RESTORATION OF MAXILLARY CENTRAL INCISORS WITH MINIMALLY INVASIVE FELDSPATHIC CERAMIC VENEERS LAYERED ON REFRACTORY MODEL
CASE PRESENTATION
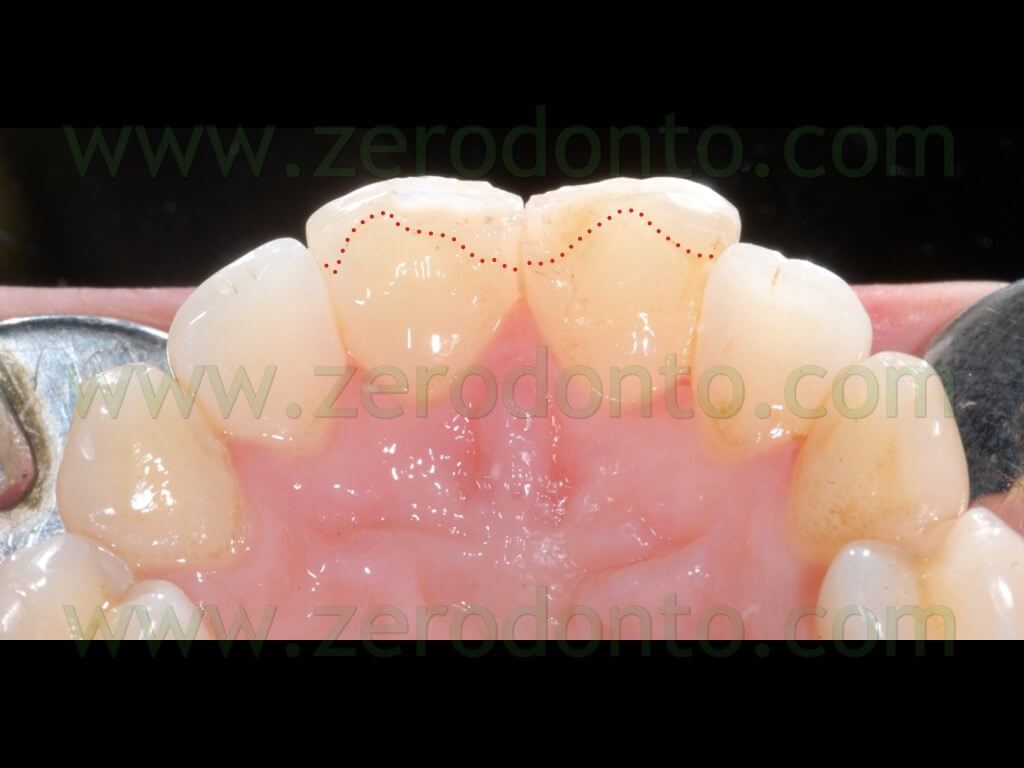
A 26 year-old female patientpresented with fractures of the incisal margins of 1.1 and 2.1.


The patient reported that she had already received composite restorations on such teeth twice but cohesive failures occurred in both occasions. Moreover, shecomplained of an unsatisfactory esthetic result.

The patient was in good general health, was a moderate smoker (about 10 cigarettes per day) and had acceptable oral hygiene. Dental crowding, malocclusion and abfractions were noticed but the patient did not accept any orthodontic treatment and asked just for the restoration of the maxillary central incisors.
The patient refused a new restoration with composite materials and, after achieving a written consent, it was decided to make two feldspathic porcelain veneers, in order to restore both function and esthetics with a minimally invasive adhesive approach.
In rest position, the visibility of the incisal margins of the teeth to be restored was considered satisfactory.

The previous composite restorations were identified under magnification and transillumination in order to remove the restorative materials selectively and project the best preparation design.

Due to mandibular dental crowding and type of fracture of the incisal margins, particular attention was given to the evaluation of overjet and overbite, in order to assess the availability of the functional spaces for the final restorations.


Diagnostic impressions were made and inter-maxillary relationship recorded by means of a centric occlusion wax, in order to mount the casts on an average values articulator.

