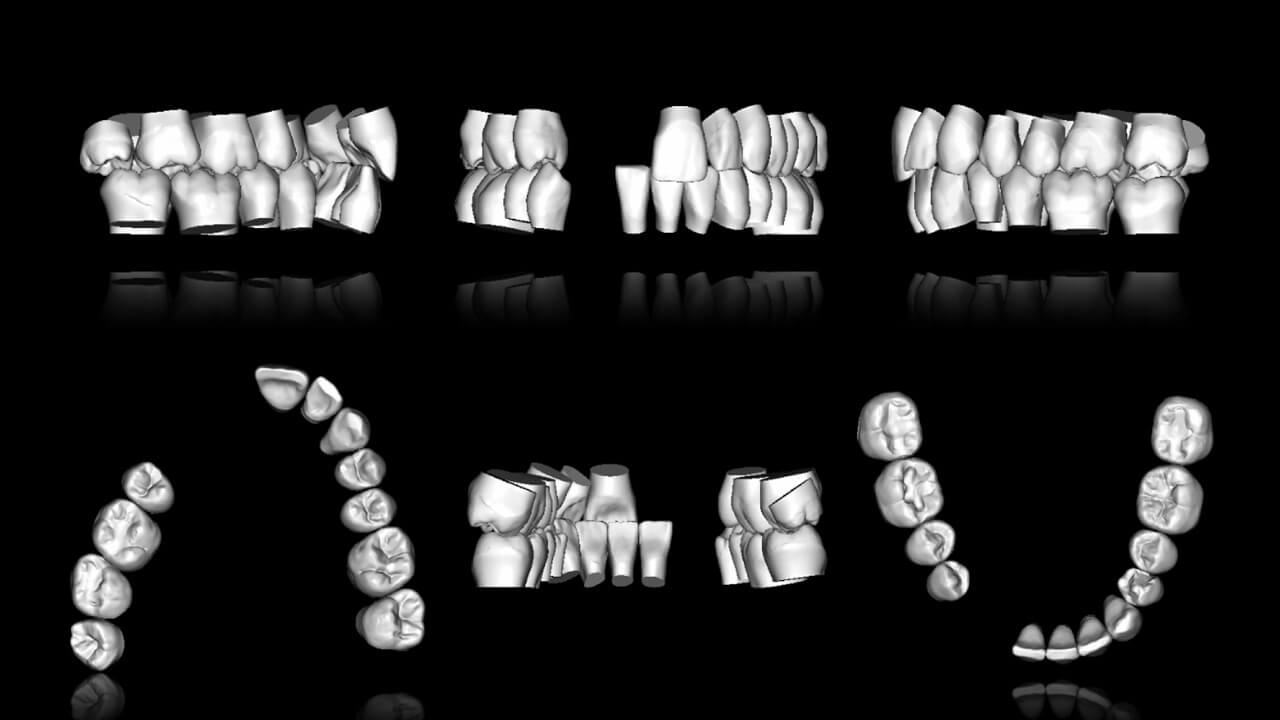
A pre-operative set-up was then performed by positioning the missing dentition in the right position (taking as a reference point the opposing site of the occlusion which was luckily not modified by the trauma and was still in its original, class I occlusion).
On the base of this pre-visualization, it was now possible to simulate the bone skeleton changes of the displaced fragments and the reconstructive procedures necessary to reconstruct the missing bone, following the nowadays well consolidated principle of a prosthetically driven bone reconstruction planning.


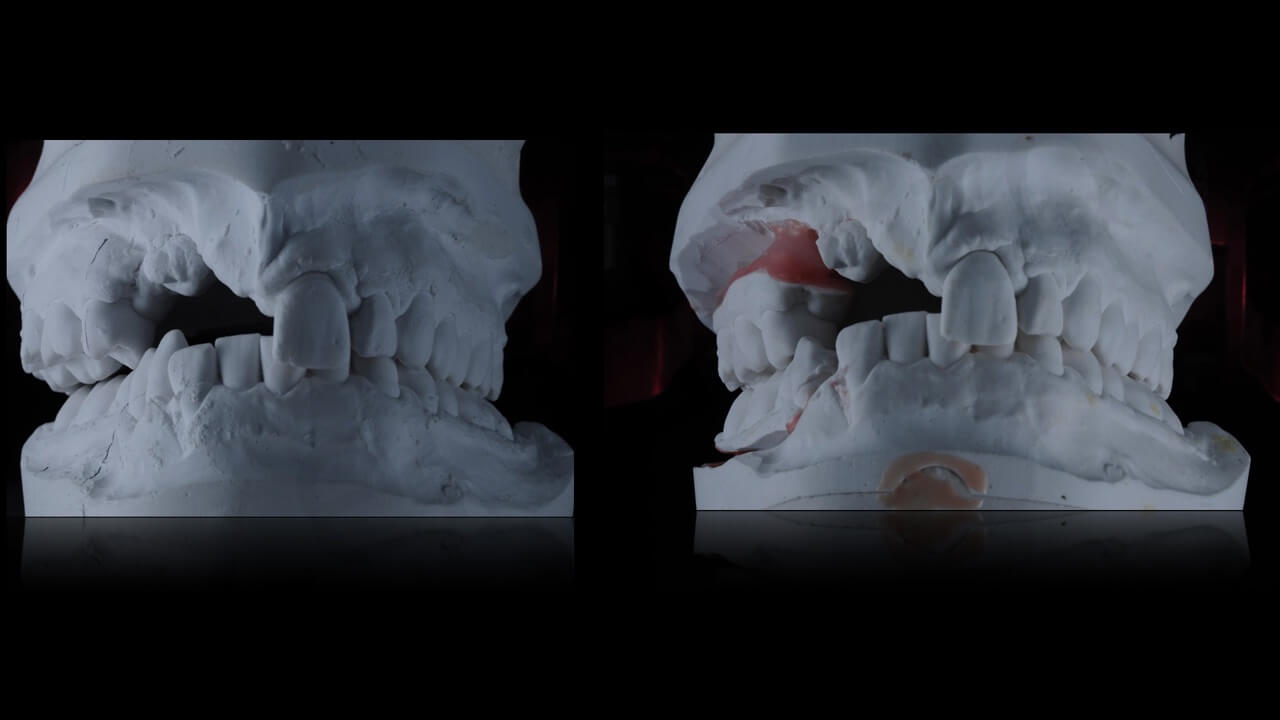
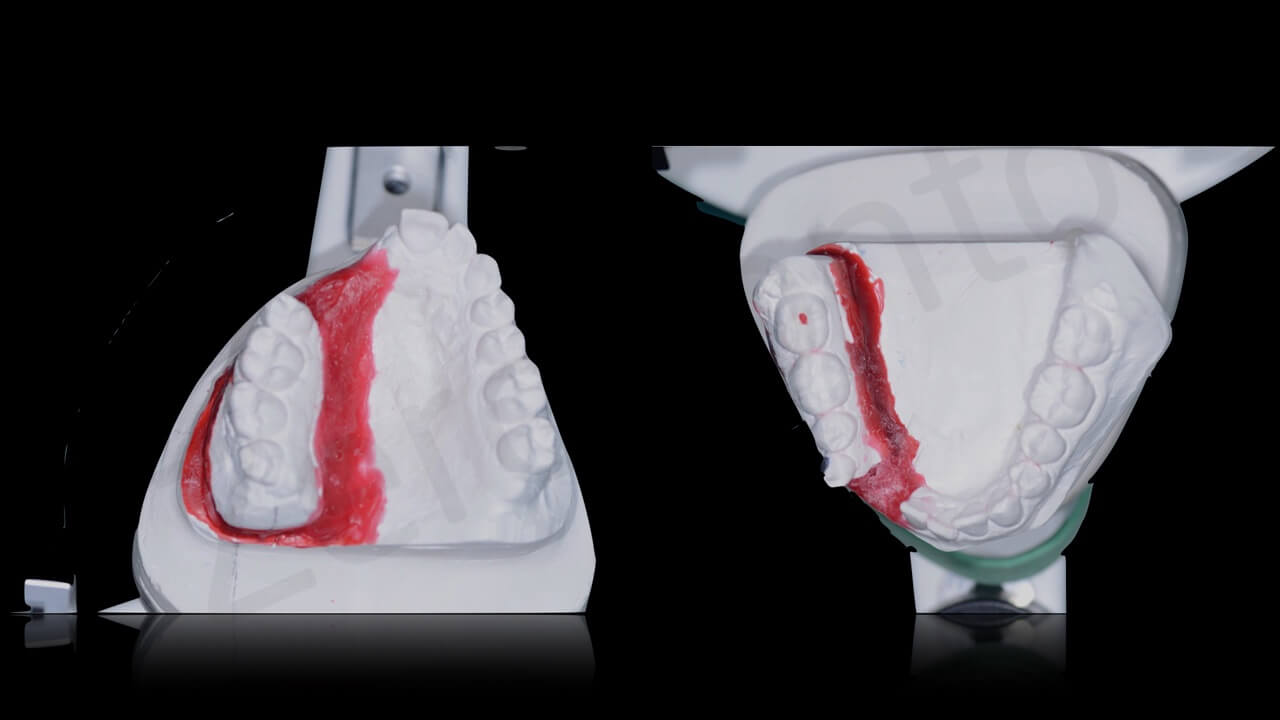
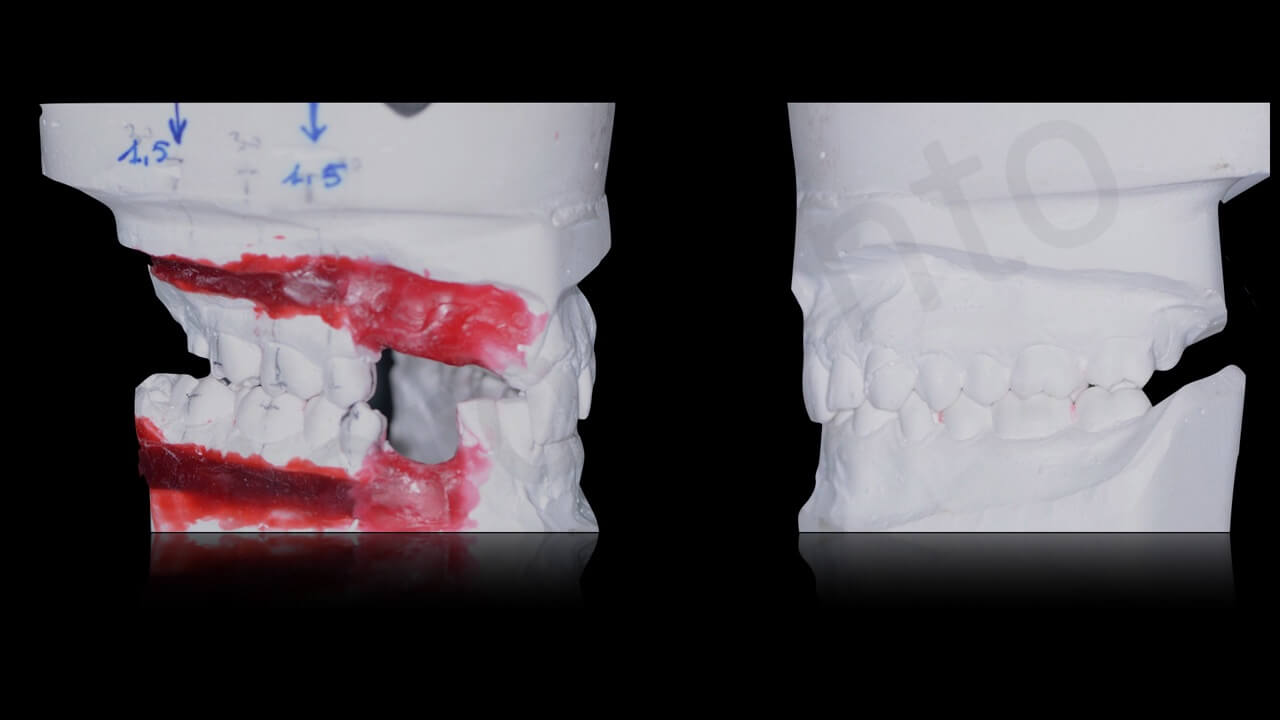
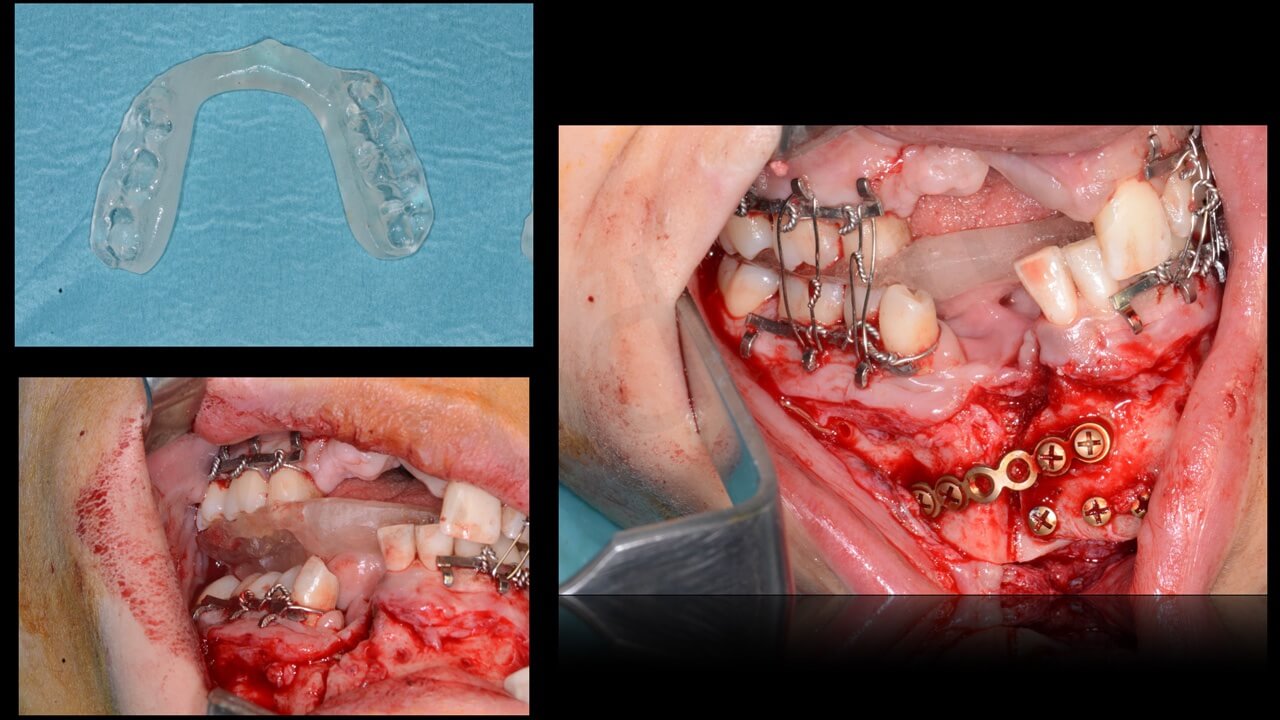
 On a duplicate of the casts, a surgical intermediate splint was fabricated in order to simplify surgical repositionnig of the mandible (first) and, then, a second surgical splint to guide the final position of the osteotomized maxillary segment in the final, right position, following the typical principles and procedures of of orthognatic surgery.
On a duplicate of the casts, a surgical intermediate splint was fabricated in order to simplify surgical repositionnig of the mandible (first) and, then, a second surgical splint to guide the final position of the osteotomized maxillary segment in the final, right position, following the typical principles and procedures of of orthognatic surgery.
A detailed explanation of the surgical and prosthetic steps were described to the patient and summarized as follows:
1) surgical repositioning of the maxillary and mandibular segments to re-create adequate intermaxillary relationships (at present totally modified by the trauma sequelae)
2) surgical reconstrucion of the maxillo-mandibular bone loss with the use of autogenous iliac bone grafts;
3) re-alignment of residual dentition with orthodontic treatment;
4) endosseous implant placement once bone grafts were adequately integrated;
5) reconstruction of lost soft tissues (mucoda and keratinized mucosa) in the edentulous areas by means of connective and epithelial auogenous grafts (taken from the palate) and xenogenic collagen matrixes;
6) provisional prosthetic restoration;
7) final prosthetic restoration.
The patient was thoroughly informed as regards all these steps, including, postoperative morbidity, potential risk of partial or total failure of the surgical procedures, necessity of modifying the initial plan during the restoration according to the real results.
An informed consent including all these details was delivered read and signed by the patient.
