Introduction
Oral surgery in children is not always an easy surgery. It is often complicated by:
– specific age-related pathologies, not always easy to recognize
– complex anatomy associated with the mixed dentition
– reduced surgical access
– difficulties in obtaining the cooperation
– the need for coordinating surgery and orthodontics
There are opportunities for oral surgery typical age-related operations and other conditions that require a different approach when patients are children:
– extraction of infraoccluded primary teeth
– extraction of impacted supernumerary teeth
– treatment of cysts
– germectomies of mandibular wisdom teeth
Extraction of infraoccluded primary teeth
The infraocclusion consists of a cessation of the growth of the alveolar process which results in a seeming apical displacement of primary teeth, especially molars. It is important to know that infraocclusion can worsen rapidly.
Diagnosis and Treatment
– slight infraocclusion: the occlusal surface of the deciduous tooth is located between the occlusal plane of the adjacent teeth and their equator.
 8 year old girl with mild infraocclusion of 65
8 year old girl with mild infraocclusion of 65
The recommended management of such cases is monitoring by frequent clinical (not radiographic) examination in order to carry out timely extraction, if the infraocclusion worsens.

 The infraocclusion of the second primary molar increases and becomes moderate one year after the radiograph, thus requiring the extraction
The infraocclusion of the second primary molar increases and becomes moderate one year after the radiograph, thus requiring the extraction
– moderate infraocclusion: the occlusal surface of the primary tooth is located between the equator of the adjacent teeth and the gingival margin. It is generally associated with tilting of adjacent teeth and block or diversion of the eruption path of the corresponding permanent teeth. The treatment consists of the extraction.
 Male 7 year old child with moderate infraocclusion of 55 and apical displacement of 15
Male 7 year old child with moderate infraocclusion of 55 and apical displacement of 15
 The intraoral radiograph shows the shape of the roots of 55
The intraoral radiograph shows the shape of the roots of 55
 The apical displacement of the second primary molar is clinically and radiographically evident
The apical displacement of the second primary molar is clinically and radiographically evident
 The extraction of infraoccluded primary tooth required the division of the roots: particular attention should be paid to preventing damage to the permanent tooth
The extraction of infraoccluded primary tooth required the division of the roots: particular attention should be paid to preventing damage to the permanent tooth
– severe infraocclusion: the occlusal surface of the deciduous tooth is located at the level of the gingival margin or more apically; the infraoccluded tooth may become completely intraosseous. The diagnosis was not timely enough in these cases.
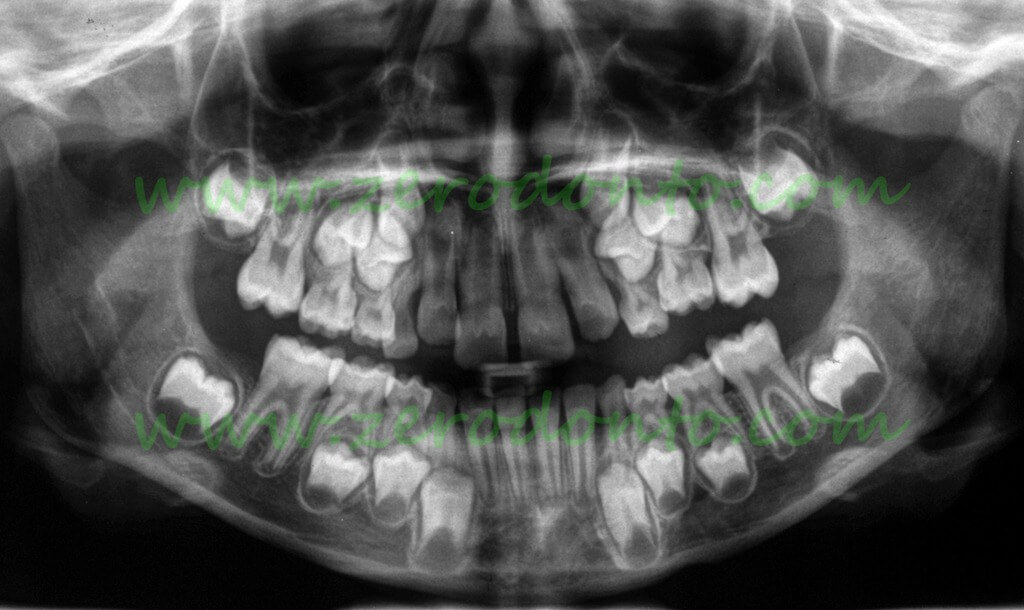
 Panoramic radiograph of a 9 year old patient:
Panoramic radiograph of a 9 year old patient:
• the upper right second primary molar is severely infraoccluded and associated with mesial displacement of the premolars and mesial tilting of the first permanent molar, resulting in evident loss of space
• the lower right second primary molar is severely infraoccluded and associated with mesial tilting of the first permanent molar and apical displacement of the second premolar
![clip_image001[4] clip_image001[4]](https://www.zerodonto.com/en/wp-content/uploads/2013/06/clip_image0014_thumb10.jpg) Clinically, the second premolar appears to be missing in the arch while significant loss of space occurred. The arrow indicates the area of the infraoccluded primary molar
Clinically, the second premolar appears to be missing in the arch while significant loss of space occurred. The arrow indicates the area of the infraoccluded primary molar
The treatment consists in surgical removal of the primary molar and in orthodontic treatment in order to correct the inclination of the adjacent teeth associated with severe loss of space, block and diversion the eruption path of permanent teeth and extrusion of the corresponding antagonists. All of these problems could be avoided by timely diagnosis and treatment.