The patient was subjected to professional oral hygiene and motivated to home oral care by a dental hygienist. Subsequently, in order to achieve the best esthetic result, the patient required home dental bleaching with 15% carbamide peroxide and potassium fluoride. Since the oxidizing agents may interfere with the polymerization of composite resins, the finalization of the case was delayed for two weeks.
CASE STUDY: FABRICATION OF MOCK-UP AND TEMPORARY RESTORATIONS
A working wax-up was made harmonizing the shapes and volumes of the teeth to be treated. The wax-up was made on the basis of the prosthodontist’s clinical indications and the patient’s requests and expectations.




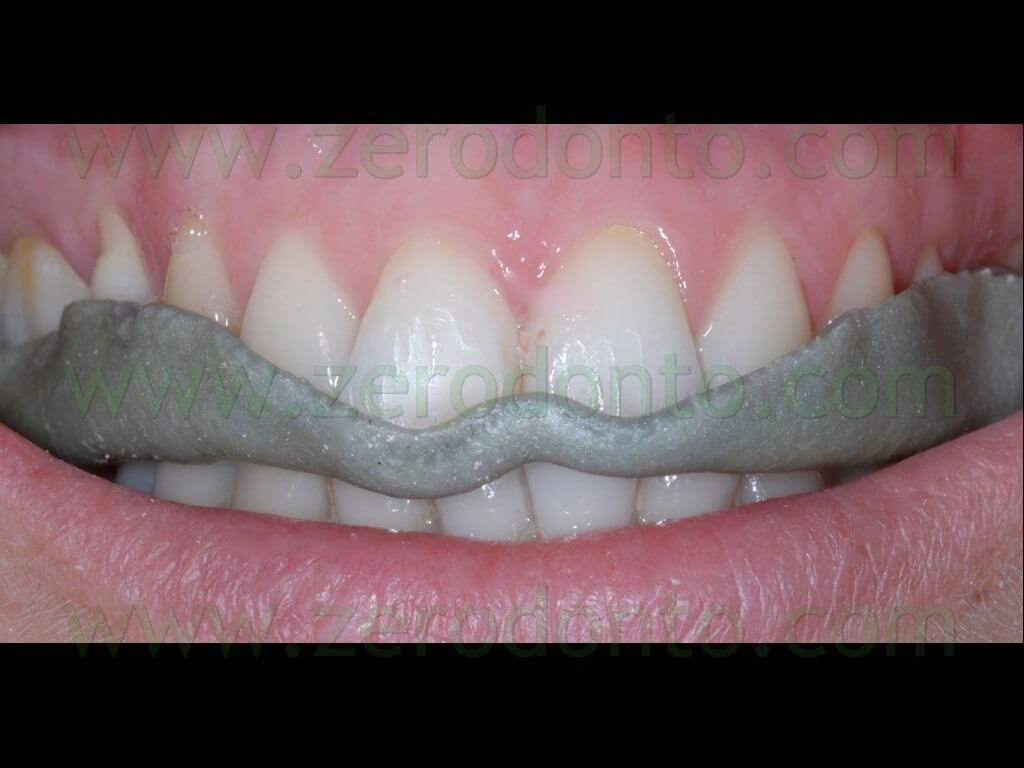
After a multidisciplinary approach aimed at optimizing the communication between the patient and the dental team, the wax-up was accepted. Consequently, the dental laboratory made an acrylic resin direct-indirect additive mock-up with an average thickness of 0.3 mm, converting the wax-up into resin.



As regards the mock-up, the two resin elements were kept together in order to increase the retention.




The mock-up was placed onto the patient’s unprepared teeth, so as to preview the final result, discuss it with the patient and make possible modifications.
Esthetic and phonetic tests were carried on, evaluating both the rest position and the smile line, thus permitting to modify the mock-up that resulted excessively extended at level of the incisal margins.




The mock-up was modified directly at the chair; the incisal areas to be shortened were marked with black ink and the changes made using a diamond bur mounted on a laboratory hand-piece.



The mock-up was tried in intra-orally again; any additive modification (e.g. undercuts to be passed) may be carried out using composite resins according with the conventional layering techniques. Once the desired pre-visualization was achieved, the shape of the mock-up was transferred and finished on the diagnostic die cast.




Although several techniques were reported in the literature to make provisional restorations for laminate veneers (e.g. direct, direct-indirect, indirect), it was decided to make indirect temporary acrylic resin laminates, in order to optimize the esthetic result.







Several silicone templates were made to check thickness during tooth preparation.