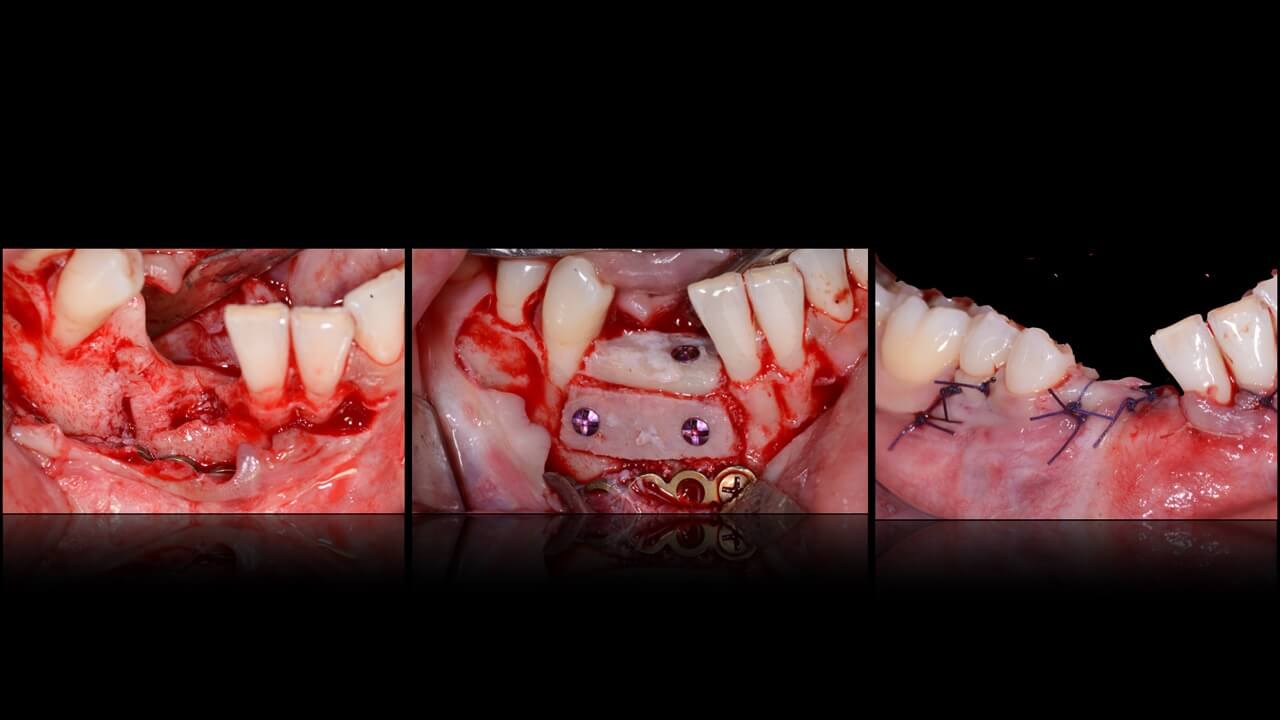
Step 1
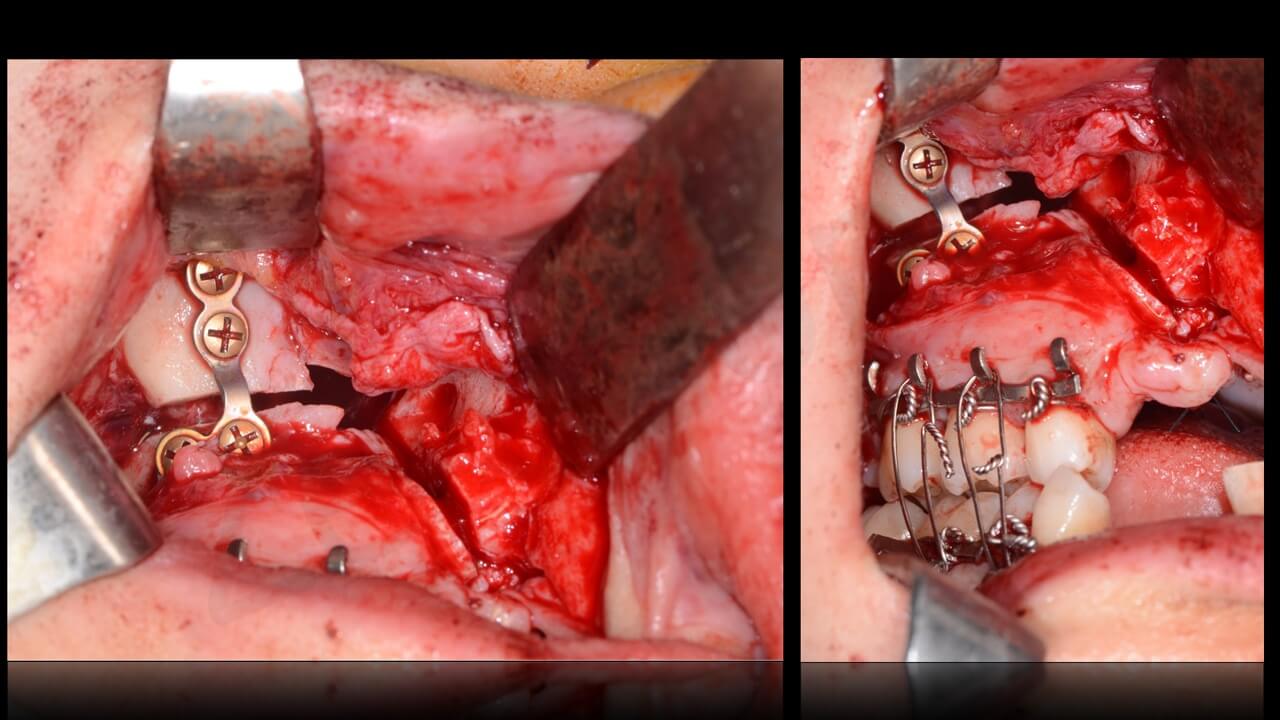
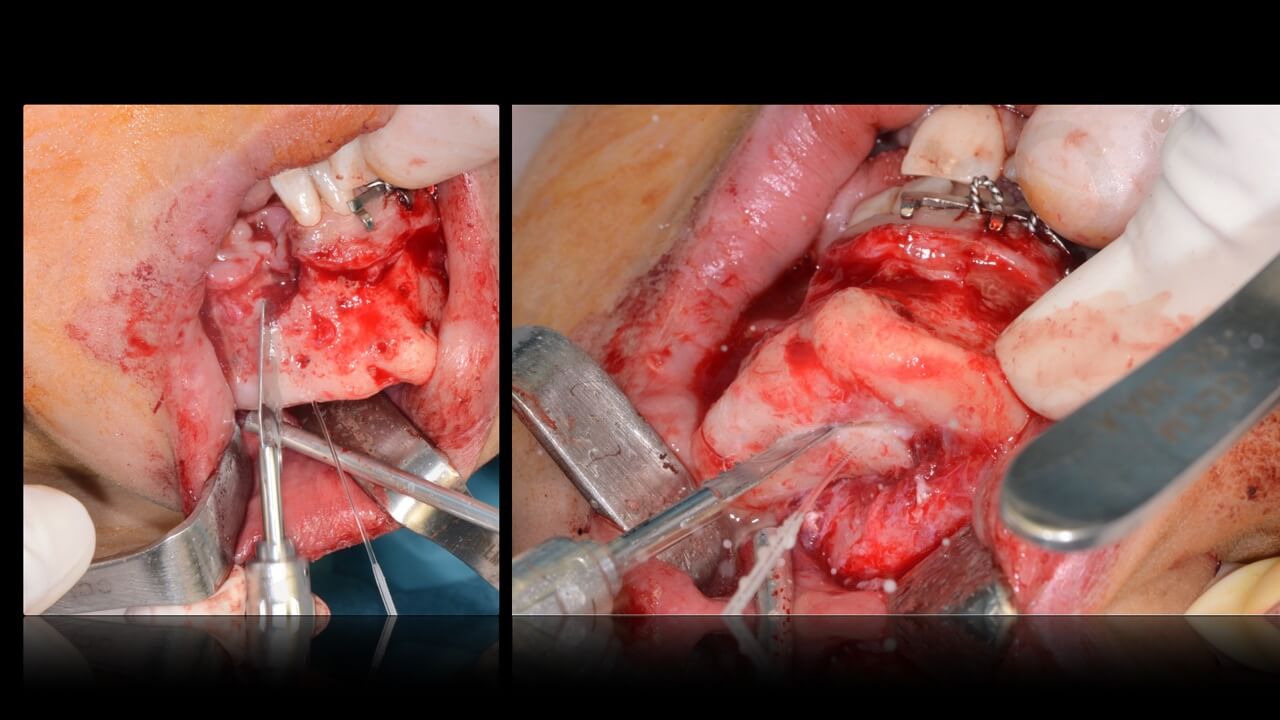
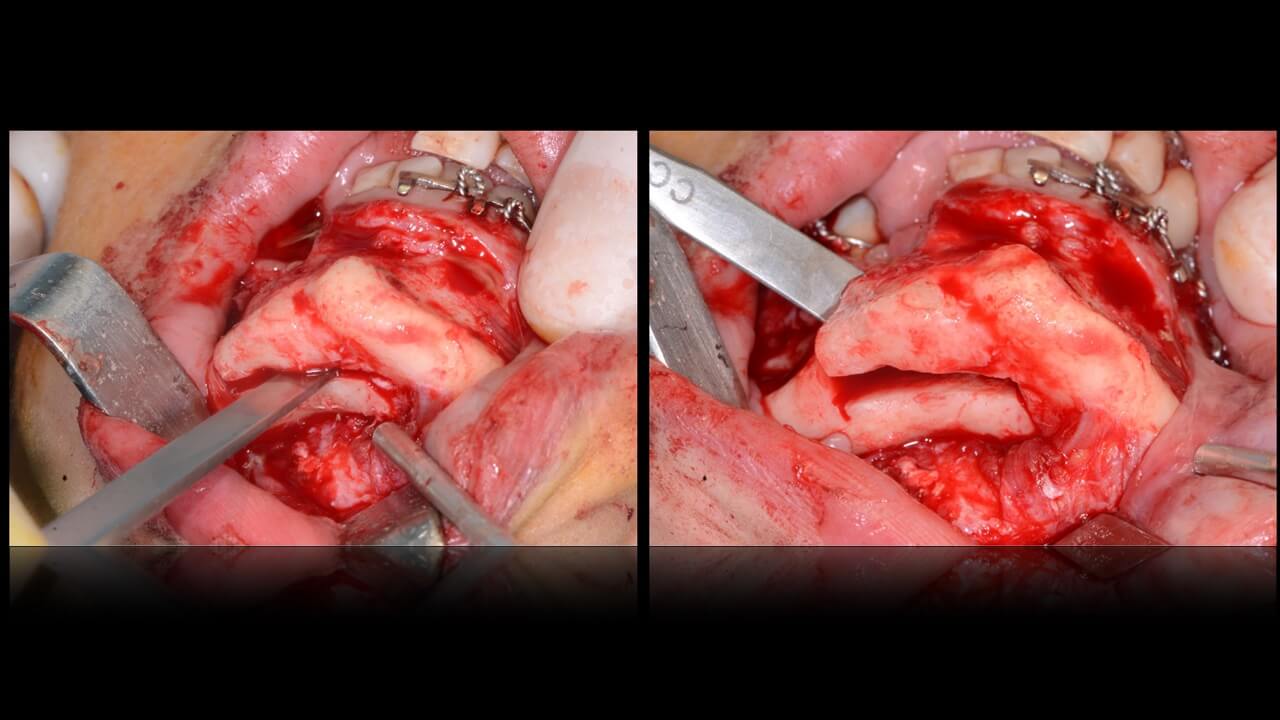
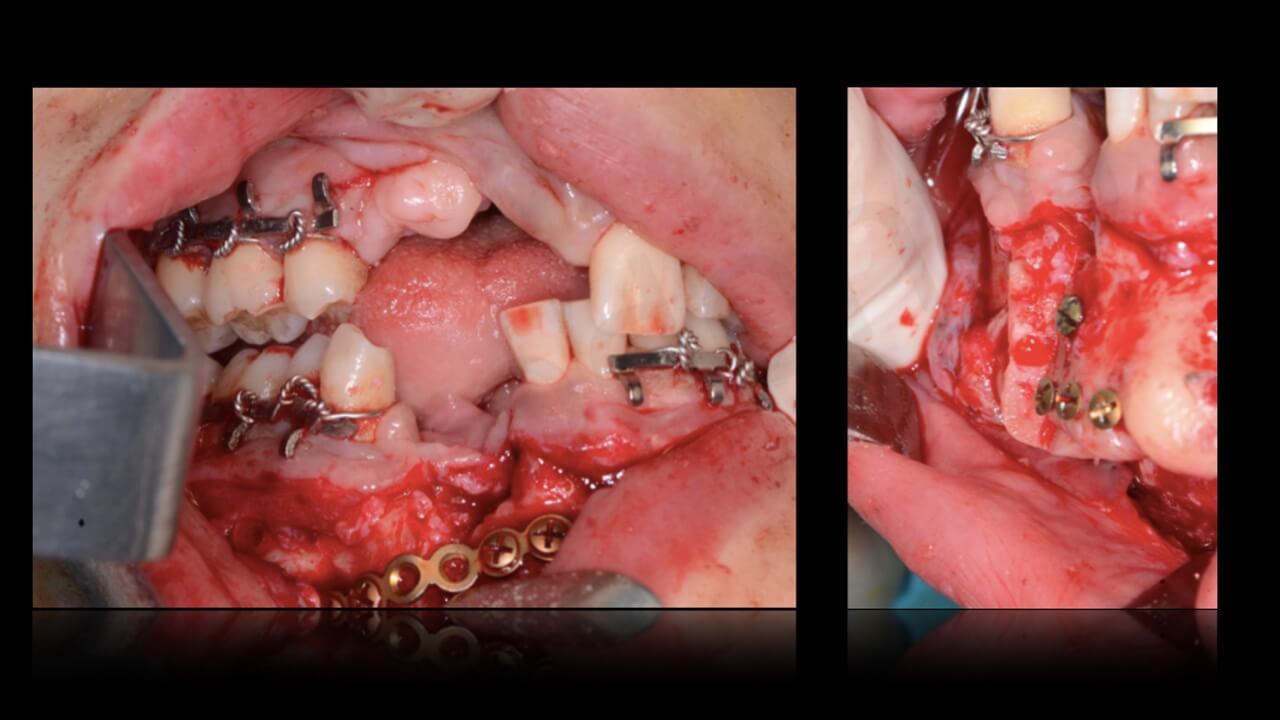
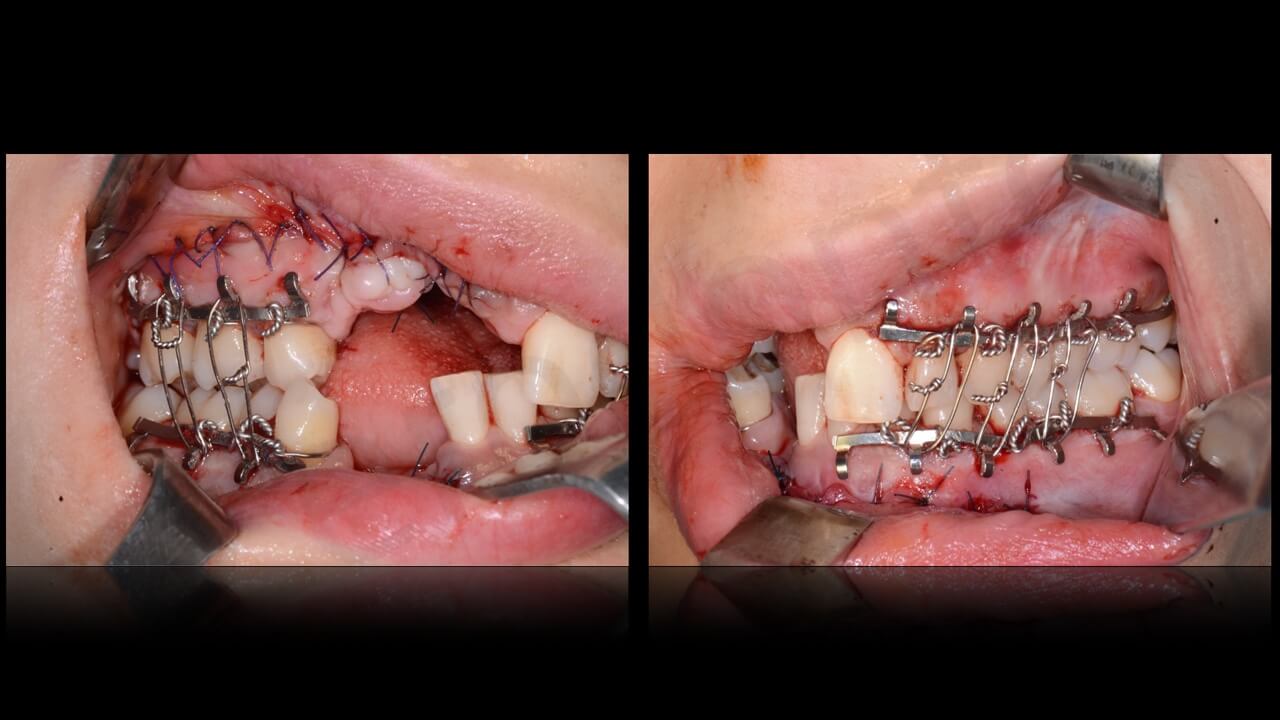
The first step consisted of a surgical procedure performed under general anesthesia on January 2015 with naso-tracheal intubation. It consisted of dento-alveolar osteotomies of the posterior maxilla and mandible in order to re-create normal intermaxillary relationships. More in detail, the posterior maxilla was osteotomized and repositioned coronally and medially, while the posterior mandible was osteotomized andreposioned caudally and buccally, until a normal intermaxilalry elationship was obtained. Finally, the osteotomized segments were stabilized with titanium plates and screws using as a reference for final position the pefabricated resin stent.
