Introduction
In the last decade, a growing interest for more friendly, patient oriented surgery have urged clinical investigators to focus their interest in the development of less invasive approaches. Surgical procedures in medicine and in dentistry have undergone radical changes to reduce invasivity; in parallel novel instruments and materials have been developed for the inevitable evolution of the surgical armamentarium (Cortellini 2012).
The field of periodontal surgery have been enriched with this peculiar and innovative approach rather recently (Harrel and Rees 1995). They proposed the “Minimally Invasive Surgery (MIS)” with the aim to produce minimal wounds, minimal flap reflection and gentle handling of the soft and hard tissues (Harrel and Nunn 2001, Harrel et al. 2005). Cortellini and Tonetti (2007a) proposed the Minimally Invasive Surgical Technique (MIST) to stress the aspects of wound and blood clot stability and primary wound closure for blood-clot protection. These concepts were further enforced with the Modified Minimally Invasive Surgical Technique (M-MIST, Cortellini & Tonetti 2009) that, additionally, incorporated the concept of space provision for regeneration. Minimally invasive surgery is a term that describes the application of very precise and delicate surgical procedures that require the use of magnifying devices, like operating microscopes or magnifying lenses, and microsurgical instruments and materials. Cortellini & Tonetti (2001, 2005) proposed the use of an operative microscope in periodontal regenerative surgery, reporting an increased capacity to manipulate the soft tissues that resulted in an improved potential for primary closure of the wound from an average 70% of the cases obtained with regular surgery to an excellent 92% obtained with microsurgery.
Minimally Invasive Surgical Techniques
Two different minimally invasive techniques have been proposed: 1) procedures that include the elevation of a tiny buccal flap as well as the elevation of the interdental papilla and of the palatal flap and 2) techniques that are limited to the elevation of the buccal flap.
These procedures can be applied for the treatment of shallow and deep intrabony defects (up to the apical third of the root surface).
Diagnosis of intrabony defects
The diagnosis of the intrabony defect is based on periodontal probing. The difference of attachment level between two interproximal surfaces represents the intrabony component of the defect. If the mesial surface of a tooth has an attachment level of 10 mm and the distal surface of the neighbouring tooth has an attachment level of 4 mm, the depth of the intrabony component is 6 mm.


The diagnosis can be confirmed with a periapical radiograph that provides relevant information about the morphology of both the defect and the root. However, in many instances, the radiograph underestimates the real depth of the defect.

Pre-operative patient and site preparation
A critical prerequisite to periodontal regeneration is the control of periodontal disease. The patient should present with very low levels of plaque and inflammation as the result of a successful cause-related therapy. In addition the patient should not smoke or at least smoke less than 10 cigarettes per day. Systemic diseases, like diabetes, have to be under control. Intraoral prophylaxis with a low-speed rubber cup and prophylaxis paste should be performed immediately before surgery; in addition, the patient should rinse the mouth with 1% chlorexidine for 1 minute.
Anesthesia
Local anesthesia with carbocaine and adrenaline 1:100.000 has to be injected in the mucosal tissues. Attention has to be paid not to infiltrate the gingival margin and, in particular, the defect-associated interdental papilla in order to avoid possible side effects in the early healing phase due to over-infiltration of these tissues.
Minimally Invasive Surgical Technique (MIST)
The Minimally Invasive Surgical Technique (MIST, Cortellini and Tonetti 2007a, 2007b) is based on the elevation of very short buccal and lingual flaps that include the defect-associated interdental papilla; the papilla is dissected with two different approaches according to the width of the interdental space. In narrow interdental spaces a diagonal cut is selected, as described in the Simplified Papilla Preservation Flap (SPPF, Cortellini et al. 1999); conversely, a horizontal cut is performed in wide interdental spaces, according to the Modified Papilla Preservation Technique (MPPT, Cortellini et al. 1995a, 1995b). The buccal and the lingual intrasulcular incisions are restricted to the teeth neighbouring the defect; the buccal and lingual full thickness flaps are therefore elevated with minimal mesio-distal and corono-apical extensions, the aim being to expose the coronal edge of the residual bone crest. In most of the cases the reflection of the buccal flap does not involve the muco-gingival line. Scaling and root planing are performed by means of mini-curettes and sonic/ultrasonic instruments.