TOOTH PREPARATION
Before tooth preparation, periodontal probing was performed in order to identify the gingival biotype and choose the most appropriate retraction cords; the patient had a thick gingival biotype with an average probing depth of about 3 mm.


The thickness of the unprepared teeth was measured using a gauge, so as to know the amount of hard tissue removed at every stage of the preparation. However, it should be noted that this procedure is valid only with structurally intact teeth and it is rather laborious and imprecise, as it is not possible to keep unique anatomical landmarks during preparation.

A windowed silicone template was used to assess both the incisal and buccal preparation.


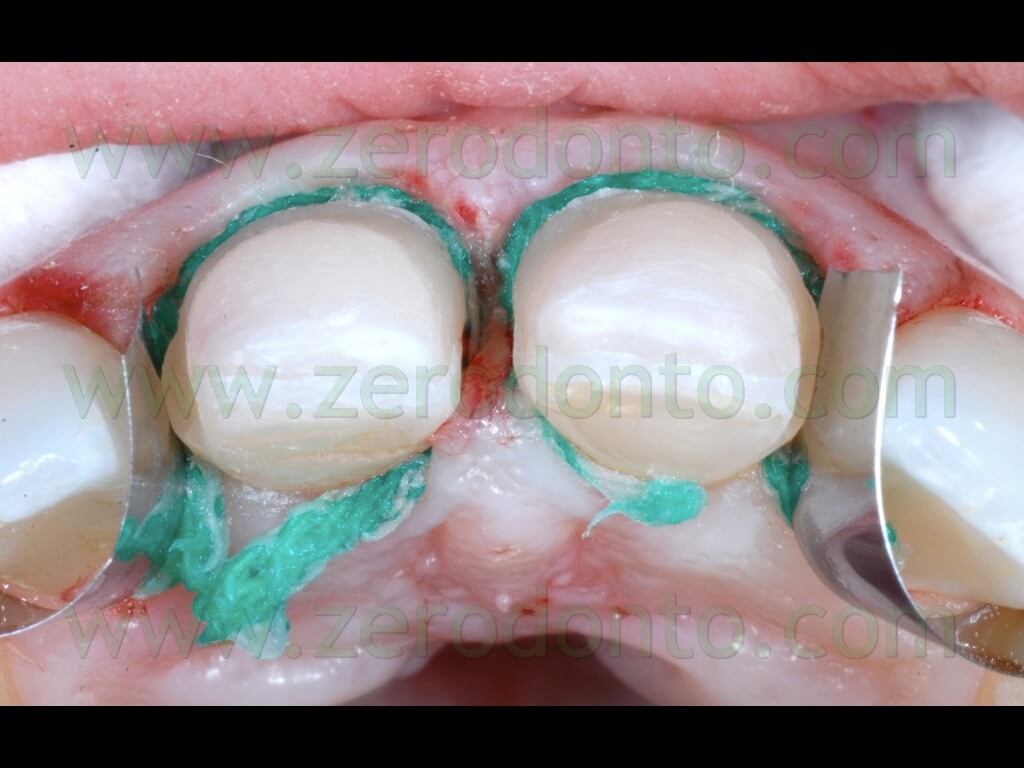
First, a single gingival retraction cord was used, in order to dislocate the marginal tissues apically and easily identify the cement-enamel junction (CEJ).

With the exception of particular clinical situations, the cervical finish line of porcelain veneers is placed 0.5 mm coronally to the CEJ, in order to optimize the adhesive cementation procedures on enamel. The maxillary lateral incisors were protected with metal matrixes.

The preparation for porcelain veneers should have a buccal thickness of about 0.5-0.7 mm, so as to remain within the enamel (based on mean anthropometric measurements) and to optimize the thickness of the ceramic. Both teeth were prepared with an incisal butt-joint. The preparation of the buccal surface of the maxillary central incisors was performed using two different techniques: the “dimple technique” on 11 and the “depth slot technique” on 21.