 At the same time, the deficit involving soft tissues of the right upper lip was corected with a lipofilling technique.
At the same time, the deficit involving soft tissues of the right upper lip was corected with a lipofilling technique.
After this surgery, intermaxillary relationships were restored, but the relevant bone defect involving both the anterior maxilla and mandible in association with the lack of teeth 14-13-12-11,43-42 was of course still present.
As a complicating factor, the lack of teeth 42 and 43 was followed by a distal linclination of the residual incisors toward the still present bone defect.
Post-operatove recovery was uneventful, two weeks later sutures were removed, while the intermaxillary block was maintained for another two weeks.
Two months later, new impressions were taken and new removable provisionals were fabricated to improve patient’s comfort.
All the following steps consisiting of a multidisciplinary planning including prosthetics, orthodontics, and surgery was performed according to a digital flow. The orthodontic planning and treatment was performed by Dr. Emilia Casiello, Bari, Italy; the prosthetic part was followed by Dr. Piero Venezia; the periodontal management including recostruction of lacking soft tissues by dr. Raffaele Cavalcanti, Bari, Italy; and, finally, the bone reconstructive phase as well as implant placement by prof. Chiapasco, Milano, Italy,
On May 2015, a digital scanning with a dedicated software (True Definition Scanner – 3M U.S.A.) of the maxillary and mandibualr arches and the new intermaxillary relationships was performed.
The “virtual” model was superimposed on the 3-D radiologic reconstruction of the facial skeleton with a dedicate software (Co-Diagnostix – Dental Wings – Canada). This procedure allowed to evaluate tridimensionally the bone defect, in particualr in realtion with the future prosthetic needs. This procedure allowed us to obtain a precise pre-visualization of the whole procedure.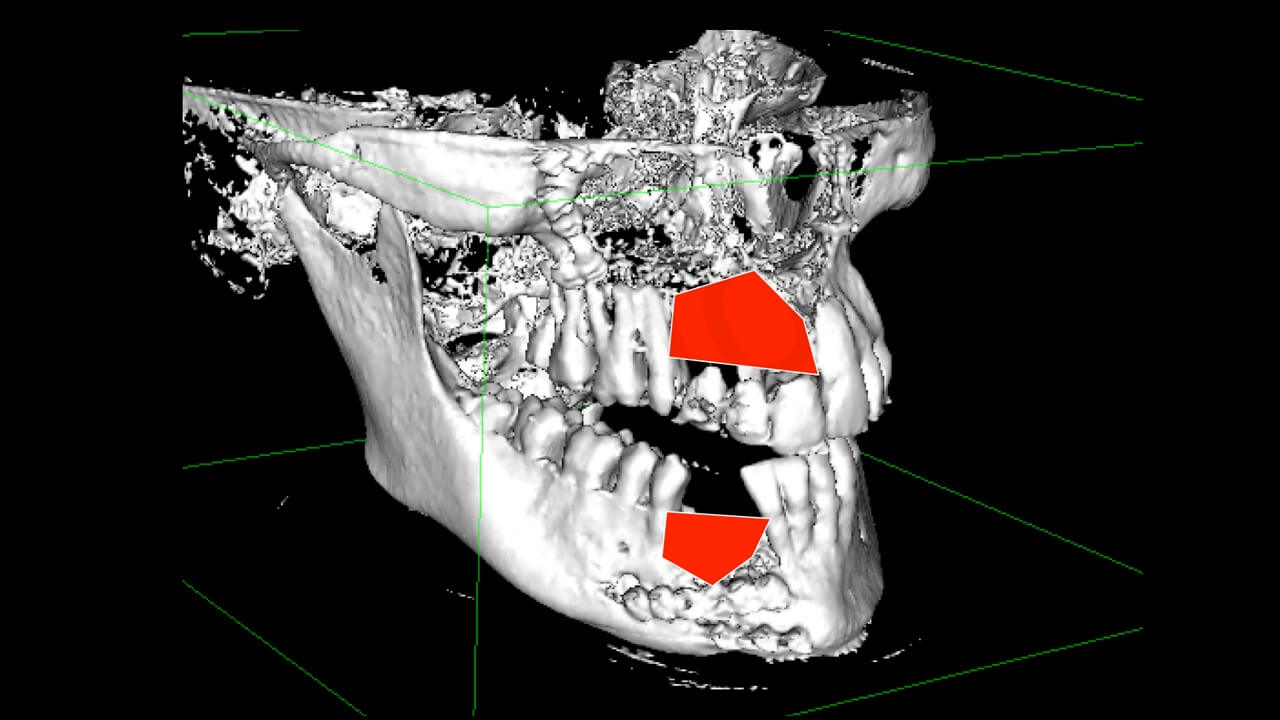
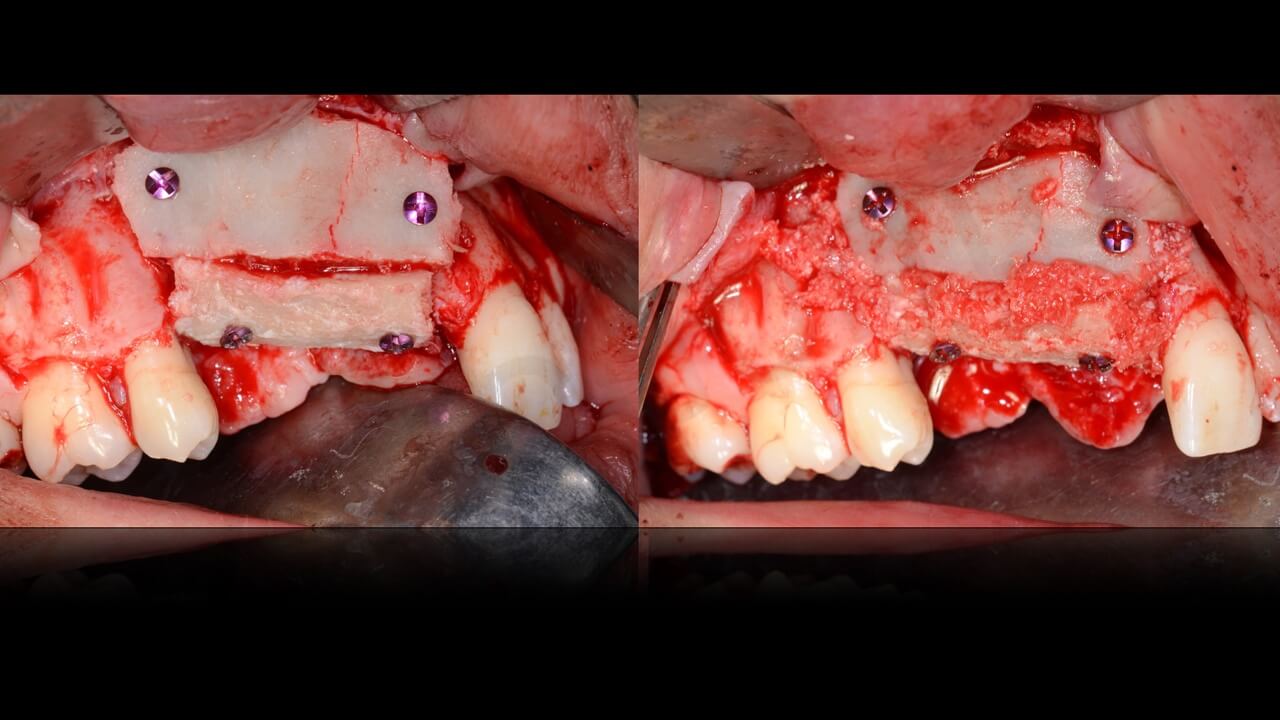
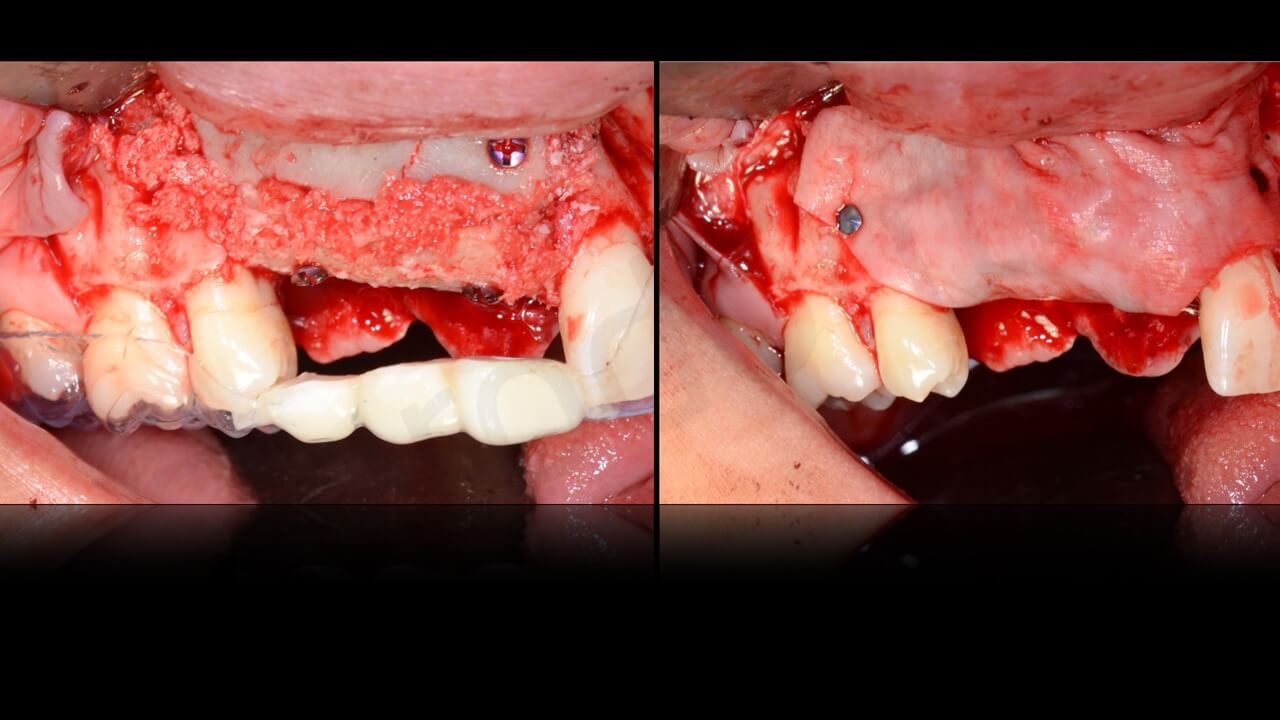
Step 2
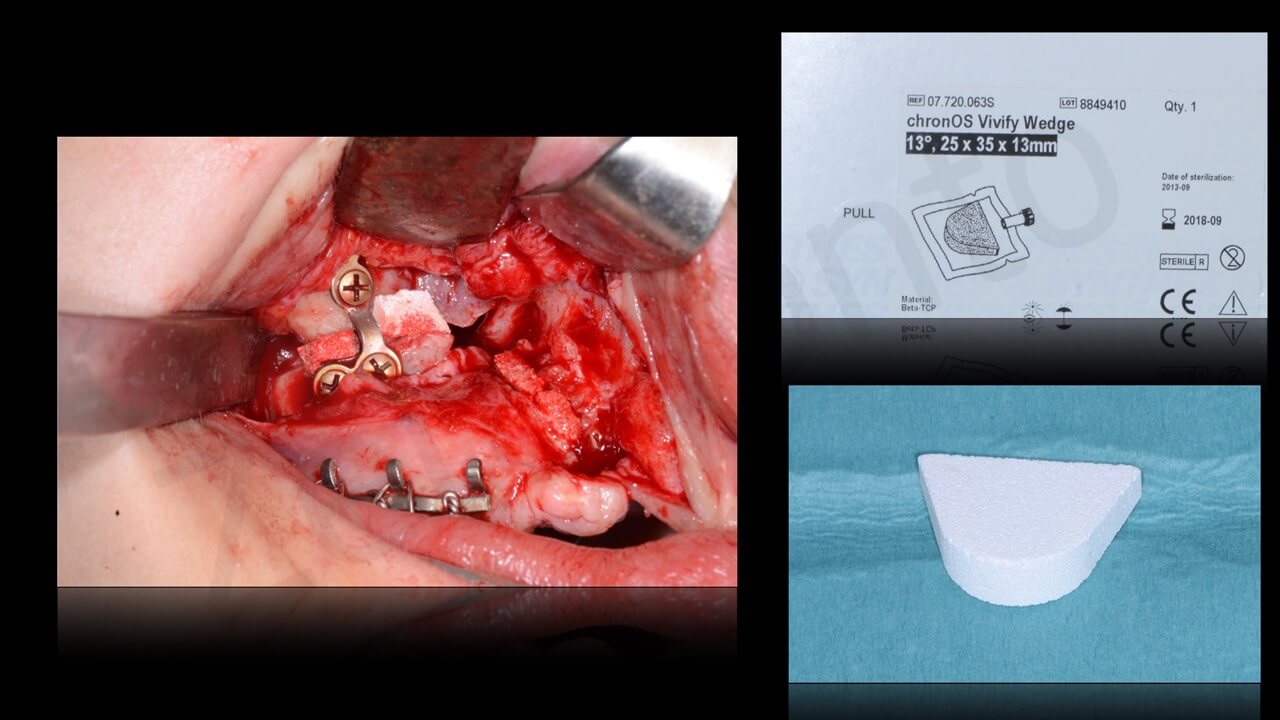
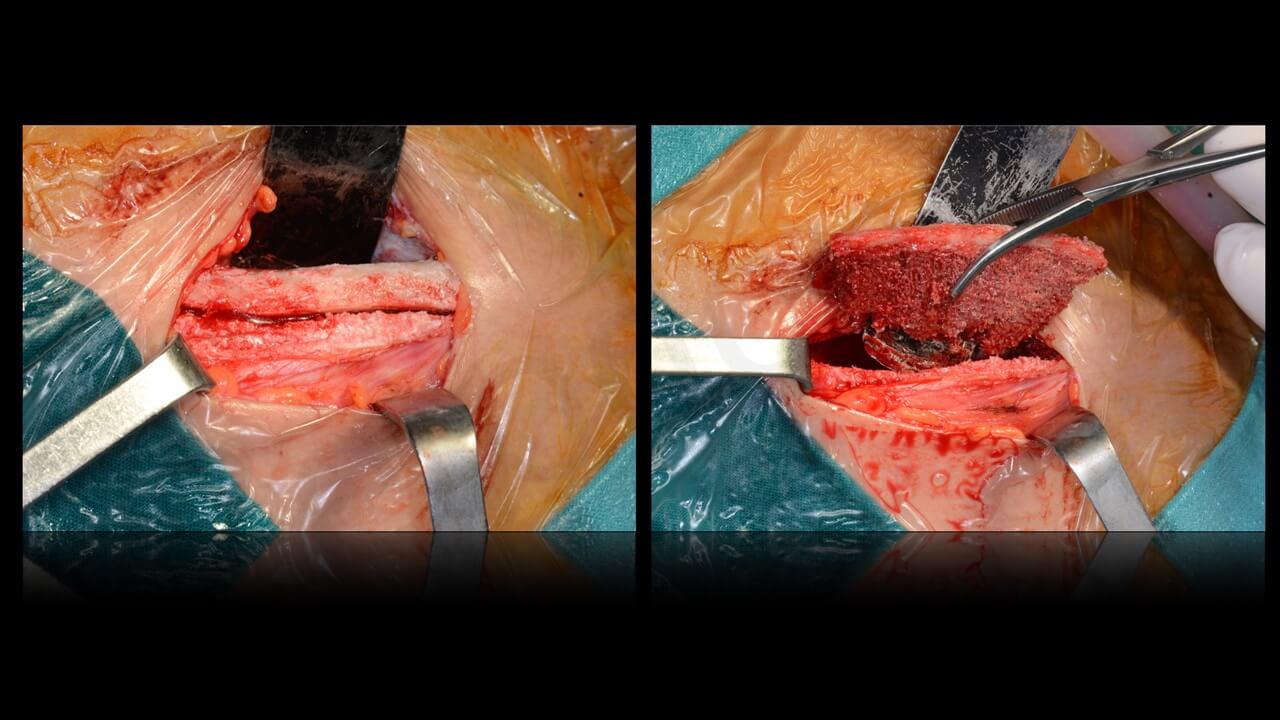
On July 2nd, 2015, the patient was once more put under general anesthesia with naso-tracheal intubation to perform the reconstrucitve phase.