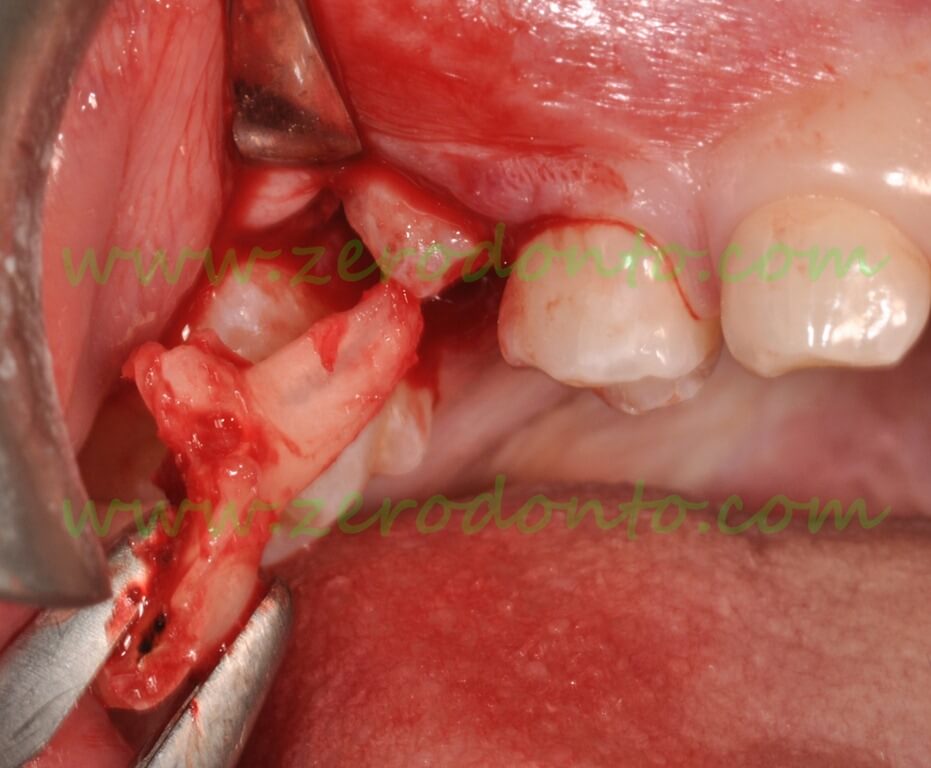
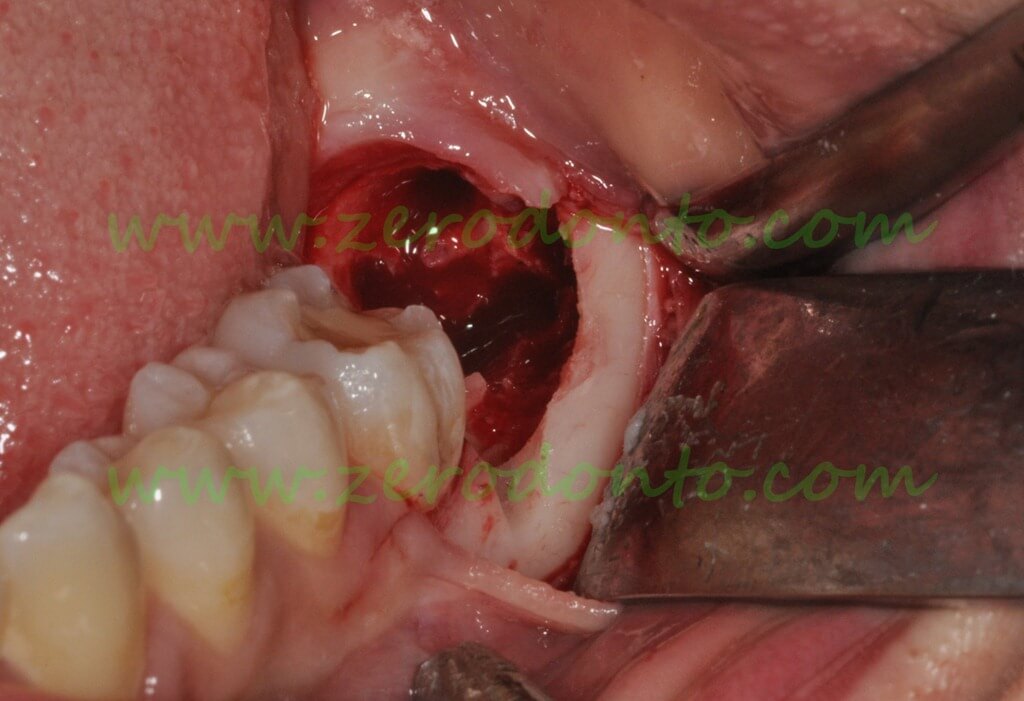
 Opening a flap and exposure of the infraoccluded primary molar
Opening a flap and exposure of the infraoccluded primary molar
 Removal of the mesial fragment after tooth fragmentation
Removal of the mesial fragment after tooth fragmentation
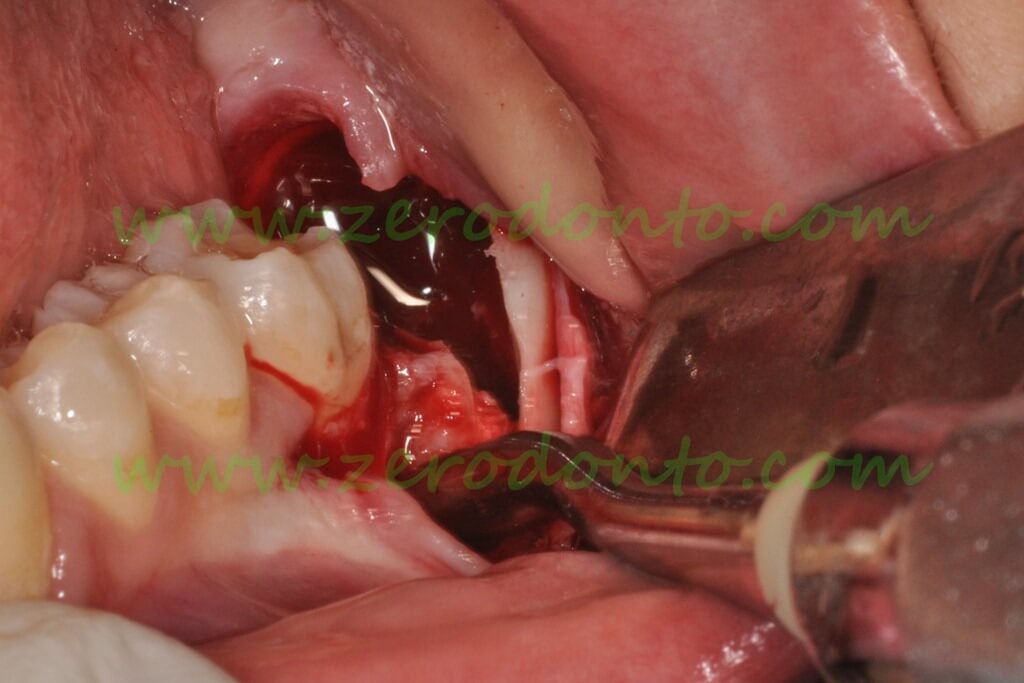
 The pericorona of the permanent germ can bee seen in the wound
The pericorona of the permanent germ can bee seen in the wound
Extraction of impacted supernumerary teeth
The diagnosis of impacted supernumerary is made on X-ray examinations performed for other reasons or due to indirect clinical signs such as missing or altered eruption of a permanent tooth.
 Panoramic radiograph of an 8 year old patient with two supernumerary teeth that block the upper left central incisor
Panoramic radiograph of an 8 year old patient with two supernumerary teeth that block the upper left central incisor
The surgical access is determined by the buccal or palatal / lingual location of the supernumerary tooth relative to the roots and germs of the adjacent permanent teeth. Therefore the following are needed:
• knowledge of the anatomy
• knowledge of the usual position of the supernumerary teeth
• a panoramic radiograph, and possibly an intraoral film too.
The use of three-dimensional imaging is almost always unjustified and often conceals a lack of knowledge of the condition.
The diagnosis is often made at 6-7 years of age, when the cooperation of the child may still be insufficient. There are rarely indications for urgent action: normally you can postpone the surgery without damage and wait for the moment when the patient’s cooperation makes the operation under local anesthesia simple and atraumatic, even from the psychological point of view.
 OPT of a patient 6 years with a supernumerary that blocks the upper right central incisor
OPT of a patient 6 years with a supernumerary that blocks the upper right central incisor
Conscious sedation with nitrous oxide is indicated in some cases of uncooperative children.
General anesthesia for the removal of supernumerary teeth should be considered a last resort and not a tranquilizer for the surgeon, when he or she is unable to plan the surgery rationally and to manage the psychological needs of the child appropriately. The major risks associated with general anesthesia are not justified by most dental disorders: serious complications are rare, but may be irreparable.
 Supernumerary tooth (mesiodens) associated with malposition of 21 in a 13 year old patient.
Supernumerary tooth (mesiodens) associated with malposition of 21 in a 13 year old patient.