Once thoroughly cleaned, the defect can be treated with different regenerative materials, such as amelogenins, growth factors, autologous bone grafts, allograft materials or combinations thereof. The use of amelogenins should also include the application of EDTA for 2 minutes on the dried root surface; the root surface is then thoroughly washed and gently air-dried to apply amelogenins.
The suture technique is based on the application of a single modified internal mattress suture (the use of a 6-0 Gore suture is suggested) in order to provide a primary intention closure of the interdental papilla. The primary intention seal can be improved applying passing sutures (the use of 6-0 or 7-0 monofilaments is suggested), when needed.
The MIST can be used also to treat multiple intrabony defects on adjacent teeth (Cortellini et al. 2008). The technique requires a larger mesio-distal extension of the flap to include all the defects-associated teeth. Although the mesio-distal extension is increased, the corono-apical elevation of the full thickness buccal flap is minimal, according to the previously reported principles.
Modified Minimally Invasive Surgical Technique (M-MIST)
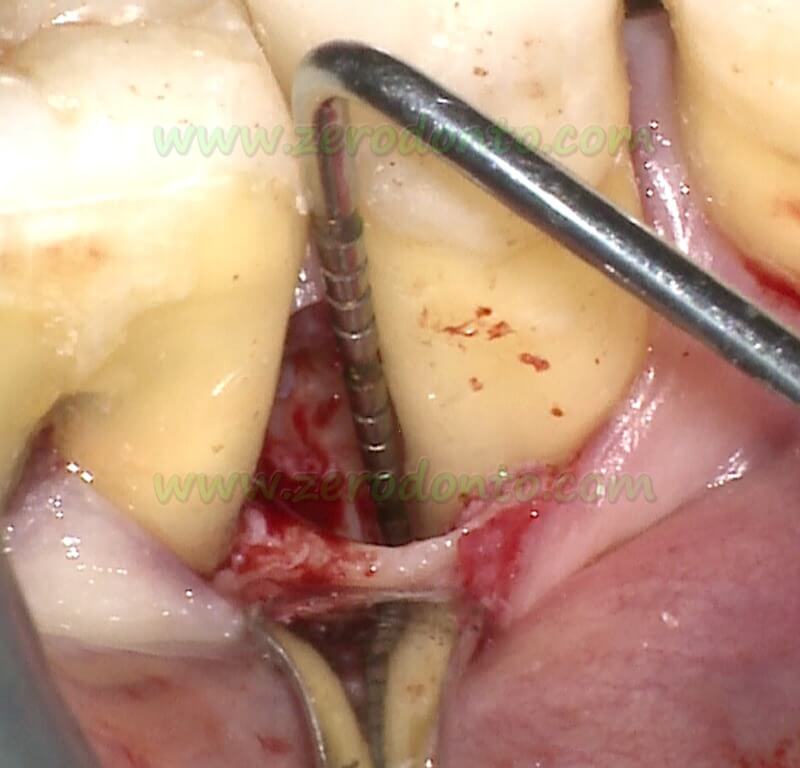
More recently, a Modified Minimally Invasive Surgical Technique (M-MIST) has been proposed (Cortellini and Tonetti 2009). The overall idea of the M-MIST is to provide a very small interdental access to the defect only from the buccal side. The triangular buccal flap is minimally elevated in order to expose the residual buccal bone crest. According to the width of the interproximal space, the incision of the buccal aspect of the papilla follows the same principles described in the MIST approach. Once the buccal flap has been elevated, the supracrestal interdental tissue is dissected from the granulation tissue by means of a mini-blade. The interdental papilla is not detached from the residual interdental bone crest and supracrestal fibres, and the palatal flap is not elevated. The granulation tissue is further dissected from the bone with the mini-blade and then removed by means of mini-curettes. Then, the root surface is thoroughly scaled and planed by the combined action of mini-curettes and sonic/ultrasonic instruments. Special care has to be paid in order to avoid any trauma to the supracrestal fibres of the defect-associated papilla.