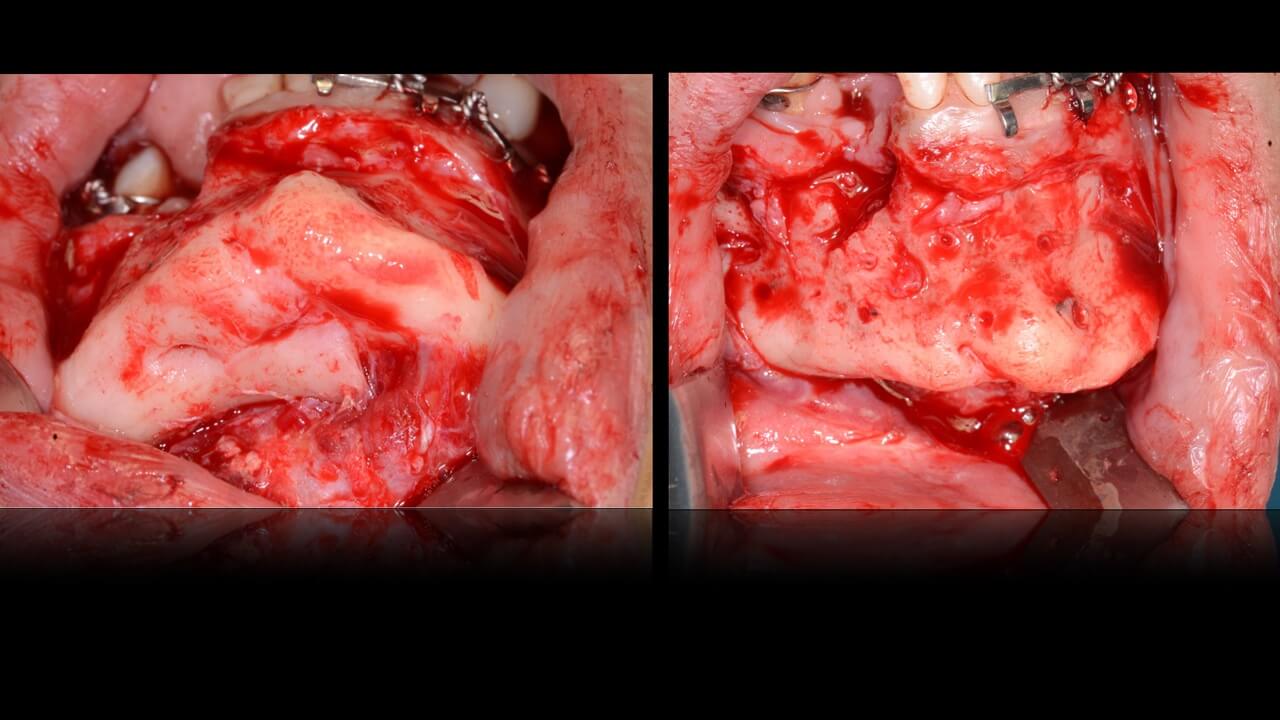
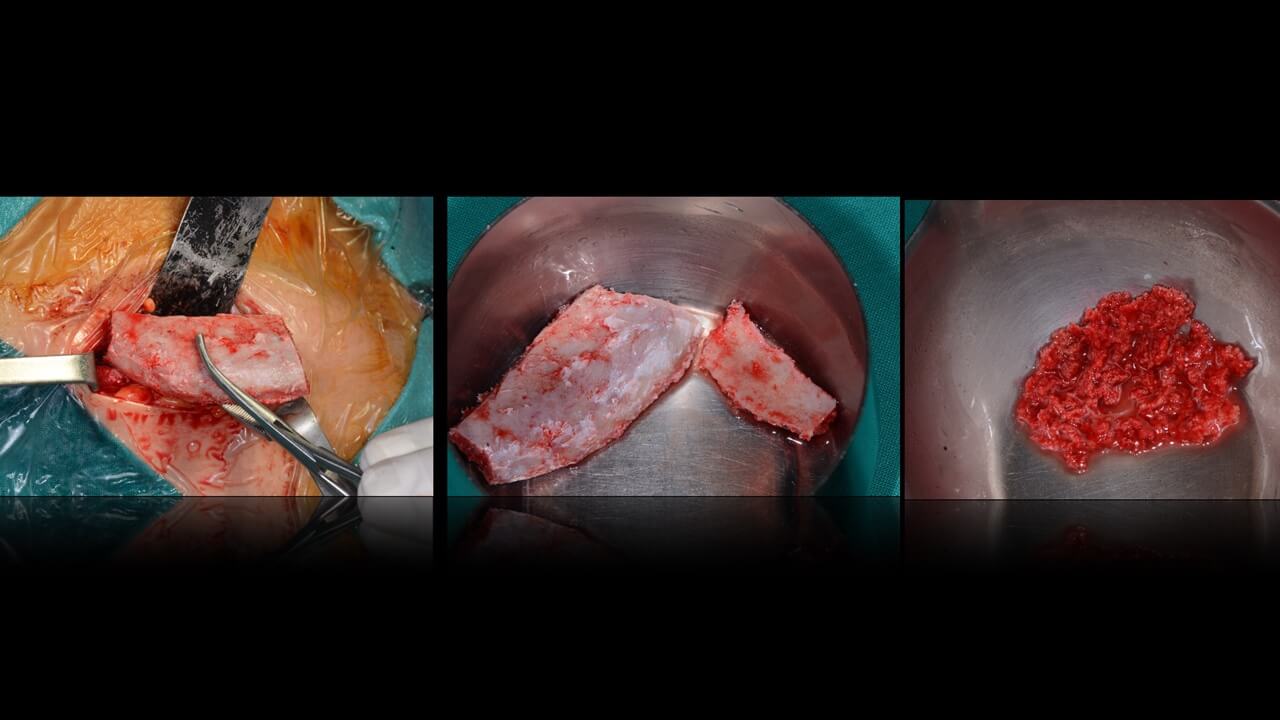
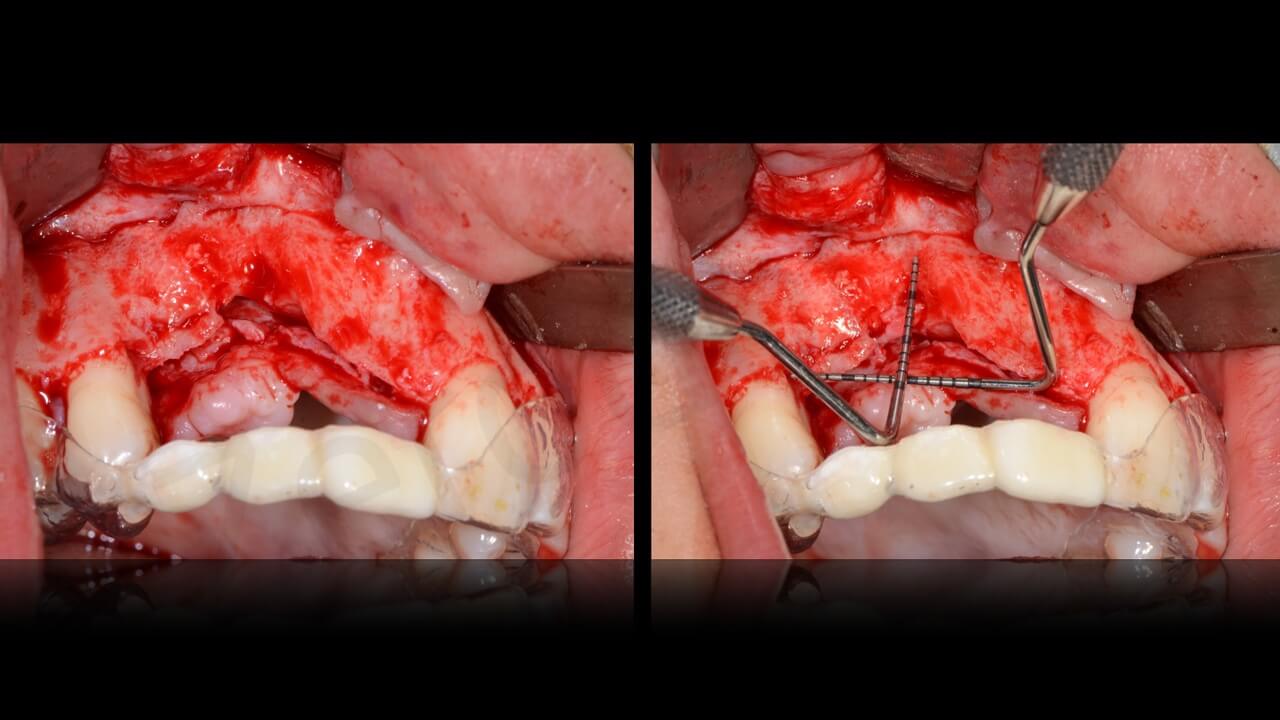
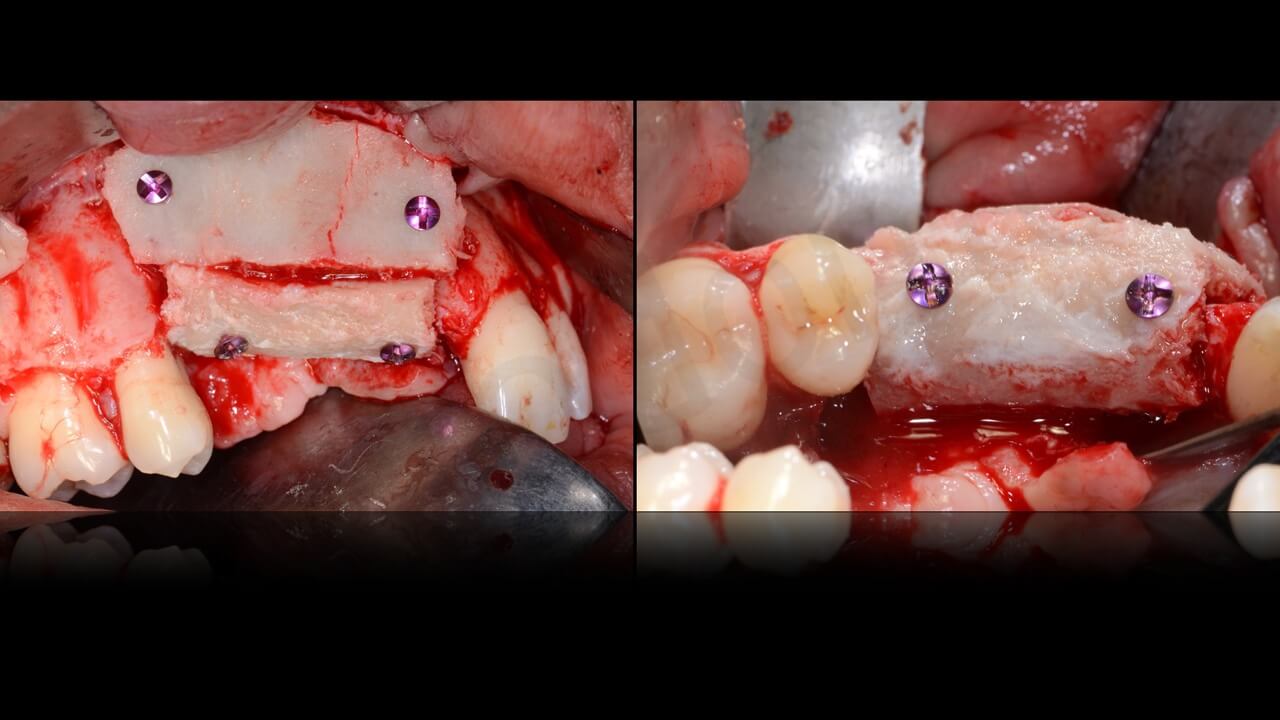
This latter (performed by prof. Chiapasco) consisted of a bone harvesting procedure from the anterior right iliac crest in order to obtain 4 blocks of bone to reconstruct both the maxillary and mandibular defects with onlay vertical and horizontal grafts. Bone blocks were fixated with titanium plates and screws and grafts wee covered with local flaps adequately released to obtain a tension-free, water-tight suture.
Post-operative recovery was once more uneventful and sutures were removed 2 weeks later.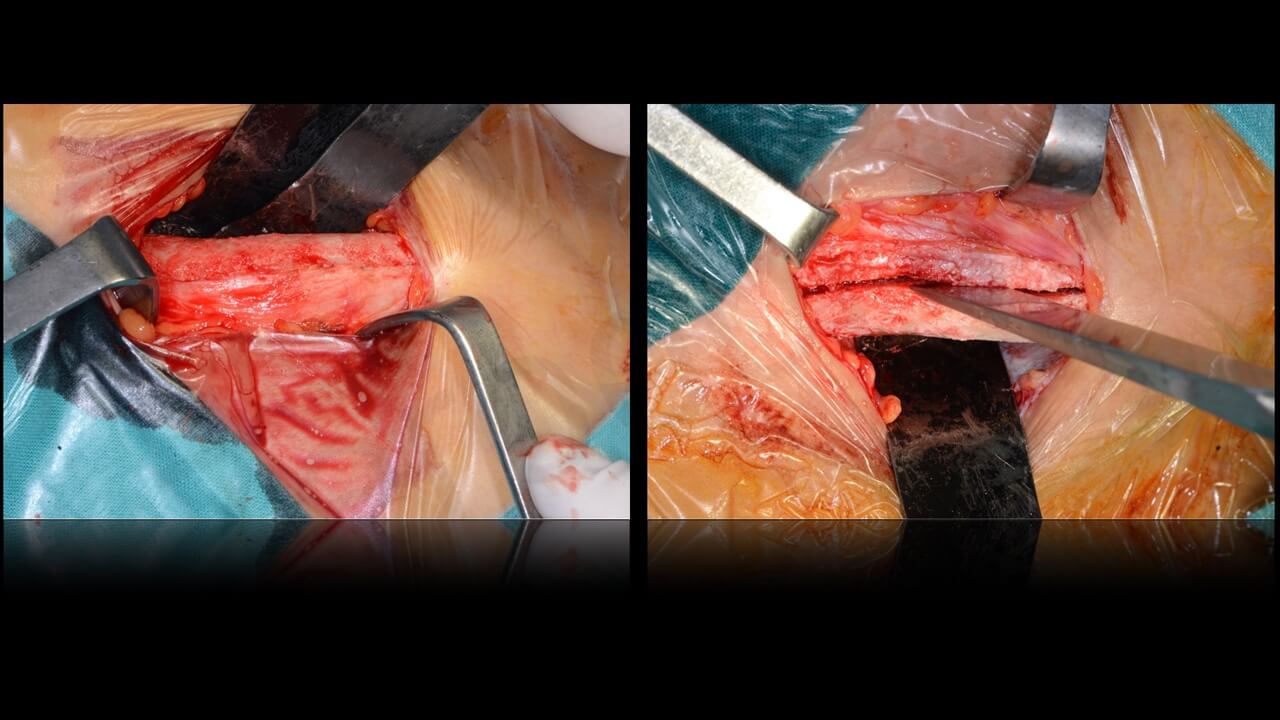

 A comparison between pre and post-operative appearance of patient’s facial profile clearly shows the major improvement obtained (still without dentition)
A comparison between pre and post-operative appearance of patient’s facial profile clearly shows the major improvement obtained (still without dentition)


 Thanks to digital analysis, it is also possible to compare the major changes obtained after the bone reconstructions.