The decision was made to remove the supernumerary tooth before orthodontic treatment:
VIDEO
• Marginal incision delimits an envelope flap
• The flap is elevated with preservation of the nasopalatal neurovascular bundle
• Bone resection by pneumatic sonic handpiece
• Partial fragmentation of the crown by bur
• Completion of the separation with a hand instrument
• Removal of the fragments with a surgical curette and a forceps for fragments
• The neurovascular bundle remained intact
 Fragments of the extracted supernumerary tooth
Fragments of the extracted supernumerary tooth
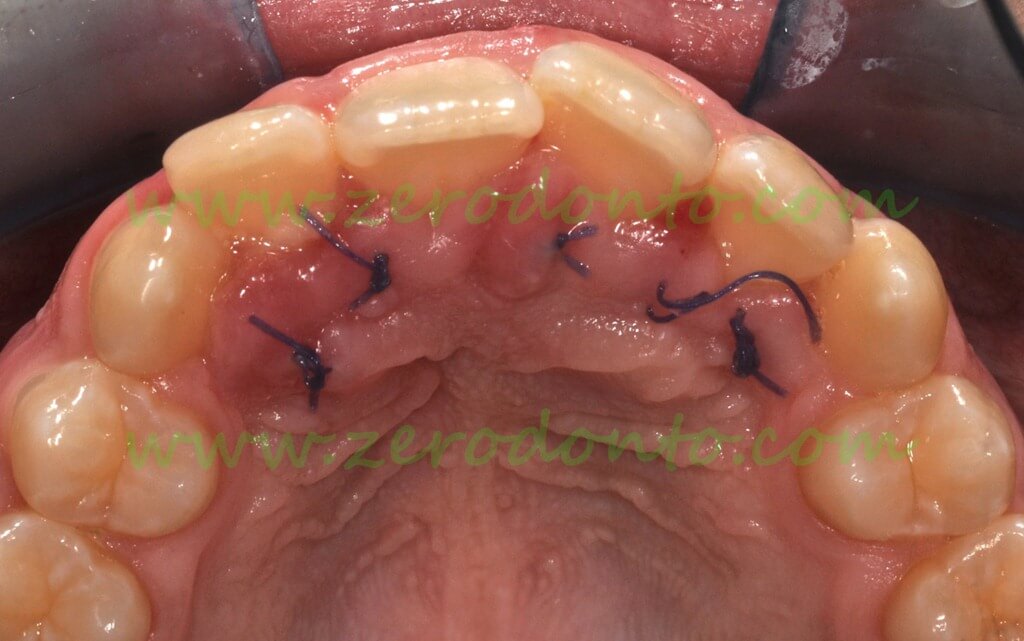
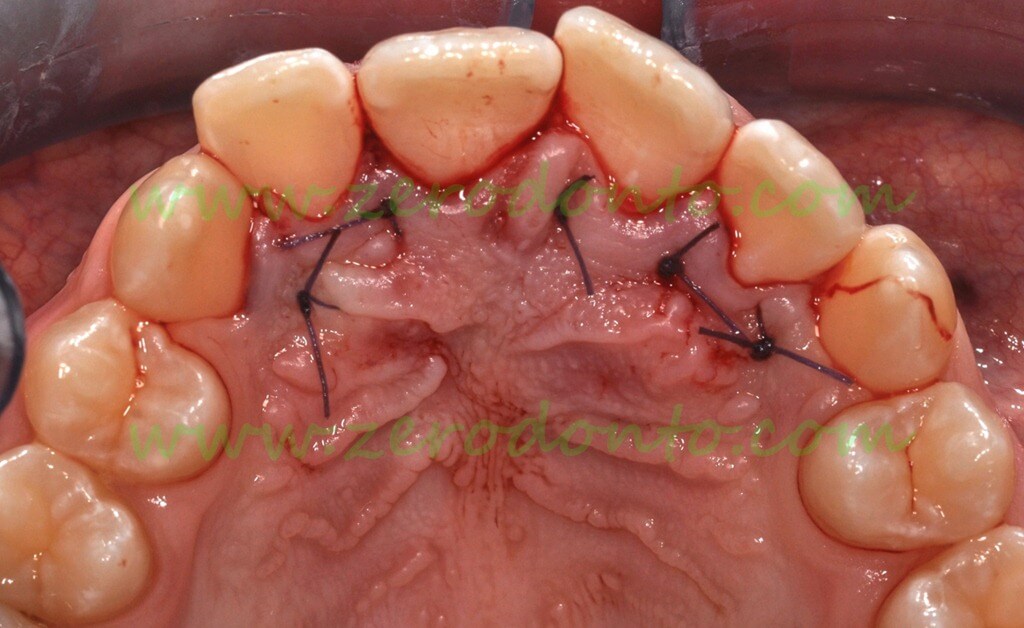 Interdental vertical mattress sutures
Interdental vertical mattress sutures
 The wound seven days after surgery
The wound seven days after surgery
 One month after surgery
One month after surgery
Treatment of Dentigerous Cysts
The most frequently encountered cyst in children and adolescents is the dentigerous cyst associated with the crown of germs of permanent teeth. The growing cyst displaces the germs, mainly in an apical direction.
The problems to be solved are:
– elimination of the cyst
– histopathologic confirmation of presumptive clinical diagnosis
– driving the displaced teeth to the arch
The first-choice treatment of dentigerous cysts consists of incisional biopsy associated with marsupialization in children, while the first choice in the adult is excisional biopsy.