All the reported clinical steps are performed through the small buccal “surgical window” and require magnifying devices and optimal illumination of the surgical field, such as an operative microscope or magnifying lenses. The primary closure of the surgical wound is achieved using a modified internal mattress suture and eventually the application of additional passing sutures, as described for the MIST technique.
Technical implications and limitations
The two reported minimally invasive approaches can be used for the treatment of many intrabony defects but, obviously, present some limitations. Complex and wide defects involving 3 or 4 surfaces of a tooth and reaching the apical third of the root or even extending to the apex have to be approached with the elevation of large flaps, such as the Modified Papilla Preservation Technique (MPPT) or the Simplified Papilla Preservation Flap (SPPF, Cortellini et al. 1995, 1999). Conversely, defects involving one or two sides of a tooth can be approached using the minimally invasive techniques. The MIST (Cortellini and Tonetti 2007a, 2007b) allows for a direct buccal and lingual access to the intrabony defect, while the M-MIST (Cortellini and Tonetti 2009) limits the access to the defect through the small buccal flap. The main problems encountered applying a minimally invasive approach are limitations in visibility and management of the surgical field, which becomes even more critical in the M-MIST. The main problem with the M-MIST approach is the access to the root surface in cases presenting with a deep palatal extension of the defect not cleansable through the buccal window. (Cortellini and Tonetti 2009). In these cases, it is suggested to elevate the interdental papilla