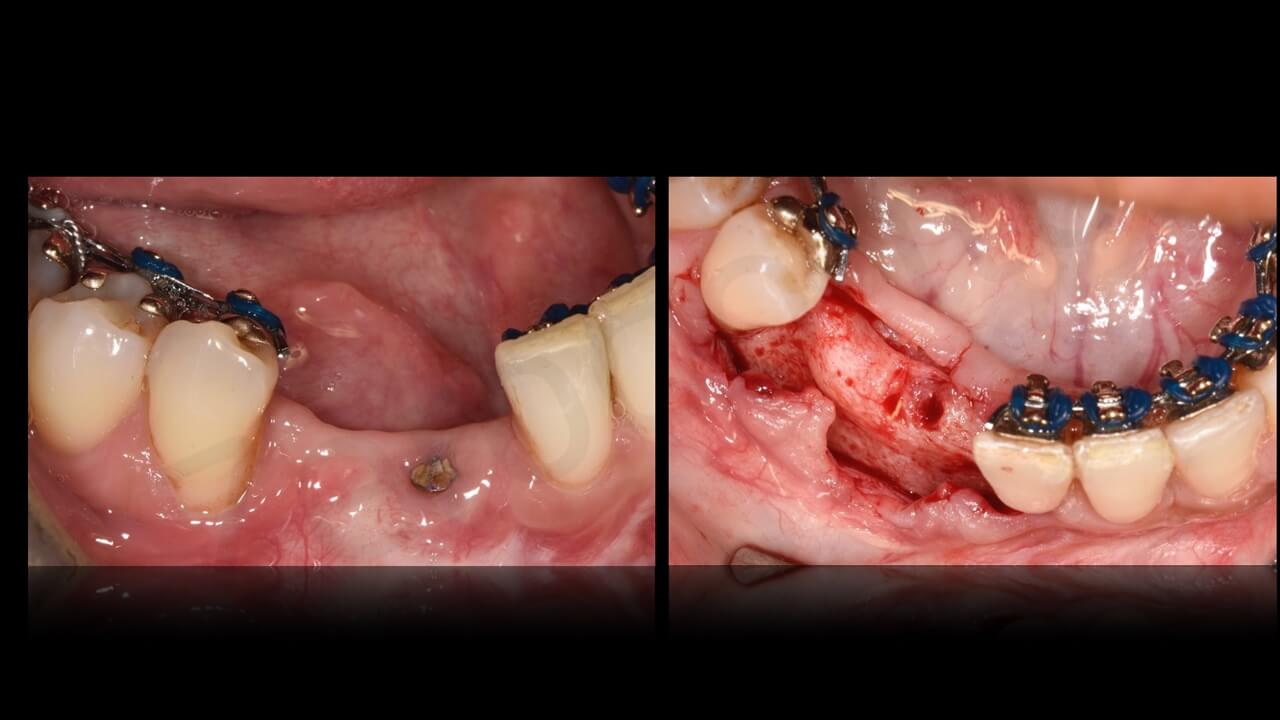
Thanks to digital analysis, it is also possible to compare the major changes obtained after the bone reconstructions. 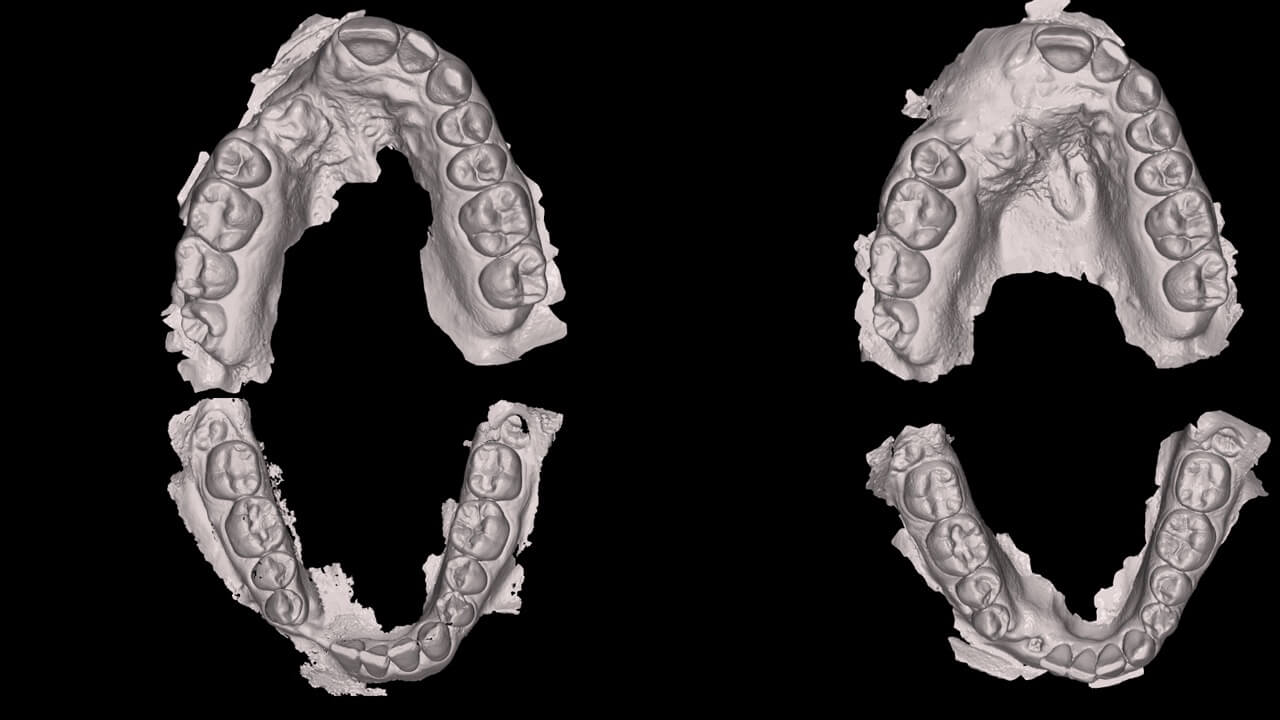 During the integration of the bone grafts, the orthodontic treatment was started (September 2015). The main goal was twofold: 1) the correction of the axis of central and lateral mandibular incisors, which, after the removal of teeth 43 and 42 underwent a relevant inclination towards the reconstructed, edentulous area; 2) to create adequate room for placement of 2 implants substituting the missing teeth.
During the integration of the bone grafts, the orthodontic treatment was started (September 2015). The main goal was twofold: 1) the correction of the axis of central and lateral mandibular incisors, which, after the removal of teeth 43 and 42 underwent a relevant inclination towards the reconstructed, edentulous area; 2) to create adequate room for placement of 2 implants substituting the missing teeth.
Preoperative orthodontic planning was performed only by means of a digital software (True Definition Scanner – 3M- U.S.A.) by Dr. Emilia casiello (Bari, Italy) with a new intraoral scan and recording of occlusal situation in the area to be treated.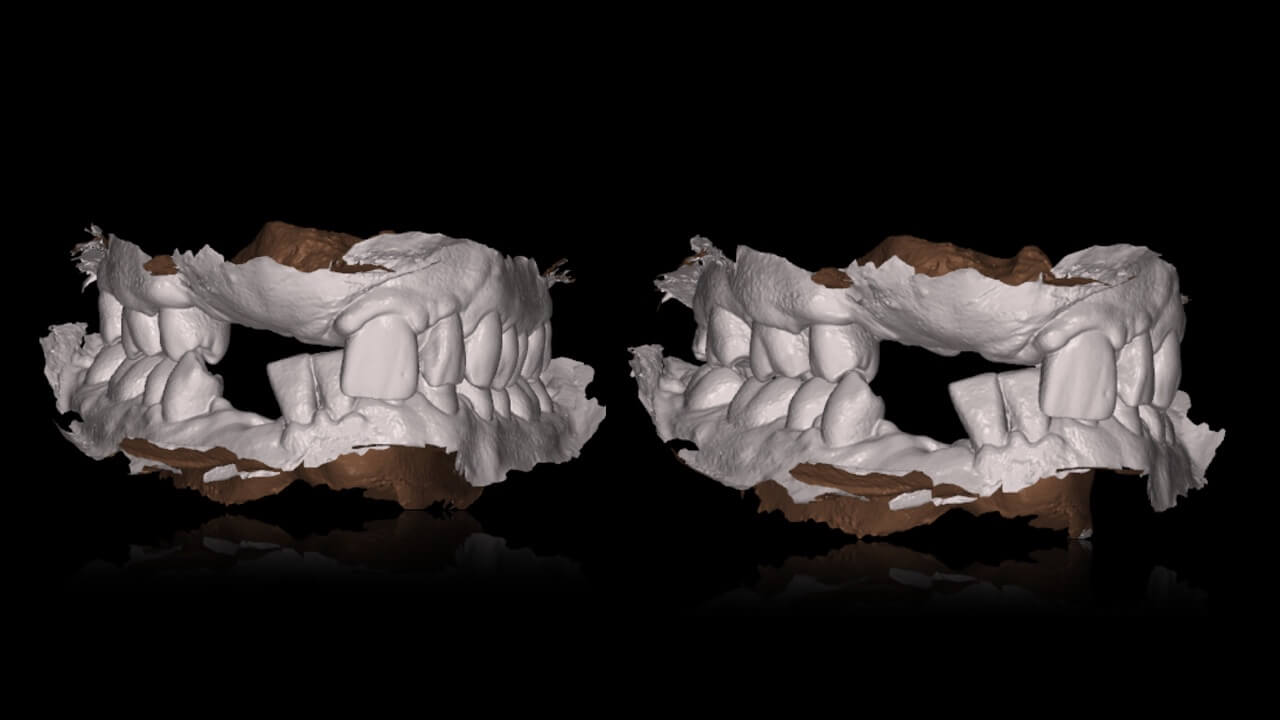 The file including digital information was sent to INCOGNITO (3M), a company in charge to produce a lingual orthodontic devices. Under direct control of the orthodontist, a set of brackets and nichel-titanium wires to be applied on the lingual side of mandibular dentiiton was fabricated and delivered for adequate alignment of the anterior mandibular teeth.
The file including digital information was sent to INCOGNITO (3M), a company in charge to produce a lingual orthodontic devices. Under direct control of the orthodontist, a set of brackets and nichel-titanium wires to be applied on the lingual side of mandibular dentiiton was fabricated and delivered for adequate alignment of the anterior mandibular teeth.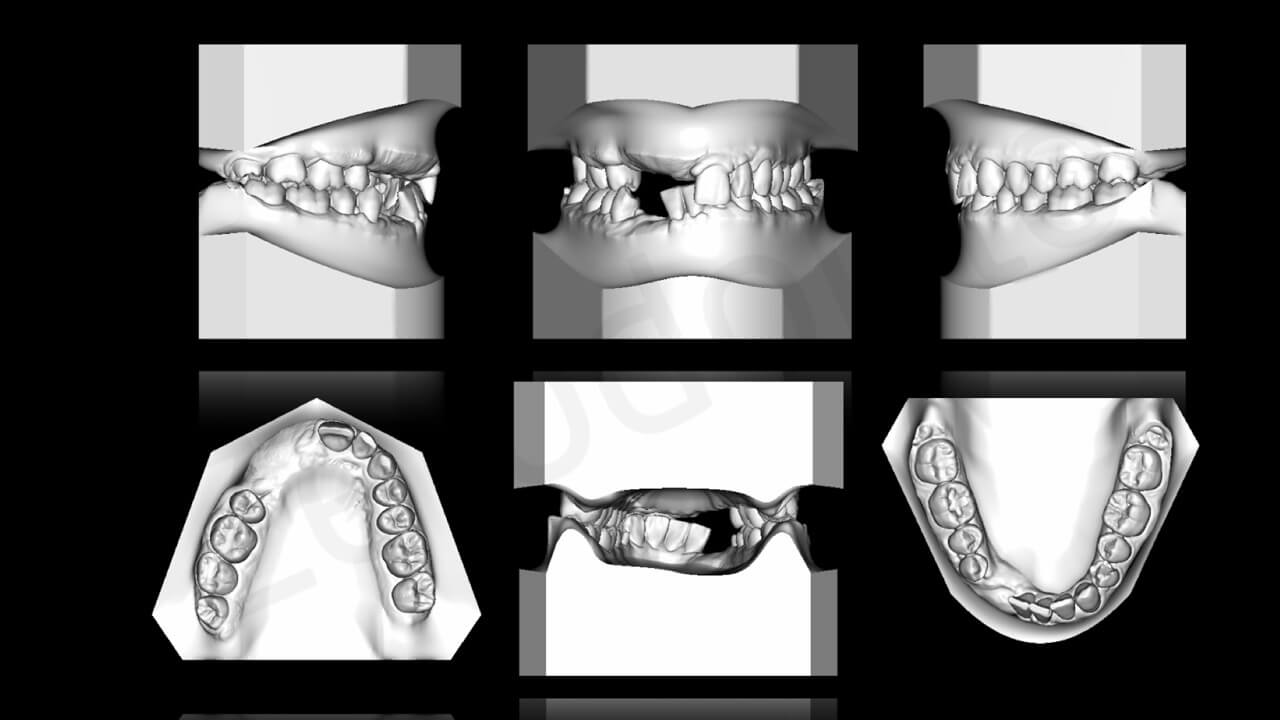
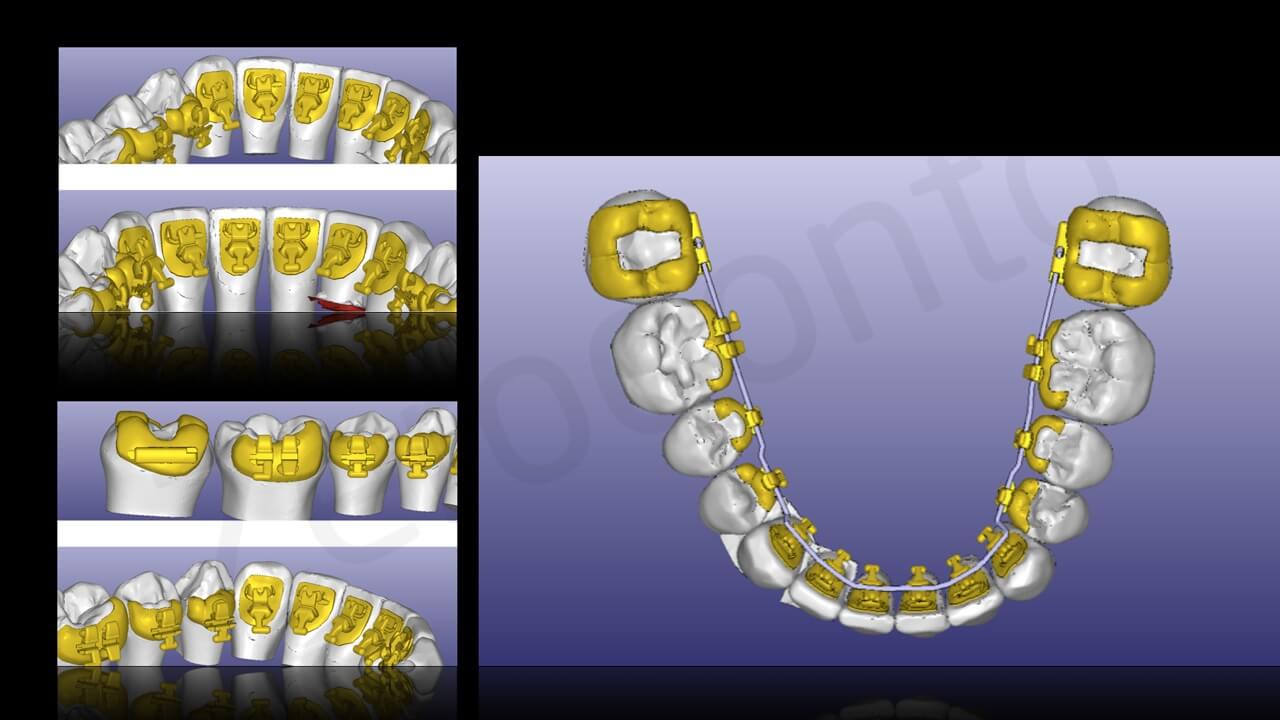 Brackets were then bonded to the inferior dental arch on the lingual side (CTP ED UNYCEM – 3M) and a first Nichel-Titanium alloy arch was applied. (fig. 52).