The “dimple technique” was performed making some dimples on the buccal surface with half of a spherical bur with a diameter of 1.2 mm, so as to obtain a series of wells 0.6 mm-deep in different areas of the tooth. Conversely, the “depth slot technique” was performed making two longitudinal guide grooves on the buccal surface, similarly to what is conventionally carried out for the preparation of an abutment; it is recommended to use half of a cylindrical bur with a diameter of 1.2 mm, so as to obtain grooves 0.6 mm-deep according to the above mentioned considerations. Guide pits and grooves can be highlighted with a pencil. In the opinion of the authors, the “dimple technique” is more laborious and less reliable, since freehand the maximum equator of the bur can be easily exceeded even under magnification, resulting in non homogeneous preparation guide dimples.
After preparing the buccal surface, the finish cervical area was prepared with a 0.3 mm-deep mini-chamfer. Then, the interproximal preparation was performed, placing the interdental margins palatally to the interdental contact areas, in order to avoid undesired pigmentations of the margins over time.

Since the previous composite restorations were infiltrated, they were completely removed. The silicone templates made on the working cast were sectioned in the bucco-palatal direction, so as to check the thickness of the preparation during all clinical stages.


The finishing procedures were carried out using diamond finishing burs mounted on a sonic hand-piece and by means of Arkansas stones mounted on a low-speed handpiece, under constant water irrigation. The preparation margins were further refined with interproximal metal abrasive strips.



Once the preparations were completed, enamel was evident on the whole periphery of both teeth, providing a good substrate for the adhesive cementation. As previously described, the prepared teeth were measured using a thickness gauge, in order to perform a quantitative measurement of the mineralized tissues removed.

A final check was made with the silicone templates, in order to verify the congruence of the geometry of the preparation with the shape and volume of the mock-up.






IMPRESSION MAKING AND TEMPORARIZATION
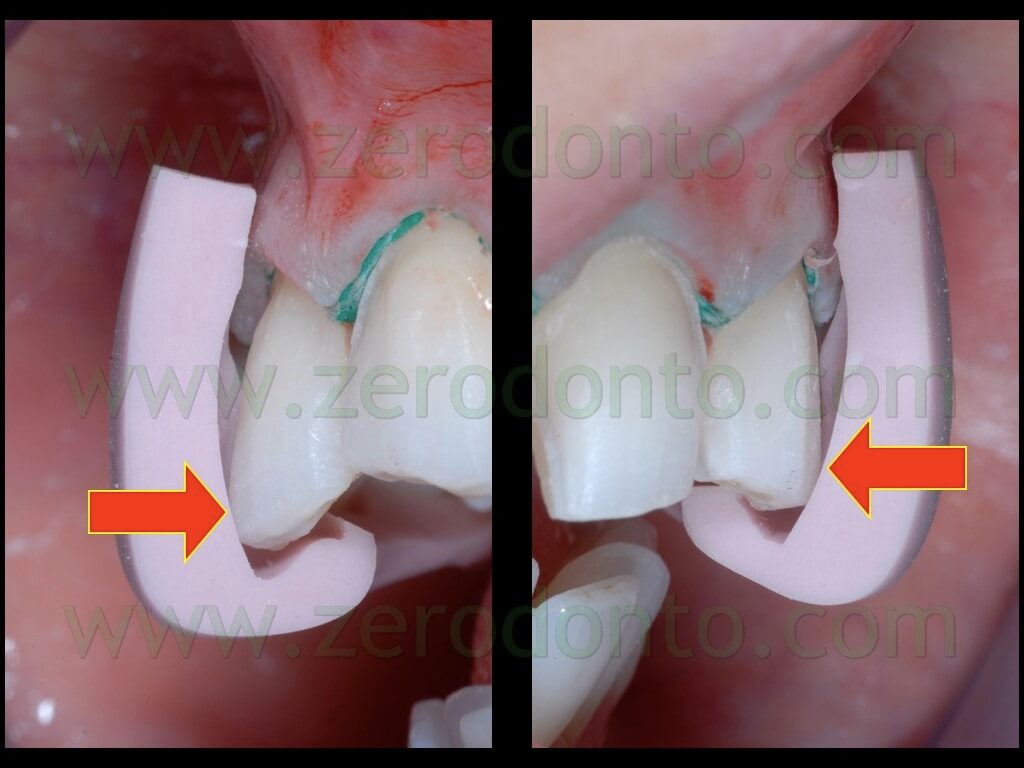
A moderate acute suffering of the interproximal papilla due to the single gingival retraction cord was noticed at the stereomicroscope. Before making the impression, it was substituted with two smaller cords, in order to avoid any possible damage to soft tissues. Moreover, two metal matrixes were positioned in the contact areas with the lateral incisors, so as to optimize the impression making.