performing a MIST approach. The minimally invasive procedures take great advantage by the use of an operative microscope that allows an optimal adaptation of the magnifying factor on the basis of the surgical needs and is supplied with an illumination system coaxial with the lens, resulting in an ideal illumination of the operative area.

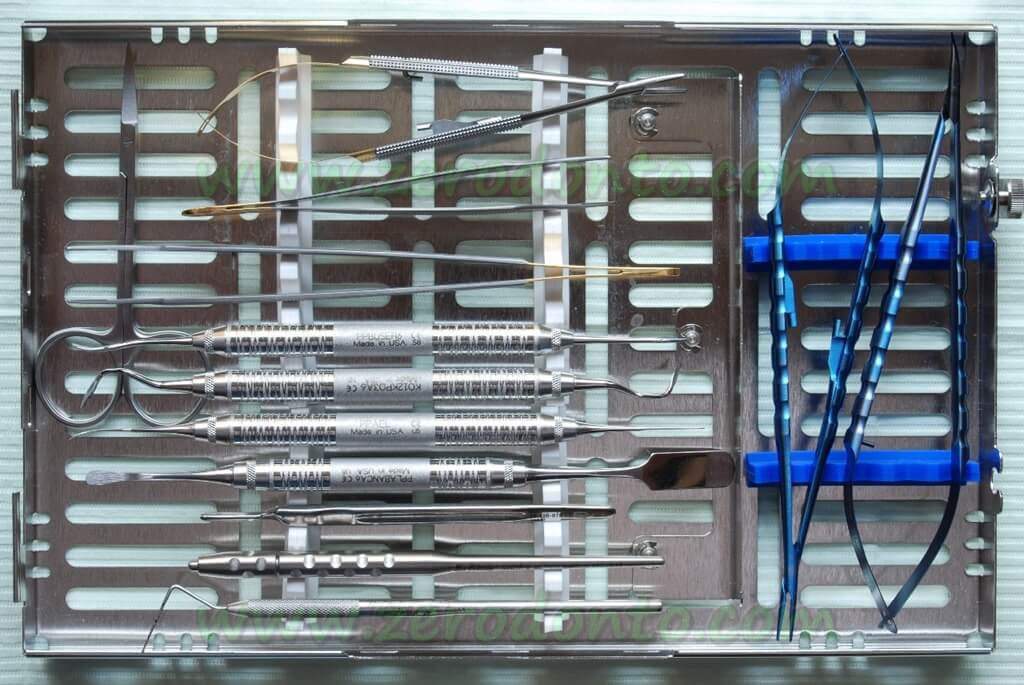
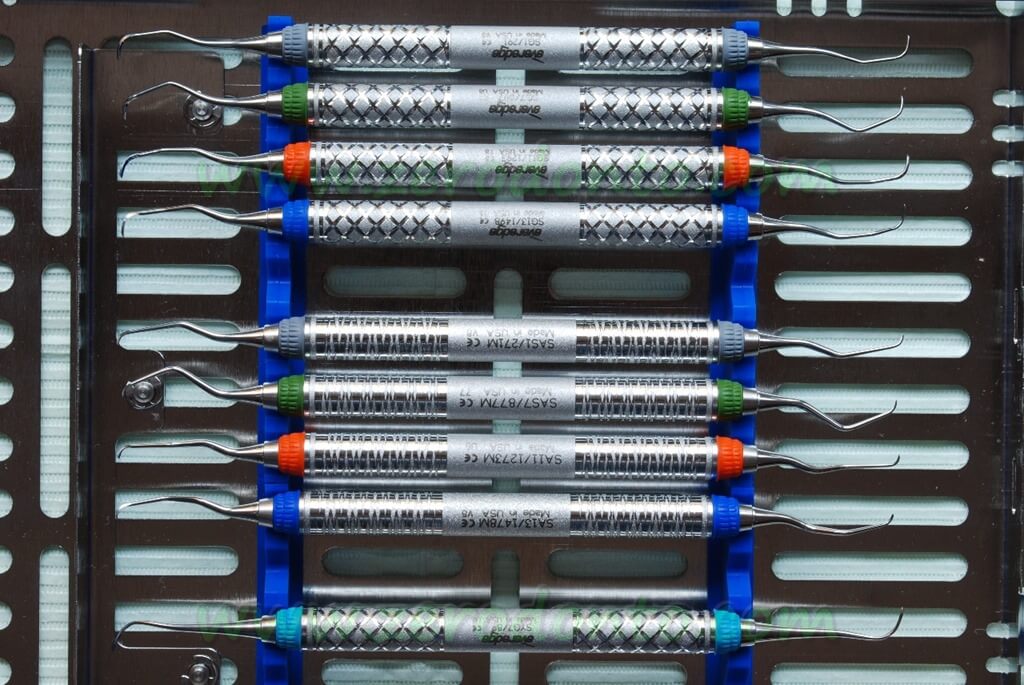
In addition, it is mandatory to implement the surgical tray with microsurgical instruments and materials, like tiny periosteal elevators, micro-pliers, micro-blades, mini-curettes, small scissors and needle holders. Small 6-0, 7-0 or even 8-0 non-resorbable sutures should also be adopted.
Post-operative healing
The patient is dismissed with the following prescriptions:
- One 600 mg ibuprofen tablet immediately after surgery and one after 8 hours; further doses of pain-killer can be taken in case of need;
- 100 mg doxycycline 2 times per day for 1 week;
- 0.12% chlorhexidine mouth-rinse for 1 minute 3 times per day; chlorhexidine mouth-rinse will be continued until when the patient will resume regular mechanical tooth cleaning (usually for 5 weeks);
- no mechanical oral hygiene for 1 week;
- soft food intake for 1 week.
1 week after surgery:
- removal of the sutures;
- oral prophylaxis with chlorhexidine gel;
- adoption of a soft toothbrush in the regenerated area;
- soft food intake.
3 weeks after surgery:
- oral prophylaxis with tooth-pastes;
- adoption of under-dimensioned interdental brush or floss in the regenerated area;
- medium consistency food intake.
5 weeks after surgery:
- oral prophylaxis with tooth-pastes;
- resume regular tooth-brushing and interdental cleaning;
- regular food intake.