Brackets were then bonded to the inferior dental arch on the lingual side (CTP ED UNYCEM – 3M) and a first Nichel-Titanium alloy arch was applied. (fig. 52). Four months afterwards, a correct alignment of teeth and adequate room for implant placement in the edentulous area (42-43) was obtained.
Four months afterwards, a correct alignment of teeth and adequate room for implant placement in the edentulous area (42-43) was obtained.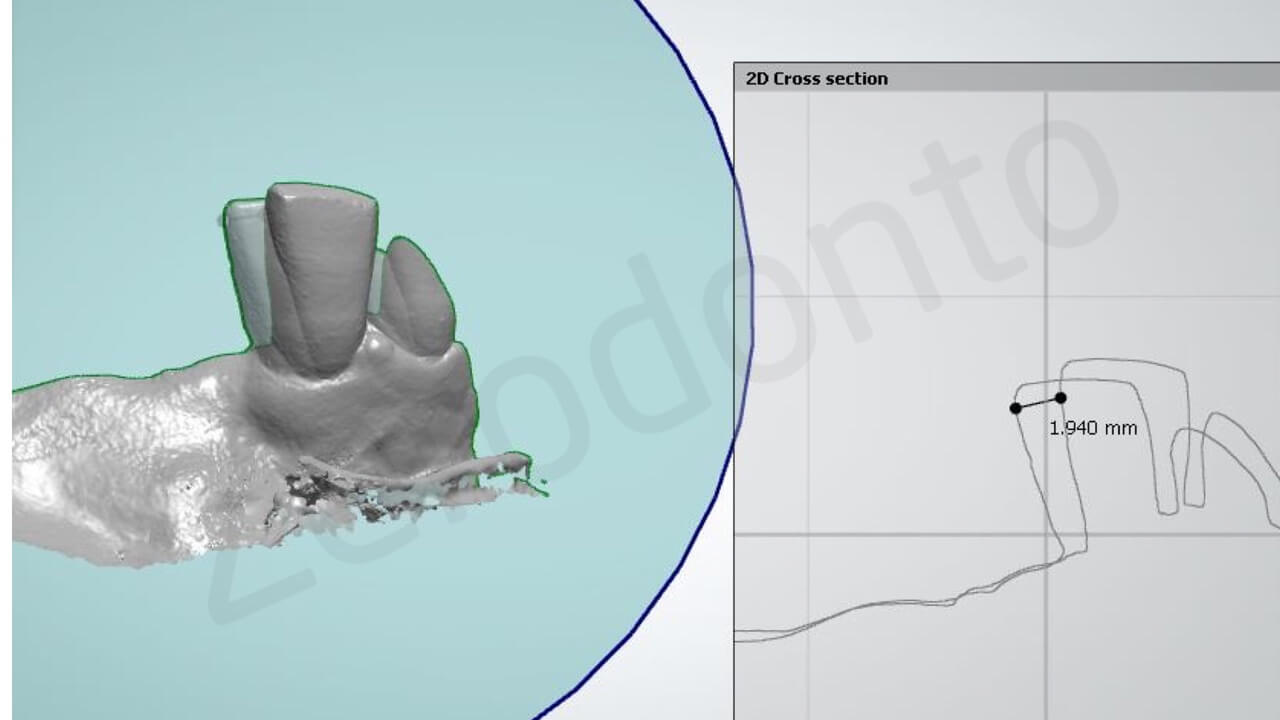
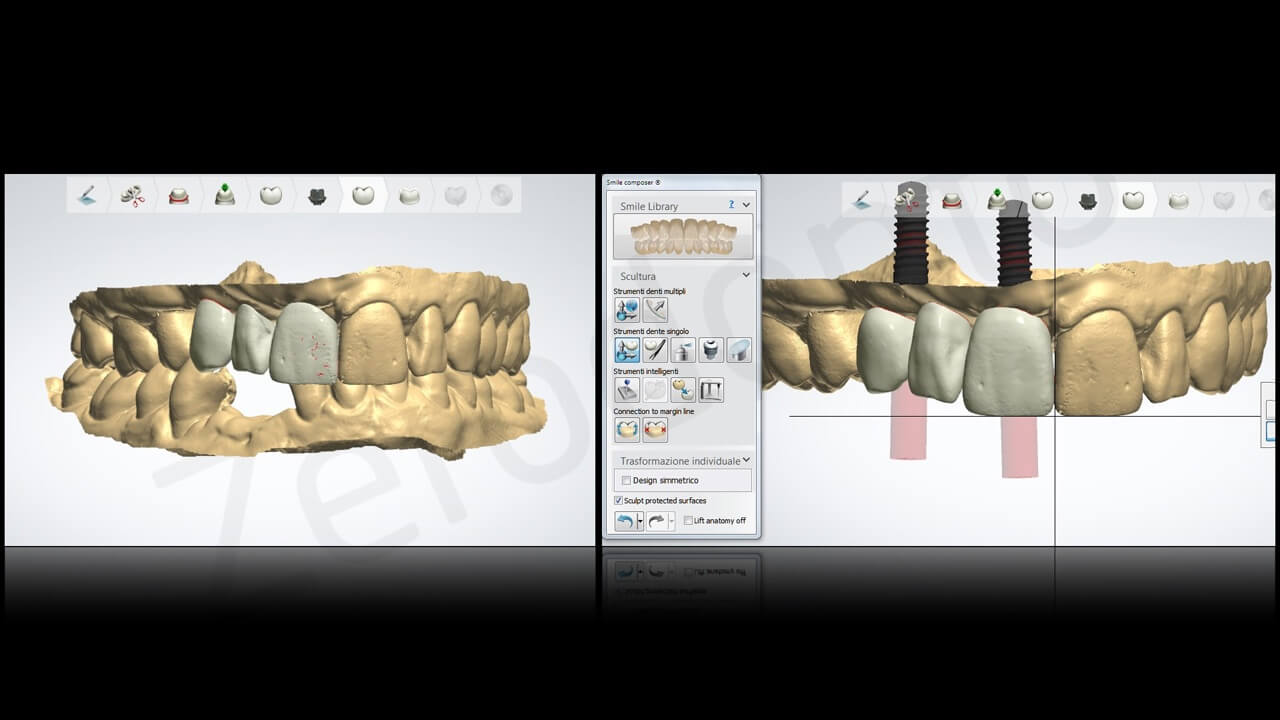
 The following step (November 2015) was represented by an intraoral digital scan and the files were sent by Dr. Venezia to his dental lab (Apulia Digital Lab – Bari – Italy) requesting a “virtual” wax-up of the missing maxillary and mandibular dentiiton
The following step (November 2015) was represented by an intraoral digital scan and the files were sent by Dr. Venezia to his dental lab (Apulia Digital Lab – Bari – Italy) requesting a “virtual” wax-up of the missing maxillary and mandibular dentiiton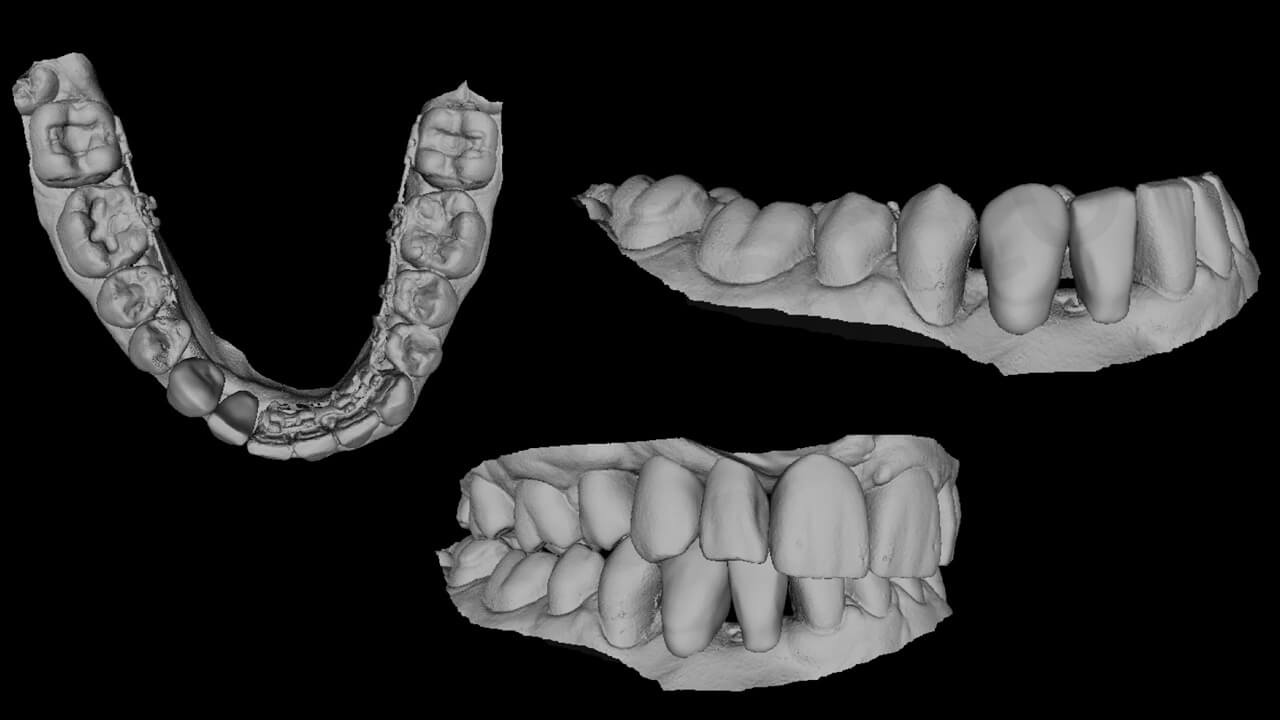 The super-imposition of the DICOM files of the CTCB with those deriving from the intraoral optical scanning performed with a dedicated software (Co-Diagnostix® – Dental Wings) allowed a precise pre-operative evaluation of implant positioning according to the final prosthetic restoration.
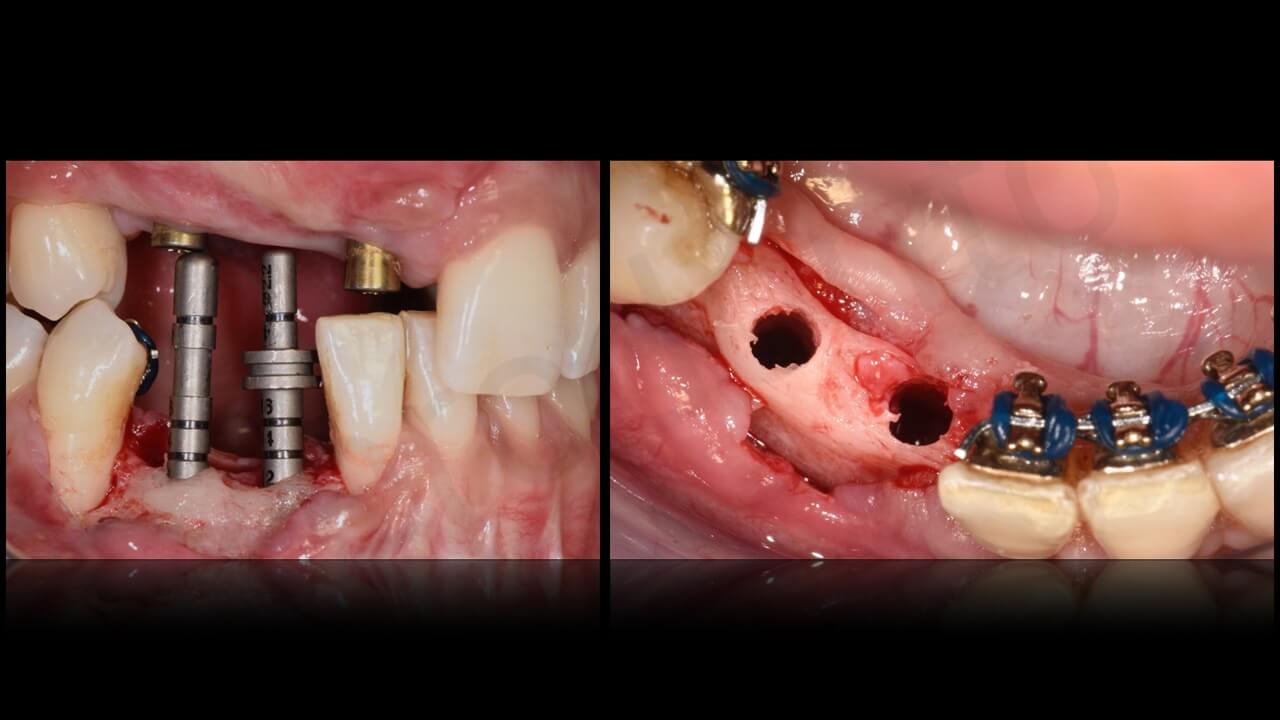
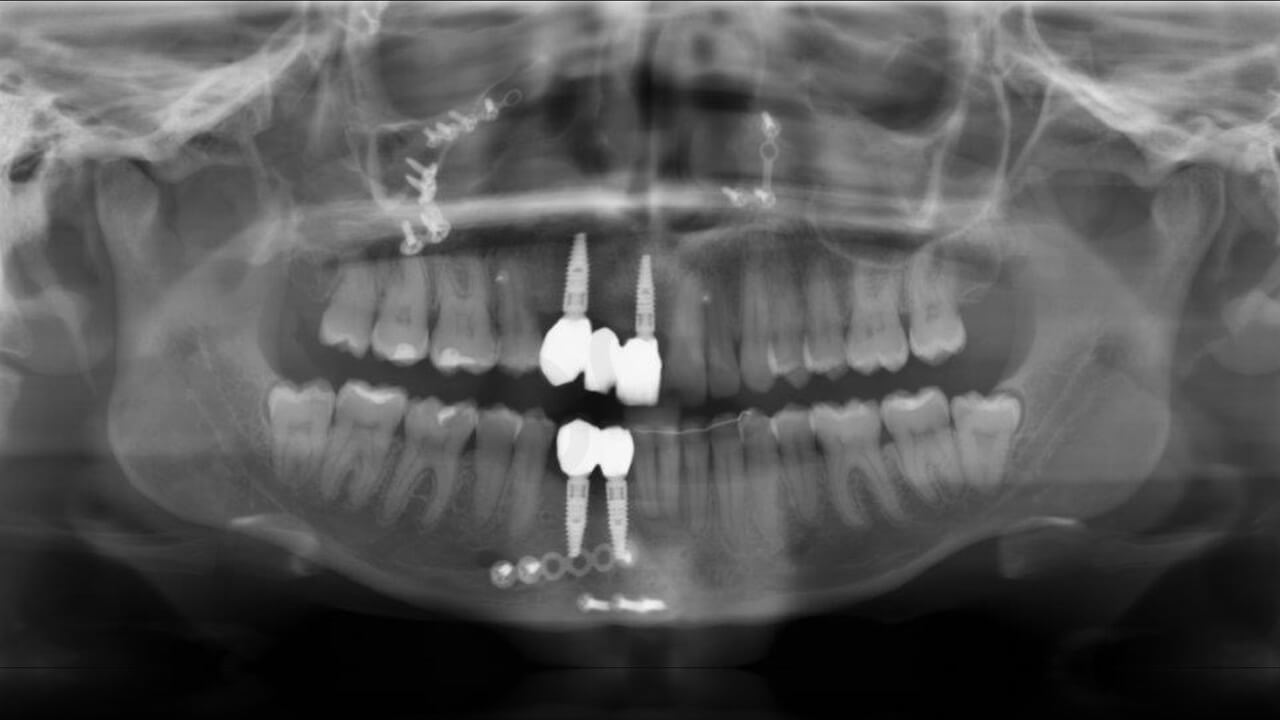
The super-imposition of the DICOM files of the CTCB with those deriving from the intraoral optical scanning performed with a dedicated software (Co-Diagnostix® – Dental Wings) allowed a precise pre-operative evaluation of implant positioning according to the final prosthetic restoration.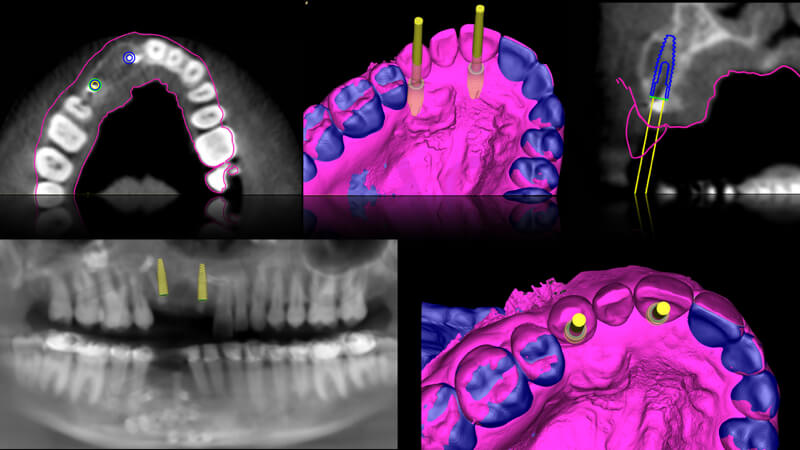 In the upper arch, according to the information obtained by digital analysis, 2 implants, 3.3 mm in diameter and 12 mm in length (Straumann BLT- Straumann Institute- Switzerland) were planned to support a 3-unit fixed prosthesis. One implant had to be placed in the area of the missing right central incisor and one in the area of the cuspid. It was decided to use a screw retention system of the new implant-supported bridge.