The main steps of the procedure are:
– creating an opening in the ridge by removing the corresponding primary teeth
– taking out a piece of the cyst wall (incisional biopsy)
– maintening the opening in the ridge by means of an acrylic cone, which is usually connected to a retainer for space maintenance
Sketch of a typical case
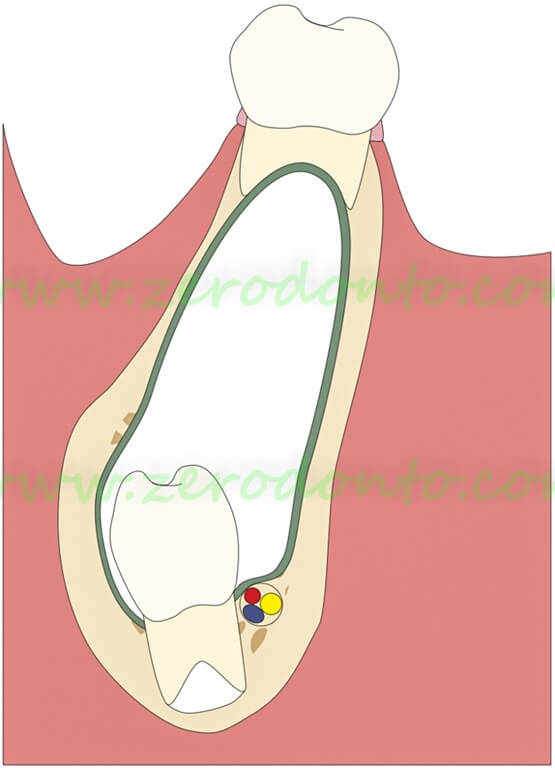
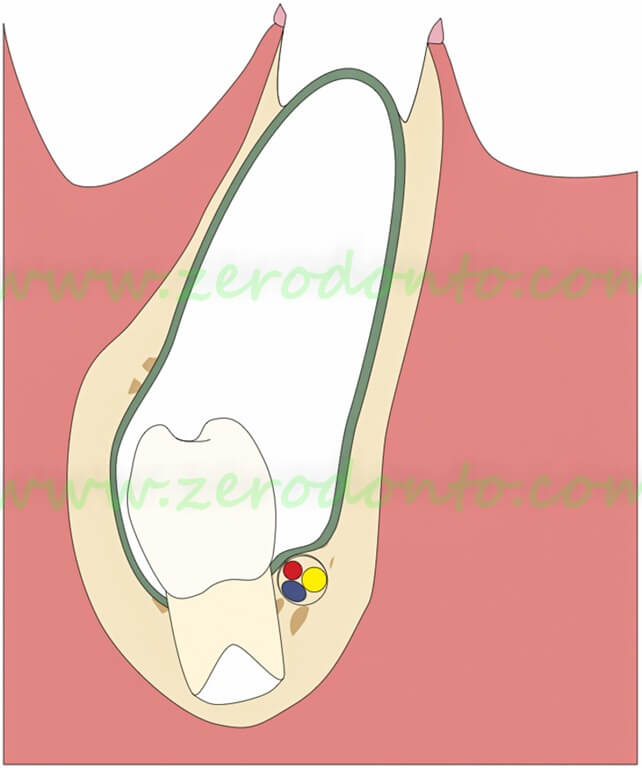
Mandibular cyst associated with persistence of a primary molar and apical displacement of the germ of the premolar. The removal of the primary molar exposes the cyst wall
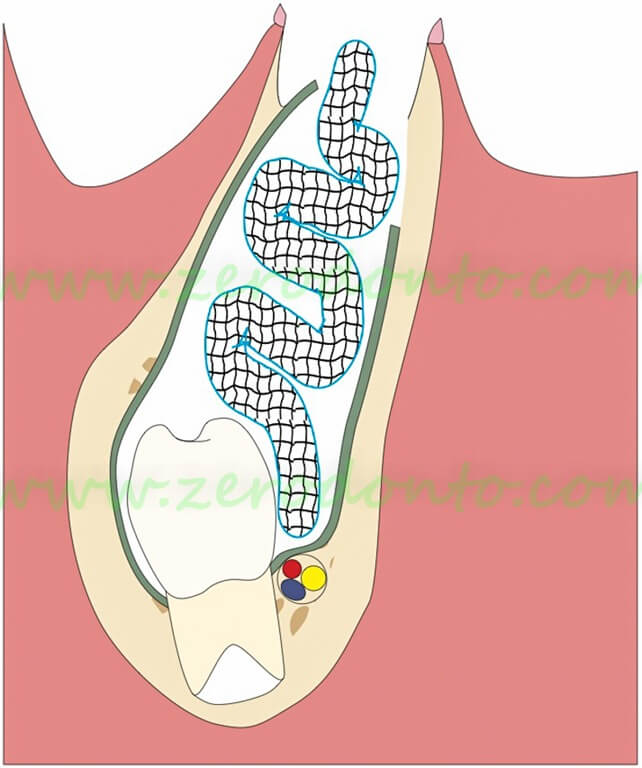 Harvesting of a portion of the cyst wall (biopsy) and insertion of iodoform gauze or of a rubber drainage
Harvesting of a portion of the cyst wall (biopsy) and insertion of iodoform gauze or of a rubber drainage
After 7 days the gauze is removed and the gap is kept open by means of a resin cone projecting into the surgical breach. The resin spur is shortened as the premolar erupts
The treatment is completed in about 3 months
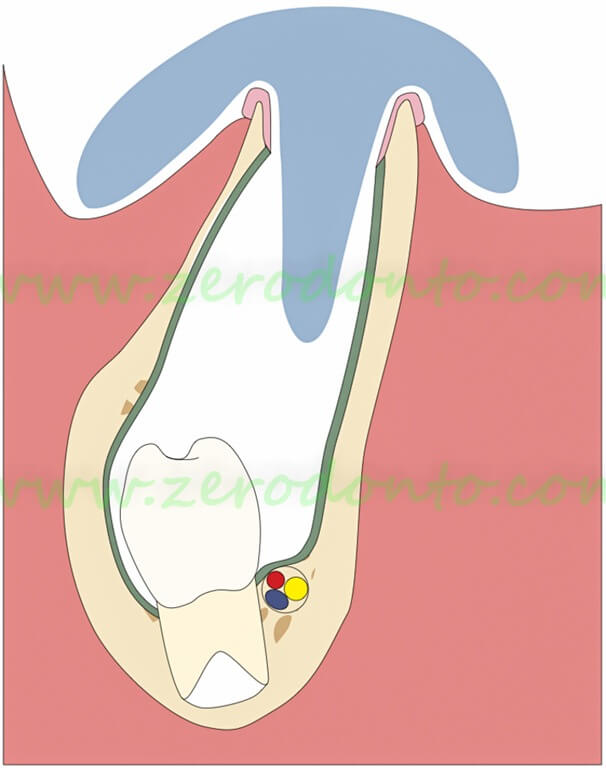
 Panoramic radiograph of a female 8 year old patient, showing a large radiolucent lesion with displacement of 31, 32, 33 and 34
Panoramic radiograph of a female 8 year old patient, showing a large radiolucent lesion with displacement of 31, 32, 33 and 34

 Clinical situation after the spontaneous loss of 83
Clinical situation after the spontaneous loss of 83

 Extraction of 84 and insertion of a gauze drainage after biopsy
Extraction of 84 and insertion of a gauze drainage after biopsy

 Drain removal 48 hours after surgery
Drain removal 48 hours after surgery

 Clinical and radiographic control after 3 months
Clinical and radiographic control after 3 months

 Clinical appearance after completion of the orthodontic treatment.
Clinical appearance after completion of the orthodontic treatment.
(orthodontic treatment by Dr. Maria Cristina Ceccarelli, Florence)