Post-operative healing: complications
The development of minimally invasive surgery has greatly reduced the amount of complications and side effects in the post-operative period. In the immediate post-operative period, the main problem is represented by the primary closure of the surgical wound. Following traditional regenerative periodontal surgery based on papilla preservation flaps, Cortellini and Tonetti (2000) reported 70% of primary closure of the surgical wound. In other words, 30% of the cases showed a failure of the surgical wound that resulted in a reduced clinical improvement of the treated area. Using the MIST, the primary closure of the flap was achieved in 100% of cases and maintained in 95% of the cases during the early healing phase (Cortellini and Tonetti 2007a, 2007b). When multiple defects were treated, primary closure was maintained in 100% of the cases (Cortellini et al. 2008). Post-operative complications, such as oedema and root hypersensitivity, were reported in very few cases (Cortellini and Tonetti 2007a, 2007b, Cortellini et al. 2008). Using the M-MIST in combination with Enamel Matrix Derivative (EMD, Cortellini and Tonetti 2009), the primary closure of the flap was achieved and maintained in 100% of the treated cases. In a controlled clinical trial (Cortellini and Tonetti 2011), a surgical site treated with M-MIST in combination with EMD and BioOss presented a slight discontinuity of the surgical interdental wound after 1 week. In none of the treated cases oedema, hematoma, or suppuration were observed (Cortellini and Tonetti 2009, 2011).
Patients’ surgical and post-operative morbidity
The clinical impact of the minimally invasive procedures on patients is reportedly extremely friendly. In a clinical study, none of the patients treated with MIST and EMD showed intraoperative pain or discomfort and only 30% of them reported some post-operative pain (Cortellini and Tonetti 2007b). The patients reporting pain described it as very moderate; pain disappeared within 26±17 hours, on average. Home consumption of painkillers was 1±2 tablets, on average; 23 patients did not take any painkiller.
In a further study on the MIST and EMD (Cortellini et al. 2008), 14 patients reported no post-operative pain while 6 patients referred a very light pain. In these patients, pain disappeared after 21±5 hours, on average. Home intake of painkillers was 0.9±1 tablets, on average; 9 patients did not take any painkiller.
In a study on M-MIST and EMD (Cortellini and Tonetti 2009), no patient reported intra- or post-operative pain; 3 patients referred a very slight discomfort in the first 2 days after surgery. Fourteen out of 15 subjects described the first postoperative week as uneventful, reporting that they had no feeling of having been surgically treated after the second post-operative day.
In a controlled study on the M-MIST alone or in combination with EMD or EMD and BioOss (Cortellini and Tonetti 2011) none of the patients reported intra and post-operative pain. Slight post-operative discomfort was reported by three patients of the M-MIST group (average VAS value 10.7±2.1), by two patients of the M-MIST EMD group (VAS 11.5±0.7) and by four patients of the M-MIST EMD/BMDX one (VAS 12.3 ±3.1). Few patients needed pain control medications: three patients from the control group (average number of tablets 0.4±0.7, maximum 2), four patients from the EMD group (average 0.3±0.6, maximum 2), and four patients from the EMD/BMDX group (average 0.5±1, maximum 3).
Conclusions
Minimally invasive surgery has to be considered a true reality in periodontal regenerative surgery. Several clinical trials have shown its efficacy and predictability in the treatment of intrabony defects. The clinical efficacy is consistently associated with a very low morbidity both during surgery and in the post-operative healing period. The minimally invasive surgical procedures require a specific training and the use of dedicated instruments and materials to be successfully applied to the treatment of intrabony defects.
References
1. Cortellini P, Pini-Prato G & Tonetti M. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol 1995a: 66: 261-266.
2. Cortellini P, Pini-Prato G & Tonetti M. Periodontal regeneration of human infrabony defects with titanium reinforced membranes. A controlled clinical trial. J Periodontol 1995b: 66: 797-803.
3. Cortellini P, Pini-Prato G & Tonetti M. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Rest Dent 1999: 19: 589-599.
4. Cortellini P, Tonetti MS. Focus on intrabony defects: guided tissue regeneration (GTR). Periodontology 2000. 2000: 22: 104-132.
5. Cortellini P, Tonetti MS. Microsurgical approach to periodontal regeneration. Initial evaluation in a case cohort. J Periodontol 2001: 72: 559-569.
6. Cortellini P, Tonetti MS. Clinical performance of a regenerative strategy for intrabony defects: scientific evidence and clinical experience. J Periodontol 2005: 76: 341-50.