In the upper arch, according to the information obtained by digital analysis, 2 implants, 3.3 mm in diameter and 12 mm in length (Straumann BLT- Straumann Institute- Switzerland) were planned to support a 3-unit fixed prosthesis. One implant had to be placed in the area of the missing right central incisor and one in the area of the cuspid. It was decided to use a screw retention system of the new implant-supported bridge.
To optimize implant positioning, two surgical templates were produced according to the pre-operative prosthtic planning. The templates were obtained from a block of transparent PMMA (PMMA Tray Disc for Zenotec- Wieland) with 3mm holes to allow the passage of 3mm implant drills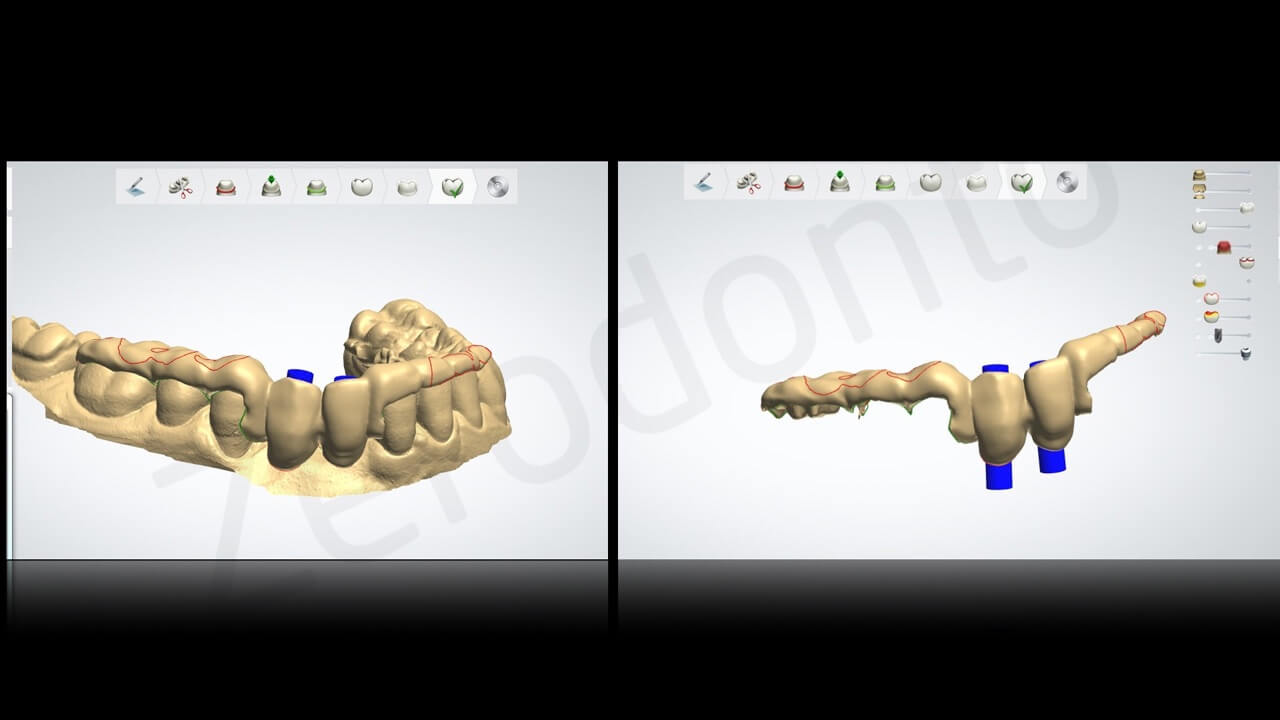

Step 4
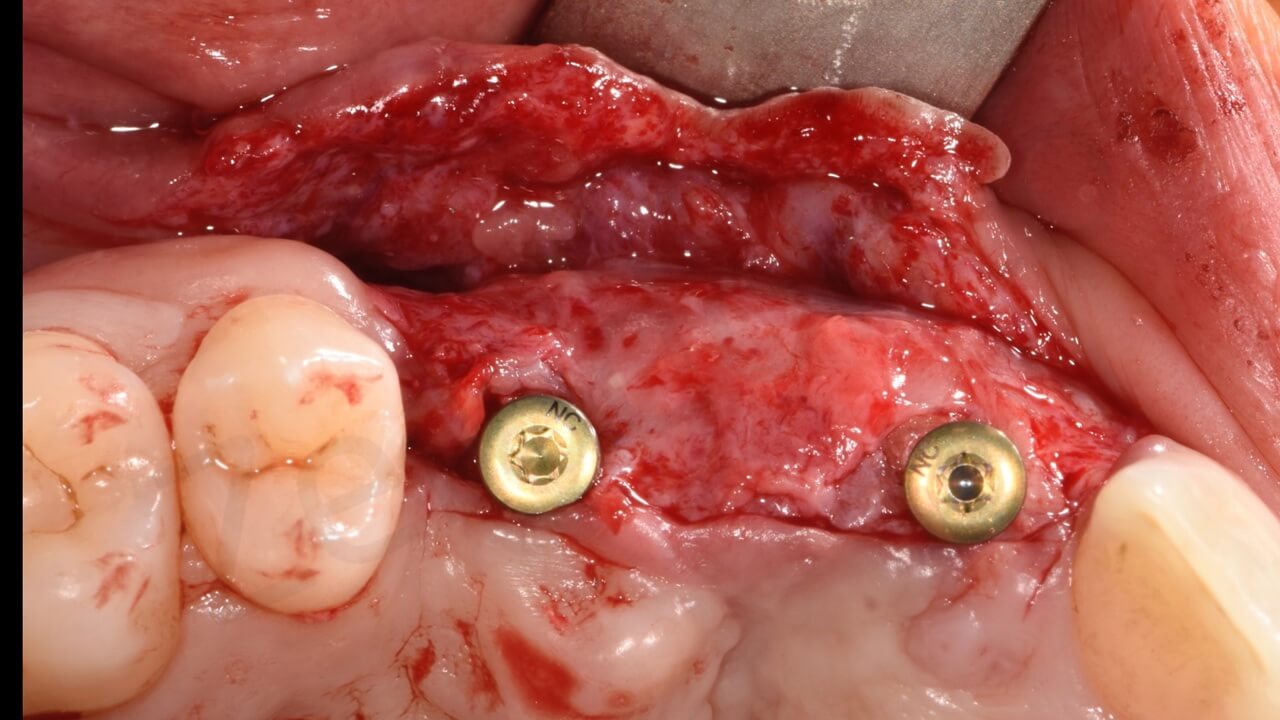
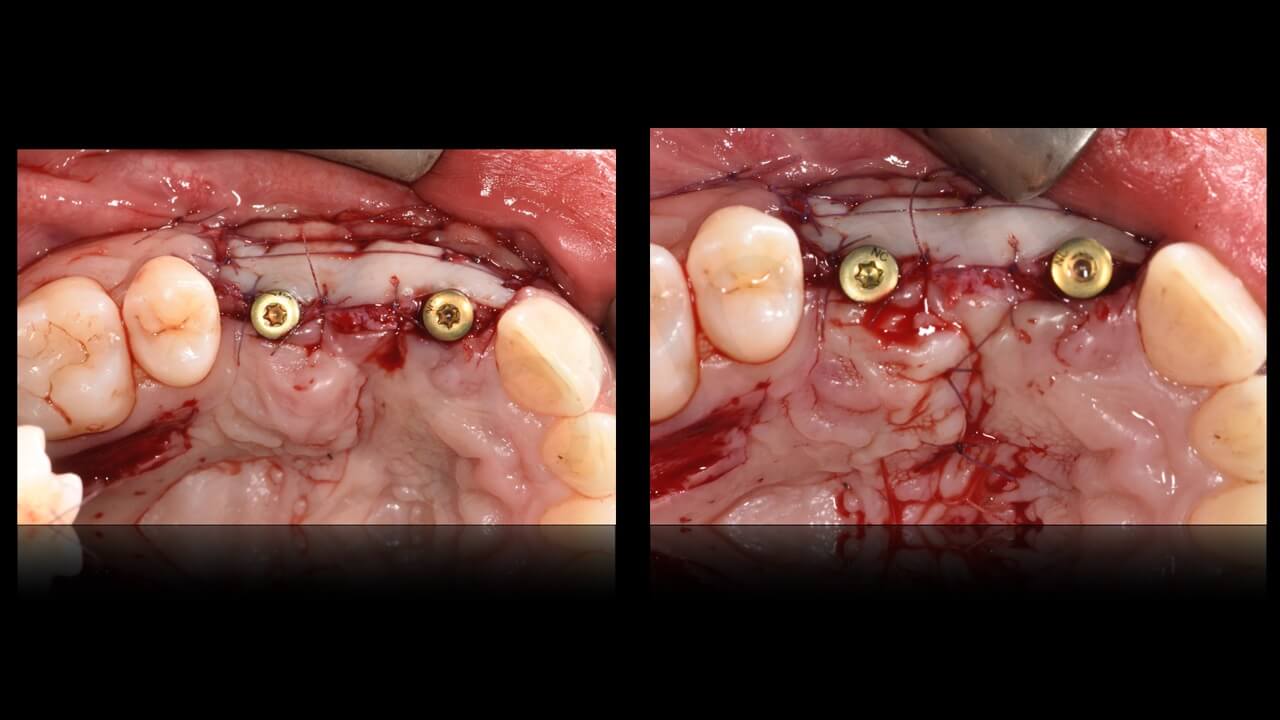
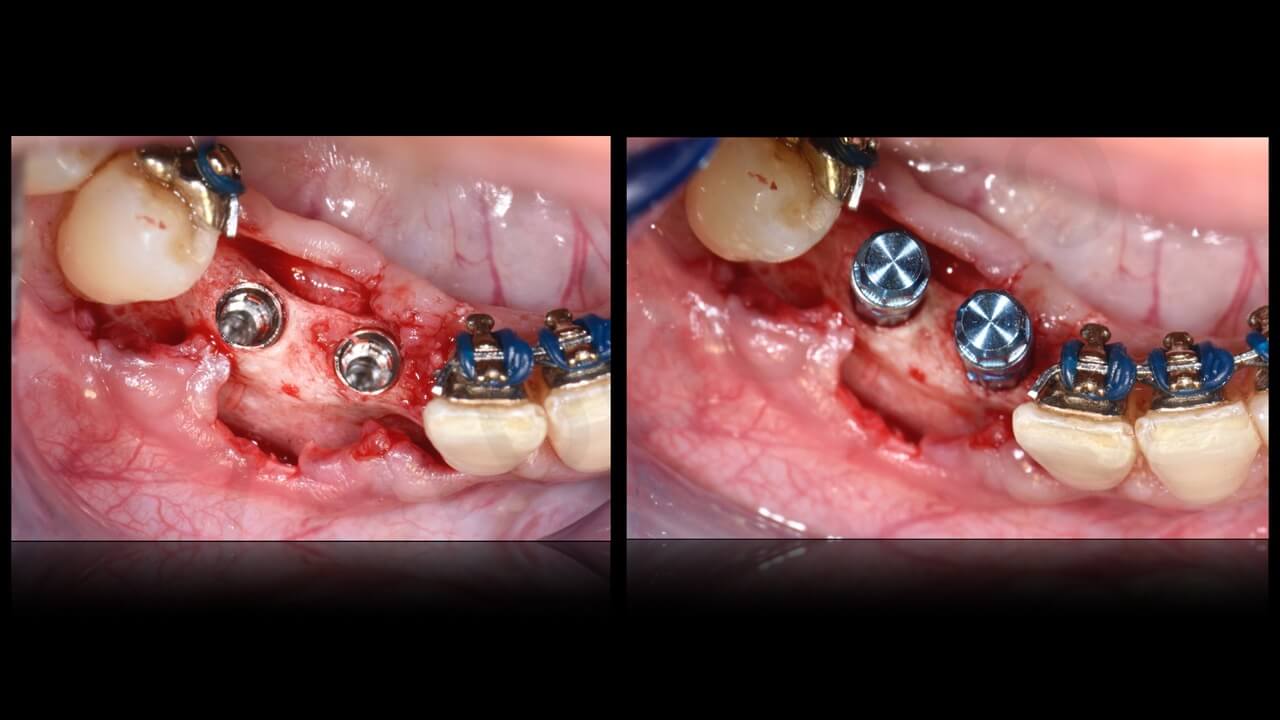
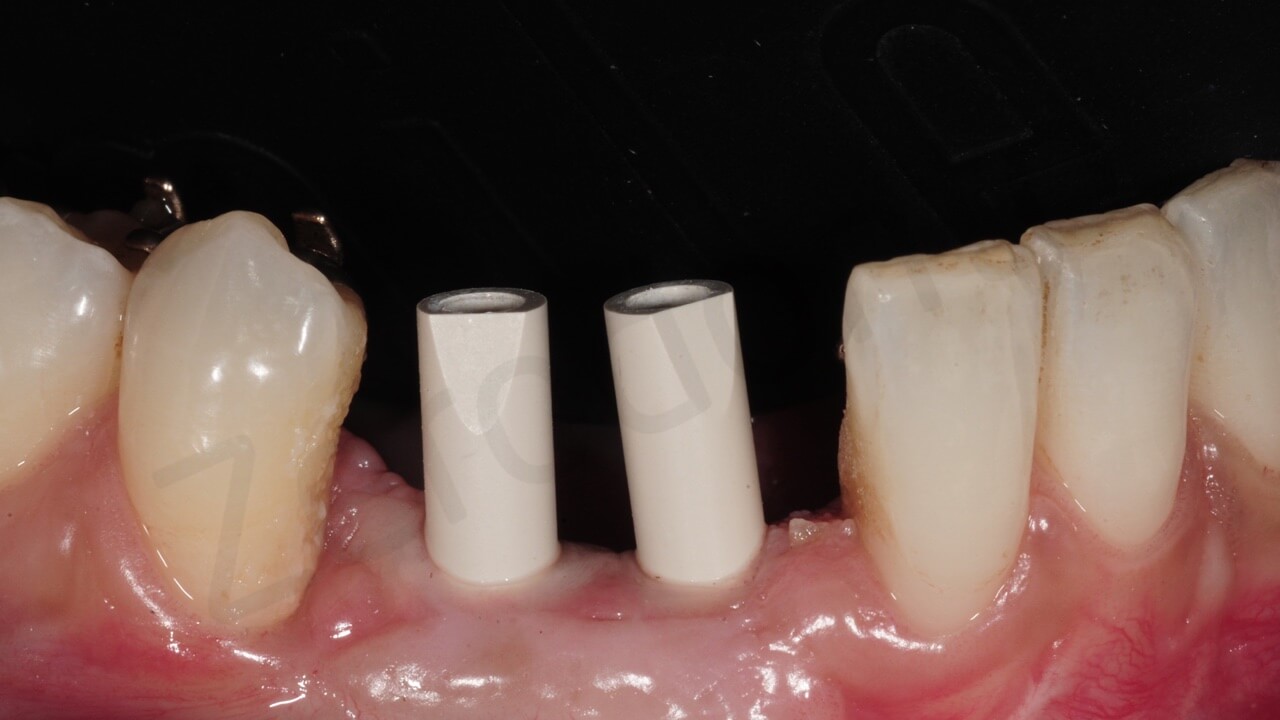
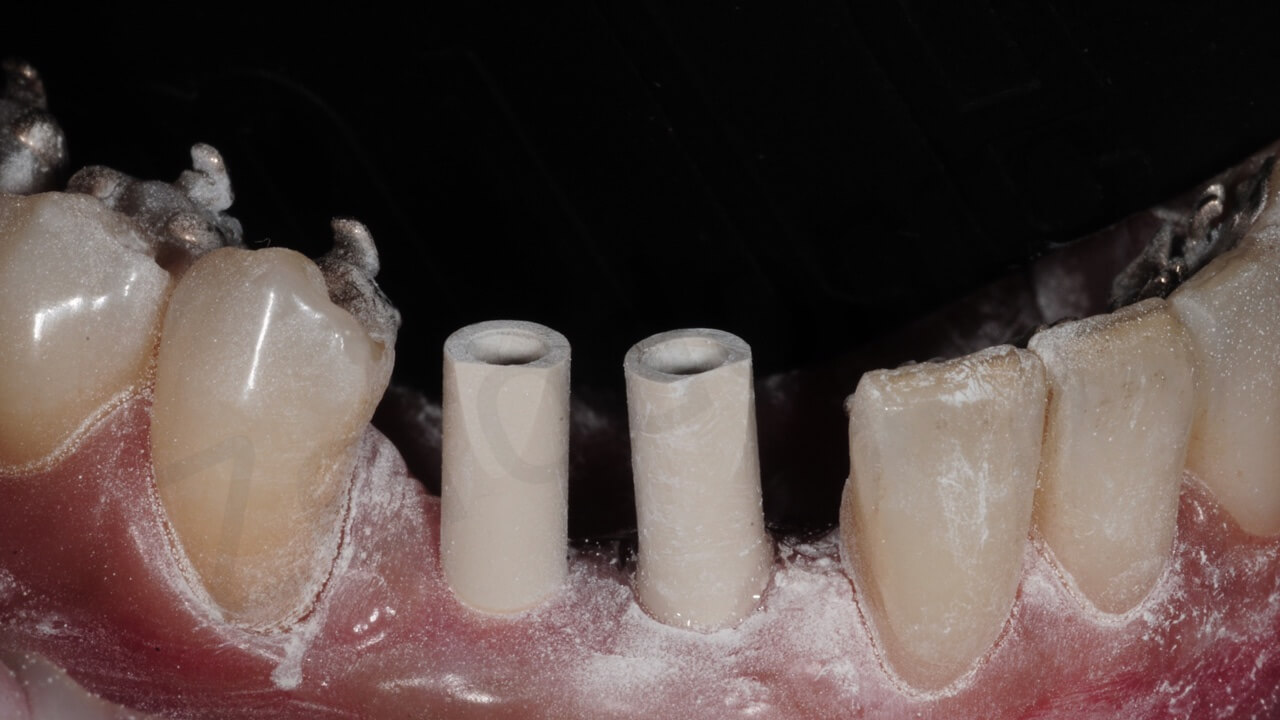
On December 20, 2015, Prof. Chiapasco, following the indications of the pre-fabricated templates placed 2 osseointegrated titanium-zirconium alloy implants (Straumann BLT) 3.3 mm in diameter and 12 mm in length. Implants were placed after the elevation of a partial tickness flap with the following aims: 1) do not disturb the still ongoing revascularization of the graft; and “) to perform at the same time a vestibuloplasty and a epithelial/connective tissue taken from the palate, to re-create the missing keratinized mucosa around the implants.