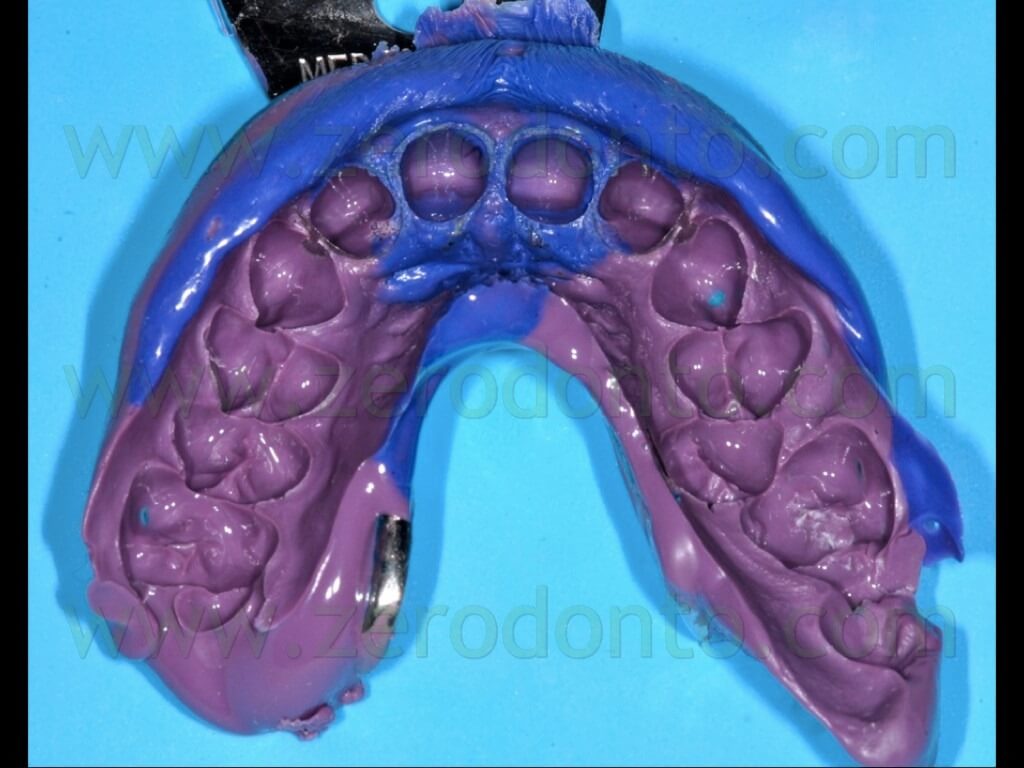
A one-step/two-phase impression with low and medium viscosity polyethers was made. The metal matrixes were kept in the impression material.
After impression making, the retraction cords were removed and the gingival sulci were inspected and cleansed. Subsequently, the color of the adjacent teeth was recorded; particular attention was paid to the over-saturation determined by teeth bleaching.

The indirect temporary restorations were relined intra-orally using acrylic self-polymerizing resin. Any misfit due to micro-movements of the restorations were corrected with a further fluid relining, particularly at the level of the cervical finish line.



The temporary veneers were finished and polished. Then, they were mechanically blocked on the prepared teeth by means of limited undercuts at level of the interproximal areas. No temporary luting agents were used, in order not to contaminate dental substrates to be used for the final adhesive cementation.


The contact points in centric occlusion and during the non-axial movements were carefully checked and balanced.