7. Cortellini P, Tonetti MS. A Minimally Invasive Surgical Technique (MIST) with Enamel Matrix Derivate in the Regenerative Treatment of Intrabony Defects: A Novel Approach to Limit Morbidity. J Clin Periodontol 2007a: 34: 87-93
8. Cortellini P, Tonetti MS. Minimally Invasive Surgical Technique (M.I.S.T.) and Enamel Matrix Derivative (EMD) in Intrabony Defects. (I) Clinical Outcomes and Intra-operative and Post-operative Morbidity. J Clin Periodontol 2007b: 34: 1082-1088.
9. Cortellini P, M Nieri, GP Pini Prato, Tonetti MS. Single minimally invasive surgical technique (MIST) with enamel matrix derivative (EMD) to treat multiple adjacent intrabony defects. Clinical outcomes and patient morbidity. J Clin Periodontol 2008: 35: 605-613.
10. Cortellini P, Tonetti MS. Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J Clin Periodontol 2009: 36: 157–163.
11. Cortellini P, Tonetti MS: Clinical and radiographic outcomes of the modified minimally invasive surgical technique with and without regenerative materials: a randomized- controlled trial in intra-bony defects. J Clin Peridontol 2011: 38: 365–373.
12. Cortellini P, Stalpers G, Mollo A, Tonetti MS. Periodontal regeneration versus extraction and prosthetic replacement of teeth severely compromised by attachment loss to the apex: 5-year results of an ongoing randomized clinical trial. J Clin Periodontol 2011: 38: 915–924.
13. Cortellini P, Tonetti MS , Pini Prato G. The Partly Epithelialized Free Gingival Graft (PE-FGG) at Lower Incisors. A Pilot Study with Implications for Alignment of the Muco-gingival Junction. J Clin Periodontol 2012: 39:674-680.
14. Cortellini P. Minimally invasive surgical techniques in periodontal regeneration. J Evid Based Dent Pract. 2012;12:89-100.
15. Harrel SK, Rees TD Granulation tissue removal in routine and minimally invasive surgical procedures. Compendium of Continuing Education Dentistry. 1995: 16: 960-967.
16. Harrel TK, Nunn ME Longitudinal comparison of the periodontal status of patients with moderate to severe periodontal disease receiving no treatment, non-surgical treatment, and surgical treatment utilizing individual sites for analysis. J Periodontol 2001: 72: 1509-1519.
17. Harrel SK, Wilson Jr TG, Nunn ME Prospective assessment of the use of enamel matrix proteins with minimally invasive surgery. J Periodontol 2005: 76: 380-384.
Curriculum Vitae Dr. Pierpaolo Cortellini:
Dr. Pierpaolo Cortellini received his MD from the University of Florence (Italy) in 1980, and his DDS in 1984 from the University of Siena (Italy). Dr Cortellini is the Secretery of the Accademia Toscana di Ricerca Odontostomatologica, Firenze Italy, and Board Member of the European Research Group in Periodontology, Berne (CH). He is active Member and Past President of the Italian Society of Periodontology and Past President of the European Federation of Periodontology. Promoter of “Project Periodontal Diagnosis” and Coordinator of the 5 “National Educational Projects” from SIdP, he was Scientific Chairman of Europerio 6. He runs a private practice in Florence (Italy), with services limited to periodontics. Dr. Cortellini is involved in clinical research in periodontology since 1982, with special emphasis to periodontal regeneration, aesthetics, and diagnosis. Dr. Cortellini lectures extensively on a national and international level; he is referee of scientific journals in the field of periodontology, and is the author of more than 100 original publications in scientific journals.
For info & Courses:
Advanced Practical Course on Periodontal Regeneration
October 10 – 12, 2013 – Florence, Italy
Speakers: Pierpaolo Cortellini & Maurizio Tonetti
corsi@tangramodis.it
www.tangramodis.it/en
Private Office
Via C Botta 16
50136 Firenze, Italia
Tel + 39 055 243950
Fax + 39 055 2478031
info@ studiocortellini.it
www.studiocortellini.it
TangramOdis srl
Via C Botta 16
50136 Firenze, Italia
corsi@tangramodis.it
www.tangramodis.it
ATRO (Accademia Toscana di Ricerca Odontostomatologica) Firenze, Italia
ERGOPERIO (European Research Group on Periodontology) Berna, Svizzera