Germectomy of lower wisdom teeth
Early germectomies of lower wisdom teeth are no longer routine surgery. Interventions after full eruption of the second molars are usually preferred.
There is now a consensus about two facts:
– incisor crowding is not caused nor aggravated by the lower third molars
– second molars can be moved distally without removing the third molars.
the most frequent current indications for germectomy are:
– facilitating the recovery of an impacted second molar
– removing cystic lesions associated with the germs
– prevent damage due to inclusion of the third molar: damage to the second molar (caries and periodontal lesion)
– prevent damage associated with surgical removal of impacted third molars in adulthood, when the risk of complications increases, especially the neurological damage.
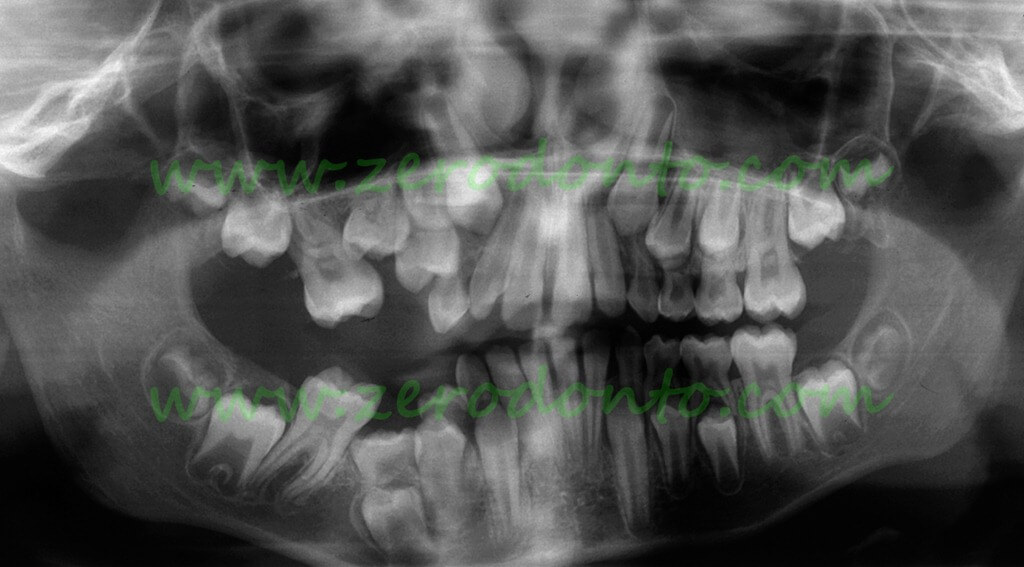
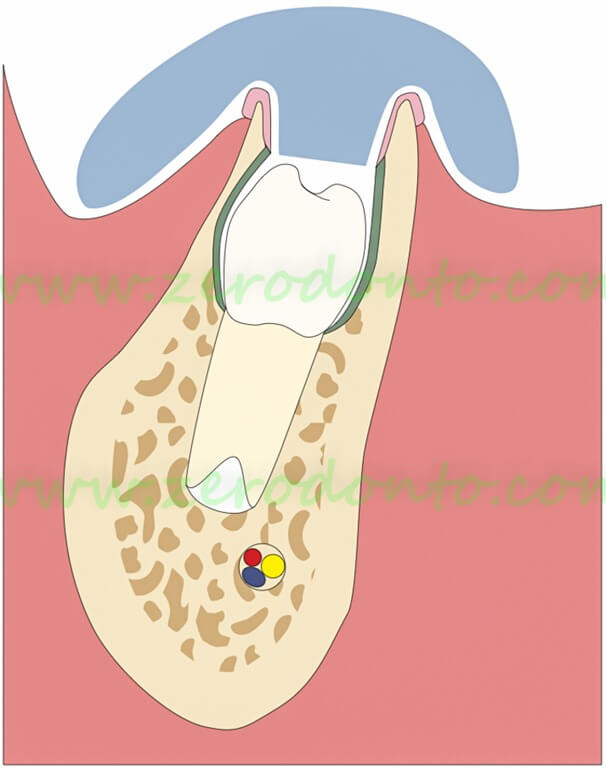
Impacted lower right second molar in a 15 year old male patient:
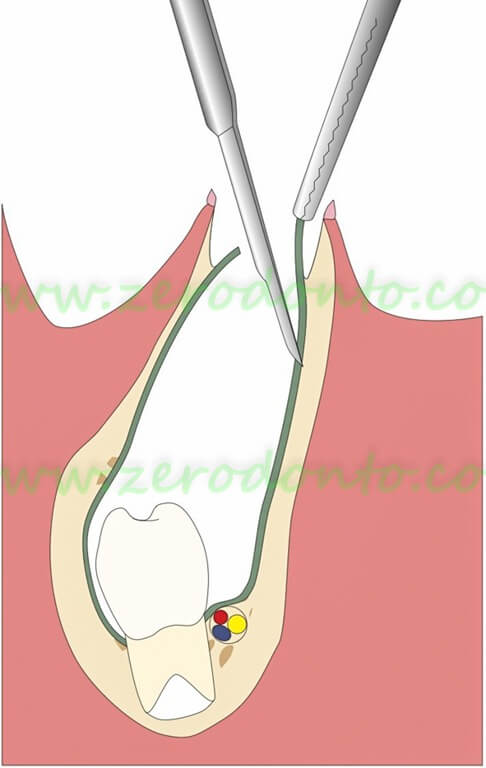
 The treatment of choice is the removal of the germ of 38 and in the orthodontic traction of the impacted second molar, that is exposed during the same surgery
The treatment of choice is the removal of the germ of 38 and in the orthodontic traction of the impacted second molar, that is exposed during the same surgery
 At the end of the orthodontic treatment, the second molar is recovered without damage to the first molar (orthodontic treatment by Dr. Fabio Favilli, Cagliari).
At the end of the orthodontic treatment, the second molar is recovered without damage to the first molar (orthodontic treatment by Dr. Fabio Favilli, Cagliari).
A delay in the treatment may result in serious consequences, up to the loss of all molars.
Impacted second molar observed at the age of 18 years:
 The prognosis of the first molar (36) is already uncertain, the chances of recovery of the second or third molar is illusory. Surgical removal of the second molar in such situations is difficult and dangerous