During the same session, again following the indications of the pre-fabricated template , 2 implants of the same type were placedc in the mandible at the level of missing teeth 42-43



Step 5
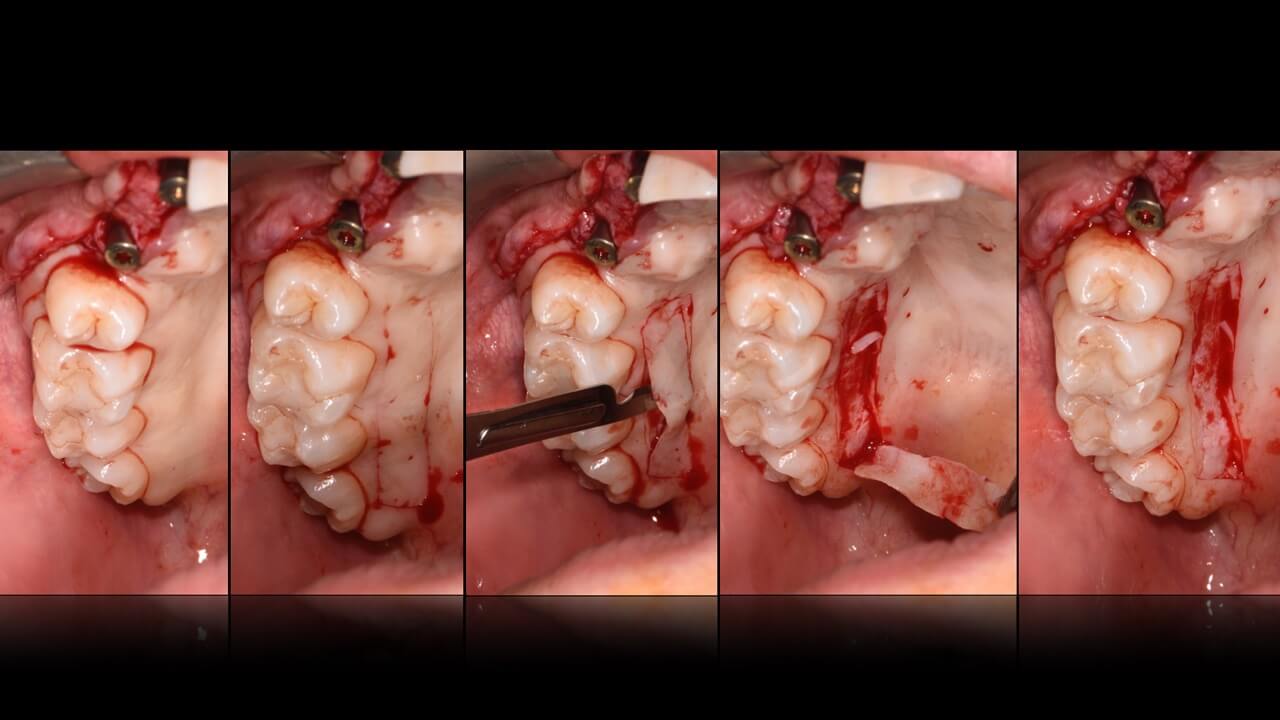
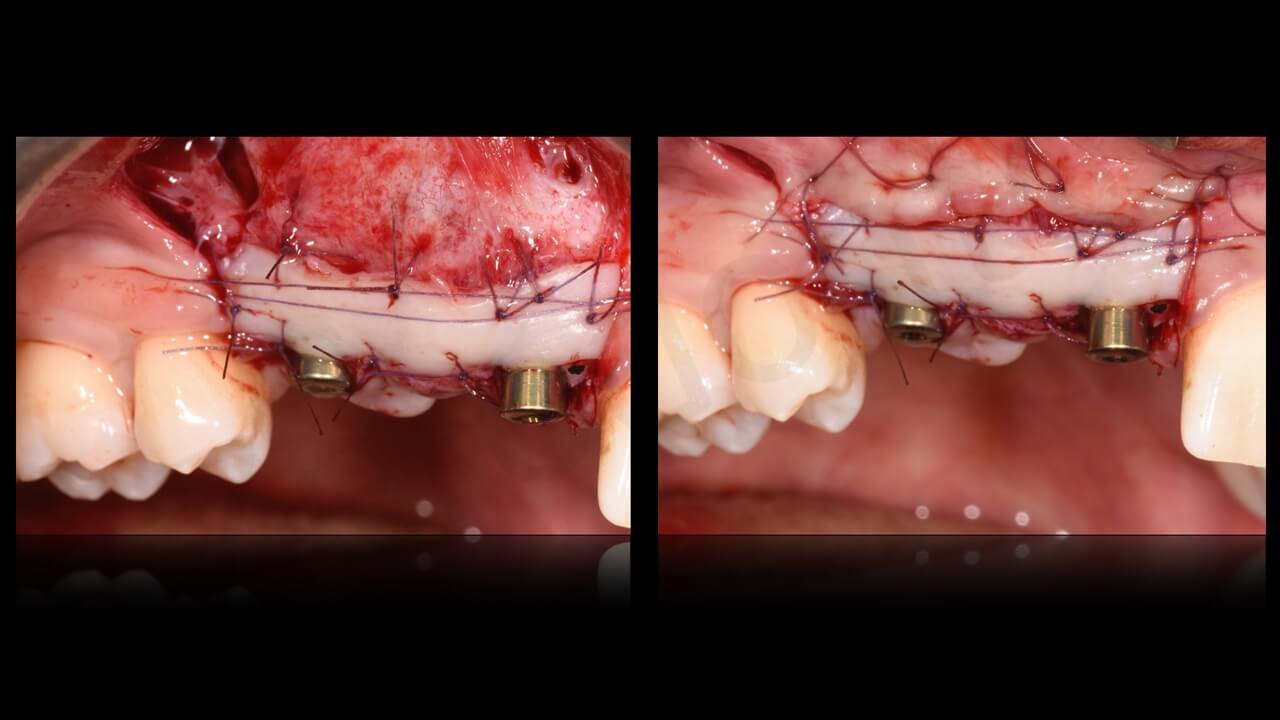
Two months later, dr. Cavalcanti, in order to optimize the quality and tickness of soft tissues around implants, further improved the width of connective tissues in the upper arch with an autogenous connective tissue graft taken from the palate in association with a collagen matrix (Mucograft®- Geistlich Biomaterials – Wolhusen-Switzerland)
Step 6
On March 2016, once implants were integrated, as well as peri-implant soft tissues, a new intraoral digital scan was taken to evaluate implant positioning.

 Two weeks later, a temporary prosthesis was delivered. Its production was performed thanks to a digital workflow: the CAD project allowed the modelling of a PMMA- Poli-Metil-Metacrilate block (TELIO-CAD Wieland). The temporary crowns obtained were then covered with a composite (NEXCO Paste IVOCLAR-VIVADENT). The coupling between the resin temporary prosthesis and the implant titanium abutments (Variobase® by Straumann) was performed with a resin cement (Multilink Hybrid Abutment – Ivoclar Vivadent).
Two weeks later, a temporary prosthesis was delivered. Its production was performed thanks to a digital workflow: the CAD project allowed the modelling of a PMMA- Poli-Metil-Metacrilate block (TELIO-CAD Wieland). The temporary crowns obtained were then covered with a composite (NEXCO Paste IVOCLAR-VIVADENT). The coupling between the resin temporary prosthesis and the implant titanium abutments (Variobase® by Straumann) was performed with a resin cement (Multilink Hybrid Abutment – Ivoclar Vivadent). The temporary crowns were modelled in order not to compress soft tissues.
The temporary crowns were modelled in order not to compress soft tissues. The crowns were screwed with a 25 newton torque and the access to the screw heads were covered with a teflon pallet and closed with a temporary composite resin. (Telio Onlay – Ivoclar – Vivadent).
The crowns were screwed with a 25 newton torque and the access to the screw heads were covered with a teflon pallet and closed with a temporary composite resin. (Telio Onlay – Ivoclar – Vivadent).
One month later, an epithelial graft taken from the palate was used by dr. Cavalcanti to improve the quantity of keratinized mucosa around the mandibular implants. After another 3 months necessary for adequate integration of the soft tisue graft, a new set of intraoral digital scans were taken to evaluate the positon of the mandibular implants to allow a proper construction of temporary crowns in the dental lab.
After another 3 months necessary for adequate integration of the soft tisue graft, a new set of intraoral digital scans were taken to evaluate the positon of the mandibular implants to allow a proper construction of temporary crowns in the dental lab.
 To optimize the final prosthetic result, a new temporary prostehsis with an ovate shaped crown at the level of tooth 12 was done.
To optimize the final prosthetic result, a new temporary prostehsis with an ovate shaped crown at the level of tooth 12 was done.
Then, gradual increases of composite material over the temporary crowns were apllied in order to improve the shape of peri-implnat soft tissues (fig. xx-xx).
Two months later, peri-implant soft tissues appeared very well integrated with the crowns profile, from an esthetic and functional point of view.
Finally, the orthodontic appliance was removed.


Step 7
Implant position were were scanned with dedicated scan bodies; Temporary bridges screwed to implant abutments in the oral cavity as well as temporary bridges screwed on analogues embedded in a heavy viscosity silicon master models were also scanned with the same machine (titanium- zhermack).
The files obtained were matched together in order to reproduce in a very precise way the trans-mucosal part of the temporary crowns as well as the soft tissues conditioned by the ovate pontic in the upper arch.
These files were extremely useful for the construction of the final prosthetic restorations in the dental lab. Then, a first esthetic and functional analysis was performed with a white PMMA tray disc test drive (ZENOTEC – WIELAND)
Then, a first esthetic and functional analysis was performed with a white PMMA tray disc test drive (ZENOTEC – WIELAND) Finally, the zirconia monolithic structures (Zenotec Traslucent T1 – Wieland) were verified in the oral cavity to evaluate occlusion parameters and the passive fit of the prosthesis superstructure to the implants.
Finally, the zirconia monolithic structures (Zenotec Traslucent T1 – Wieland) were verified in the oral cavity to evaluate occlusion parameters and the passive fit of the prosthesis superstructure to the implants. The final restoration was obtained with a zirconia-ceramic adhesion interface on the buccal side using E-MAX CERAM e IVOCOLOR (Ivoclar Vivadent) and then the zirconia superstructures were embedded to the titanium abutments.
The final restoration was obtained with a zirconia-ceramic adhesion interface on the buccal side using E-MAX CERAM e IVOCOLOR (Ivoclar Vivadent) and then the zirconia superstructures were embedded to the titanium abutments.
The abutments were screwed with a 35 N tightening torque of and the screw-access hole was sealed with teflon and composite (Emamel Plus- Micerium).
The final x-rays show a perfect fit between implants and prosthetic rehabilitation. The patient was very satisfied by the aesthetic and functional result.



Acknowledgements
We thank Pasquale Lacasella, CDT Francesco GRIECO CDT and Dino GALLO CDT (Dental Laboratory APULIA DIGITAL LAB – BARI) and Vincenzo SANTOMAURO MD for their fundamental support.
REFERENCES
- The Smile Esthetic Index (SEI): A method to measure the esthetics of the smile. An intra- rater and inter-rater agreement study.
Rotundo R, Nieri M, Bonaccini D, Mori M, Lamberti E, Massironi D, Giachetti L, Franchi L, Venezia P, Cavalcanti R, Bondi E, Farneti M, Pinchi V, Buti J.
Eur J Oral Implantol. 2015 Winter;8(4):397-403
- The BARI technique: a new approach to immediate loading.
Venezia P, Lacasella P, Cordaro L, Torsello F, Cavalcanti R.
Int J Esthet Dent. 2015 Autumn;10(3):428-43.
- Retrospective analysis of 26 complete-arch implant-supported monolithic zirconia prosthe- ses with feldspathic porcelain veneering limited to the facial surface.
Venezia P, Torsello F, Cavalcanti R, D’Amato S.
J Prosthet Dent. 2015 Oct;114(4):506-12
- Custom impression coping for an exact registration of the healed tissue in the esthetic implant restoration.
Hinds KF.
Int J Periodontics Restorative Dent. 1997 Dec;17(6):584-91.
- Implants in reconstructed bone: a comparative study on the outcome of Straumann® tissue level and bone level implants placed in vertically deficient alveolar ridges treated by means of autogenous onlay bone grafts.
Chiapasco M, Casentini P, Zaniboni M.
Clin Implant Dent Relat Res. 2014 Feb;16(1):32-50. doi: 10.1111/j.1708-8208.2012.00457.x. Epub 2012 Apr 11.
- Bone augmentation procedures in implant dentistry.
Chiapasco M, Casentini P, Zaniboni M.
Int J Oral Maxillofac Implants. 2009;24 Suppl:237-59. Review.
- Autogenous onlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a 2-4-year prospective study on humans.
Chiapasco M, Zaniboni M, Rimondini L.
Clin Oral Implants Res. 2007 Aug;18(4):432-40. Epub 2007 May 14.
- Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants.
Chiapasco M, Zaniboni M, Boisco M.
Clin Oral Implants Res. 2006 Oct;17 Suppl 2:136-59. Review.
- Clinical outcome of autogenous bone blocks or guided bone regeneration with e-PTFE membranes for the reconstruction of narrow edentulous ridges.
Chiapasco M, Abati S, Romeo E, Vogel G.
Clin Oral Implants Res. 1999 Aug;10(4):278-88.