FABRICATION OF THE PORCELAIN VENEERS
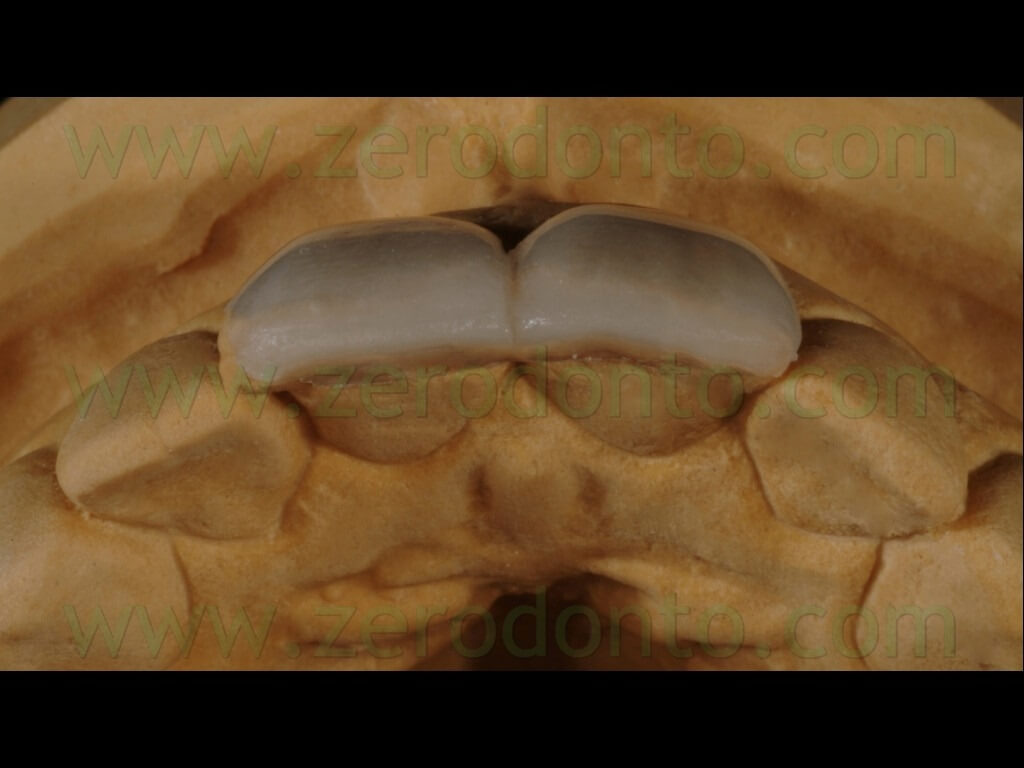
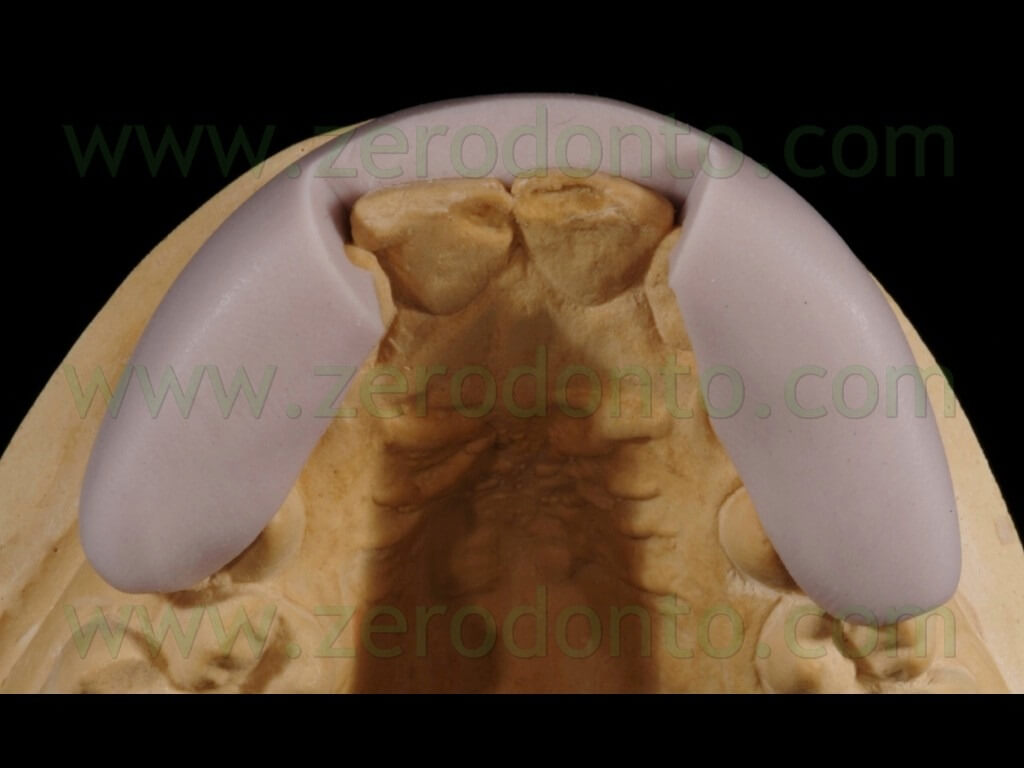
The final restorations were made using feldspathic ceramic stratified on a refractory model.