The prognosis of the first molar (36) is already uncertain, the chances of recovery of the second or third molar is illusory. Surgical removal of the second molar in such situations is difficult and dangerous
 The 3D imaging shows close relationships between the roots of the second molar and the alveolar canal. Furthermore, the roots of the second molar are considerably deep seated
The 3D imaging shows close relationships between the roots of the second molar and the alveolar canal. Furthermore, the roots of the second molar are considerably deep seated
 The first and second molars are visible in the arch. The access to the second molar is barred on the occlusal aspect
The first and second molars are visible in the arch. The access to the second molar is barred on the occlusal aspect
 After lifting of the usual triangular flap, the extraction of the third molar was completed without difficulty. The second molar is still hidden behind and below the crown of the first molar.
After lifting of the usual triangular flap, the extraction of the third molar was completed without difficulty. The second molar is still hidden behind and below the crown of the first molar.
 After further bone resection and fragmentation of the crown, it is finally possible to lift the rest of the second molar with a Friedman elevator
After further bone resection and fragmentation of the crown, it is finally possible to lift the rest of the second molar with a Friedman elevator
 Residual bone cavity partially visible after the extraction
Residual bone cavity partially visible after the extraction
All these difficulties could easily be avoided by timely diagnosis and treatment.
Case of retention of 37 in a 14 year old girl:

 The second molar is partially erupted
The second molar is partially erupted
The germectomy of the wisdom tooth is simple and minimally invasive in this development phase, and the application of an attack on the seventh is still easy.
 After placement of the bracket on the second molar, the fragmentation of the germ was initiated
After placement of the bracket on the second molar, the fragmentation of the germ was initiated
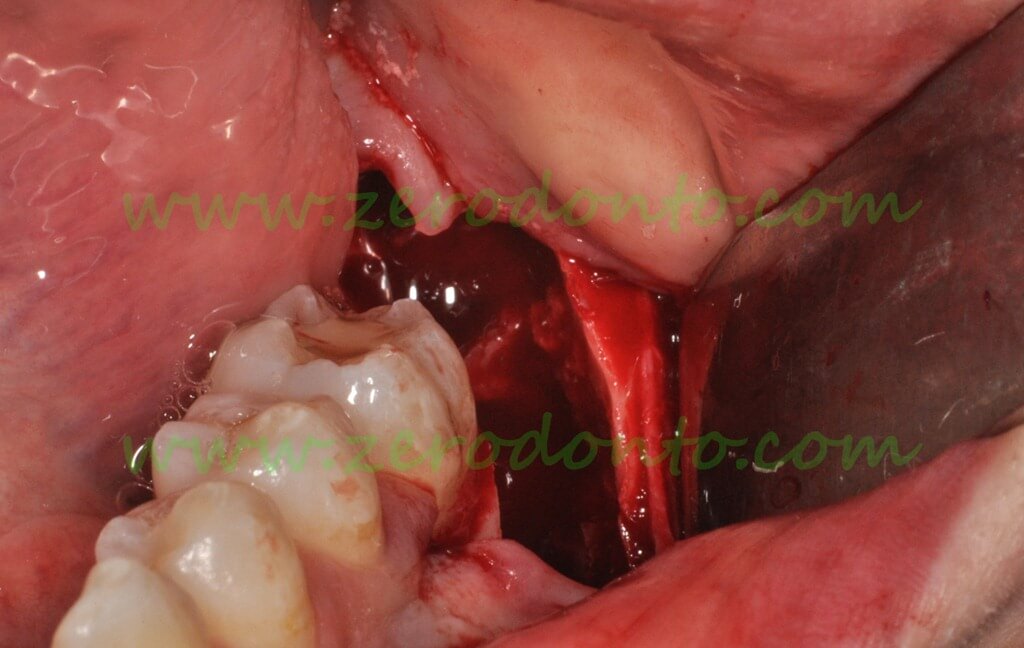
 The empty socket after removal of the germ of the third molar
The empty socket after removal of the germ of the third molar
The current international literature agrees that the neurological risk increases significantly (5-6 times) after the age of 25, while the expectancies of periodontal healing of the second molars worsen. In recent studies, the incidence of neurological damage after surgical extraction of lower wisdom teeth, ranges from 0.17% to 1.7% of extractions. The persistent damage are rare and vary from 0.04% to 0.36% (Robert et al., 2005).
The operative technique for germectomy after full eruption of the second molar does not differ substantially from the procedure used for the removal of wisdom teeth in adults, as described in a previous article .
Germectomy in a boy aged 13 years: surgical technique:
 OPT: the germ of 48 consists in the crown and a non-mineralized root bud (dental papilla)
OPT: the germ of 48 consists in the crown and a non-mineralized root bud (dental papilla)
Incision, elevation and retraction of the flap
Crown fragmentation and removal of fragments
REFERENCES
For more information on the treatment of cysts in children:
Barone R, Chiapasco M, Clauser C (1999) Chirurgia Orale. Le cisti dei mascellari. Manuale Atlante. Aggiornamenti, Firenze.
Clauser C, Zuccati G, Barone R, Villano et al (1994) Simplified surgical-orthodontic treatment of a dentigerous cyst. J Clin Orthod 28:103-106,1994.
Martinéz-Perez D, Varela-Morales M (2001) Conservative treatment of dentigerous cysts in children: A Report of 4 Cases. J Oral Maxillofac Surg 59:331-334.
Miyawaki S, Hyomoto M, Tsubouchi J et al (1999) Erupting speed and rate of angulation change of a cyst-associated mandibular second premolar after marsupialization of a dentigerous cyst. Am J Orthod Dentofac Orthop 116:578-584.
For more information on germectomies:
Becker A., Shpack., Shteyer A (1996) Attachment bonding to impacted teeth at the time of surgical exposure: Europ J Orthod 18:457-63.
For more information on neurological damage, see:
Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:377-83.
Bui CH, Seldin EB, Dodson T. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg 2003;61:1379-89.
Queral-Godoy E, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Incidence and evolution of inferior alveolar nerve lesions following lower third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:259-64.
Haug, RH, Perrott DH, Gonzalez, Talwar RM. The American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study. J Oral Maxillofac Surg 2005;63:1106-14.
Chuang SK, Perrott DH, Susarla SM, Dodson TB. Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg 2007;65:1685-92.
Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg 2010;39:320-6.
Robert RC, Bacchetti P, Pogrel MA. Frequency of trigeminal nerve injuries following third molar removal. J Oral Maxillofac Surg 2005;63:732-5.
For more information:
zerodonto@gmail.com
Roberto Barone
dottorbarone@gmail.com
CarloClauser
carlo.clauser@tin.it
Angelo Baleani
angelobaleani@live.it