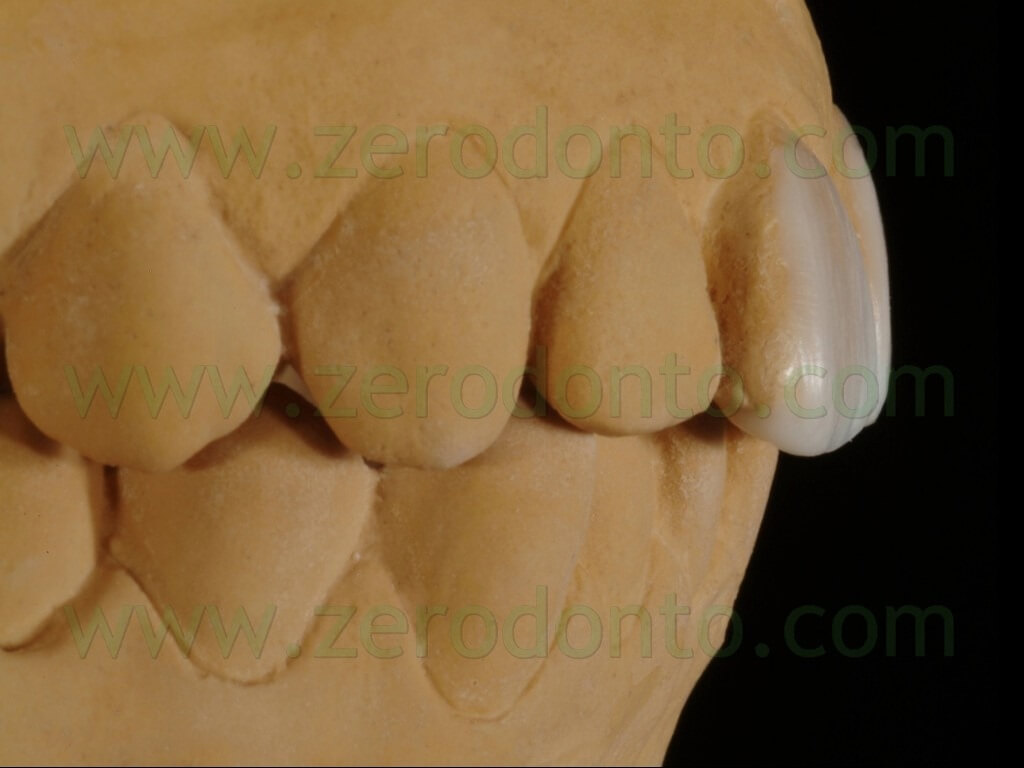
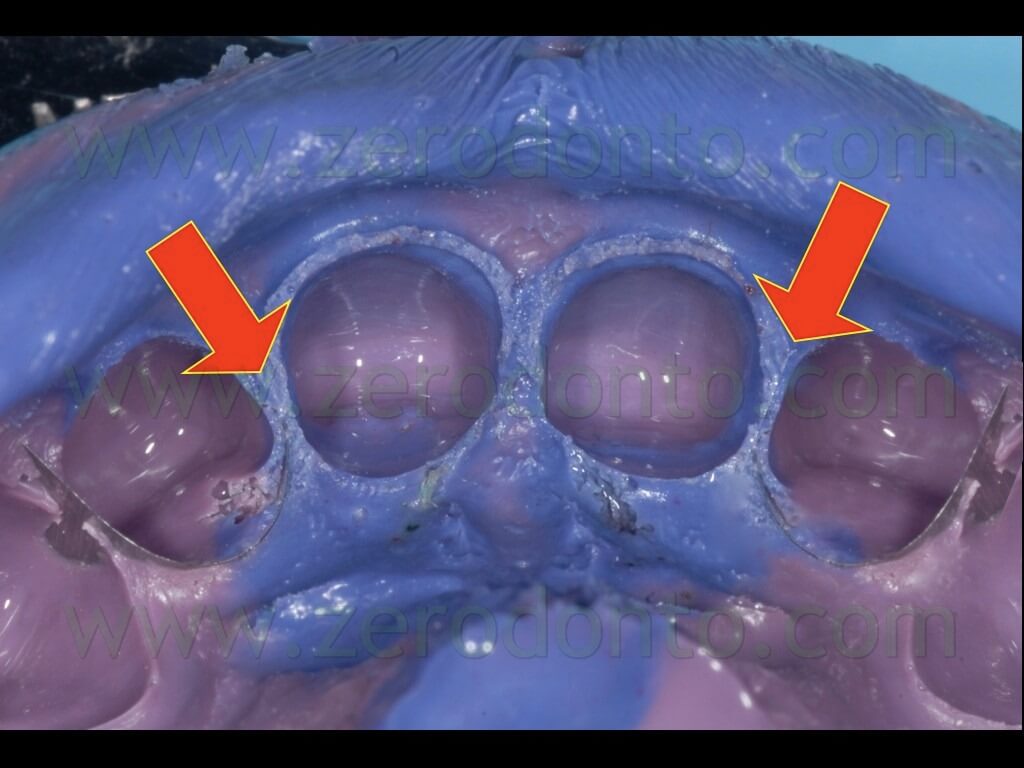
The impression was poured with extra-hard class IV plaster and a first model (sectorial model) was fabricated.

Then, the master models of the preparations were set in the alveolar model by means of a silicon check made on the not segmented cast.


Subsequently, the refractory abutments were carefully placed in the assembled working model.


A first layer of stable ceramic was fired, achieving precise and intimate contact with the underlying surface.

Subsequently, the morphological and chromatic structures of dentin, incisal plate and incisal effects were realized.


After completing the firing of feldspathic ceramic, particular attention was dedicated to the realization of surface texture; then, the veneers were finished and polished.



Finally, the veneers were separated and accurately set on the sectorial model, in order to check the contact areas with adjacent teeth. Particular attention was paid to the inspection of the intaglio surfaces of the veneers, in order to verify the absence of voids and marginal integrity.




The thickness of the veneers (0.5-0.7 mm) was measured using a thickness gauge at level of cervical, middle and incisal third.

ADHESIVE CEMENTATION
In order to optimize the adhesive procedures, no more than 7-10 days should pass between tooth preparation and cementation, avoiding dental substrate contamination. In the present case, the adhesive cementation was performed 8 days after tooth preparation, after checking the gingival tissues health.


The temporary restorations were removed; the prepared surfaces were cleansed and polished with pumice paste and inspected under stereomicroscope.


The correct color matching was checked at first trying the veneers intra-orally without any intermediate medium but by simple wetting.

Subsequently, two different colors of try-in pastes were tested (white on 11 and transparent on 21), so as to assess the light translucency, refraction and reflection effects; it was decided to use the transparent mass. These water-soluble pastes were removed by rinsing with water and drying with air.



The veneers, previously etched in the dental laboratory with 10% hydrofluoric acid, were cleanesd and conditioned with 37% orthophosphoric acid, rinsed and silanized.

The adhesive cementation was performed using a dedicated light-curing resin cement.

The adhesive cementation was carried out according to the conventional adhesive procedures under rubber dam.





The cement excesses were removed after gelling the resin cement; then, the polymerization was completed.






Interproximal areas were finished and polished with fine-grained abrasive strips.

After cementation, the gingival sulci were cleansed and inspected with a teflon curette, so as not to damage the restoration margins.

The correct placement of the veneers was checked by means of standardized periapical radiographs.

FOLLOW-UP
At the 7-day follow-up, the veneers were well integrated and the periodontal tissues in health. The occlusal contacts were checked and balanced.












At 3- and 12-month recall appointments, the stereomicroscope showed good fit of the restorations and confirmed the high biomimetic potential of veneers.








Pre-operative and post-operative pictures.
BEFORE:

AFTER:

BEFORE:

AFTER:

REFERENCES
1. Beier US, Kapferer I, Dumfahrt H. Clinical long-term evaluation and failure characteristics of 1,335 all-ceramic restorations. Int J Prosthodont. 2012 Jan-Feb;25(1):70-8.
2. Beier US, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont. 2012 Jan-Feb;25(1):79-85.
3. Sorrentino R, Apicella D, Riccio C, Gherlone E, Zarone F, Aversa R, Garcia-Godoy F, Ferrari M, Apicella A. Nonlinear visco-elastic finite element analysis of different porcelain veneers configuration. J Biomed Mater Res B Appl Biomater. 2009 Nov;91(2):727-36.
For information:
zerodonto@gmail.com

